Twogether Updates
Discontinuation of the Attendant Compensation Rate Enhancement Program and Rate Increases for Attendant Services
June 30th, 2025
HHSC Publishes IL-2025-11
HHSC will propose increased rates for identified attendant services and discontinue the Attendant Compensation Rate Enhancement program, effective Sept. 1, 2025.
These changes are pursuant to the 2026-27 General Appropriations Act, Senate Bill 1, 89th Legislature, Regular Session, 2025 (Article II, HHSC, Rider 23).
HHSC has published Information Letter (IL) 25-11, Discontinuation of the Attendant Compensation Rate Enhancement Program and Rate Increases for Attendant Services, effective Sept. 1, 2025. Review the IL for more information.
If you have further questions, contact the HHSC PFD, Long-term Services and Supports (LTSS), Center for Information and Training (CIT) at PFD-LTSS@hhs.texas.gov or (737) 867-7817.
Letter To Providers From Twogether Consulting: June 30th, 2025
June 30th, 2025

From Twogether Consulting!
Hello Everyone!

The year is flying by, and the 4th of July is already nearly here. I hope there are plenty of fun activities planned for this Friday and the weekend!
Don’t forget that hurricane preparedness sessions are still available from HHSC. They have several sessions to assist HCS/TxHmL/ISS/ICF providers. We do have a few live webinars for July 2025- “Completing ICAPs & IDRCs and Understanding LONs” as well as “Requesting Adaptive Aids, Minor Home Modifications, & Dental Services in The HCS Program”.
Twogether Consulting, along with Nursing Innovations, will be hosting a 3-day live training HCS training session in San Antonio, Tx, towards the end of August.. The session will be 3 days, and providers will be able to choose which days they want to attend or pay for all days for a discounted rate. We will have more details posted on the website in the near future. Twogether Consulting will keep you posted, or you can check out our home page on the website for current calendar events. We are still available for facility and 1 on 1 requests for webinars and live training in July. Remember that you can view all calendar postings on our Twogether Consulting website.
Twogether Consulting is pleased to have hosted Rachel Hopkins, Program Director of Healthcare Services at Molina HealthCare of Texas as our guest presenter today for our “Free IDD Provider & Family Resource Webinar” on June 30th, 2025, from noon to 1 pm. Rachel is also a certified Person- Centered Thinking Trainer. Rachael did a great job of explaining STAR+PLUS services and how the MCOs work with providers and LIDDAs as well as some of the value-added benefits specifically provided by Molina Healthcare of Texas. This session provided other information as well about STAR+PLUS Medicaid program, including its healthcare benefits, service coordination teams, and collaboration with IDD Providers and LIDDAs. We had a good amount of questions, and I appreciate the time she spent with our attendees after the presentation. We have posted a link to the recorded session on our gotostage channel as well as Twogether’s FB page and my Linkedin page. Please feel free to share.
Molina Healthcare of Texas- PPT handout
This August, Twogether Consulting will host Disability Rights of Texas as our next presenter in our “Free IDD Resource Webinar” series.
We have a variety of pre-recorded webinar trainings for program managers, case managers and nurses, and direct care, so feel free to email us at info@twogetherconsulting.com to inquire. Let us know what areas of training you would like, to help us plan future sessions.
Here are just a few of the recent pre-recorded webinar trainings available for purchase: “Admission, Post-Admission & Other Follow-Up Requirements-HCS Program”, ICAPs/LON’s/IDRC’s-ICF Program” (Also have for HCS program), “Development of The Comprehensive Nursing Assessment & Nursing Service Plan-HCS or ICF”, “Best Practices For HCS Providers: How To Remain In Compliance With TAC Ch 565”, “Role & Responsbilities of The Q”, “Surrogate Decision Making Process, Rights Restrictions & Immediate Jeopardy-ICF Program”, “Licensed ISS Providers: What You Really Need To Know.”, We also have a ore-recorded 5 part Care Coordination/Case Management series as well for the HCS program. All of these sessions and many more come with handouts as well as the link to the pre-recorded session
Please see our “Updates” section of the website for the latest news for IDD providers.

Rate Packets Now Available: For HCS/TxHmL/ICF/CFC/HCBS-AMH Waivers
June 30th, 2025
Rate Packets Now Available
The rate hearing packets were posted on the PFD website on June 23, 2025. The hearing is being conducted to receive public testimony on the proposed Medicaid Rates.
Public Rate Hearing on July 16, 2025
The HHSC Provider Finance Department (PFD) Long Term Services and Support (LTSS) will hold its Public Rate Hearing on July 16, 2025, to address proposed rates for the following:
- Medicaid and Non-Medicaid Payment Rate Actions for Attendant Services in various programs, and
- Medicaid Payment Rate Actions for Nursing Facilities (NFs) and Nursing Facility Special Reimbursement Class for Individuals with Intellectual and Developmental Disabilities (IIDs).
Session One: 9:00–10:45 a.m. CDT
Session Two: 11:15 a.m.–1 p.m.
Session Three: 2:00–3:45 p.m.
This rate hearing will be conducted both in person and as an online event. Register for the hearing to attend this online meeting. After registering, you will receive a confirmation email containing information about joining the webinar.
You can also dial in on your phone. To do so, follow the link above to register. You will then be provided dial-in instructions, including an audio PIN. The audio PIN must be entered to speak over the phone audio during the hearing.
Public Notice and Testimony
The notice for the rate hearing was published in the June 20, 2025, issue of the Texas Register and posted to the HHSC website on June 11, 2025. Unless otherwise noted in the notice and the rate hearing packets, written comments regarding the proposed payment rates may be submitted instead of, or in addition to, oral testimony until 5 p.m. (CDT) on the day of the hearing. Written comments may be sent by U.S. mail, overnight mail, special delivery mail, fax, or email, as follows:
U.S. Mail:
Texas Health and Human Services Commission
Attention: Provider Finance, Mail Code H-400
P.O. Box 149030
Austin, Texas 78714-9030
Overnight mail or special delivery mail:
Texas Health and Human Services Commission
Attention: Provider Finance, Mail Code H-400
North Austin Complex
4601 Guadalupe St.
Austin, Texas 78751
Phone number for package delivery: (512) 730-7401
Fax:
Attention: Provider Finance at (512) 730-7475
Email:
Long Term Support Services – PFD-LTSS@hhs.texas.gov
Persons with disabilities who wish to participate in the hearing and require auxiliary aids or services should contact Provider Finance at (512) 730-7401 at least 72 hours before the hearing so appropriate arrangements can be made.
Preferred Communication
If possible, use email or phone for the quickest response to communicate with HHSC about this rate hearing.
Forward this information to providers and organizations in your programs as appropriate. If you have any questions about this rate hearing, email PFD LTSS.
Twogether Consulting’s Satisfied Customer Page
June 26th, 2025
We would greatly appreciate a quote from any of our clients who would like to write up a short paragraph on how we may have helped your organization or any recommendations you have for others about our services at Twogether Consulting that you may have used over the years. We are also happy to accept updates to previous satisfied customer quotes that are currently posted on the site.
Link to Satisfied Customers Page
If you would like to send us a quote, feel free to email us at info@twogetherconsulting.com
Note: Please type Satisfied Customer Quote in the subject line. Be sure to leave your full name, company name, and title. You are also welcome to leave a website link or email if you would like.
ICF/IID Updates

June 26th, 2025
HHSC Publishes Revised Process for Reporting Incidents, Complaints and HHSC Investigations of Abuse, Neglect, and Exploitation (PL 2025-02) for ICF
HHSC Long-Term Care Regulation updated Provider Letter (PL) 2025-02 Process for Reporting Incidents, Complaints and HHSC Investigations of Abuse, Neglect, and Exploitation for Intermediate Care Facilities for Individuals with an Intellectual Disability (ICF/IID) to include the facility must report the alleged abuse, neglect, and exploitation (ANE) to HHSC Complaint and Incident Intake within one hour of suspecting or learning of the allegation. This includes instances in which the facility learns of the alleged ANE when the surveyor enters the ICF on the complaint investigation and informs the provider of the allegation. This PL replaces PL 2024-04.
For questions contact LTCRPolicy@hhs.texas.gov.
April 8th, 2025
April & May Trainings for ICF
Reporting Abuse, Neglect, Exploitation Changes and Self-Reporting Incidents for Intermediate Care Facilities
Wednesday, April 9
10 – 11 a.m.
Register here for the webinar.
Reporting Abuse, Neglect, Exploitation Changes and Self-Reporting Incidents for Intermediate Care Facilities
Thursday, May 22
2 – 3 p.m.
Register here for the webinar.
Hurricane Season – Ready or Not! Preparedness for Intermediate Care Facilities (ICF)
Wednesday, May 28
10 a.m. – noon
Register here for the webinar.
February 22nd, 2025
HHSC LTCR Updates Tag Crosswalks for Intermediate Care Facilities
LTCR has updated the ICF federal, licensure and state standards of participation tag crosswalks to the most current version.
Each crosswalk provides a detailed table that identifies the applicable tag numbers, title, Code of Federal Regulations and Texas Administrative Codes for providers to reference.
These documents are posted on the ICF Provider Portal HHSC website.
For questions, email LTCRPolicy@hhs.texas.gov.
November 13th, 2024
HHSC Rescinds PL 2024-20 Requirements for Tuberculosis Screening and Testing
HHSC rescinded PL 2024-20 Requirements for Tuberculosis Screening and Testing. Additional guidance regarding tuberculosis screening and testing will be forthcoming.
In the interim, providers should follow their program regulations and internal communicable disease and infection control policies and procedures to address tuberculosis screening and testing.
Providers may use recommendations from the Centers for Disease Control and the Texas Department of State Health Services to inform their policies.
For more information, follow the links below:
Frequently Asked Questions About TB | Texas DSHS
Tuberculosis Screening for Adults in Various Settings (PDF)
August 12th, 2024
PL 24-04 –Changes & Guidance To ICF/IID Provider Reporting Processes and HHSC Investigating Processes- Effective March 1, 2024.
As the ICF/IID rules to implement HB 4696 applies to the 6-13 bed facilities and is not yet adopted, yet the provisions in the bills became effective 9/1/2023. We are unclear if or how HHSC is monitoring for compliance as the only guidance released to date is PL 24-04 . And, this PL only addresses the provider reporting processes and HHSC investigating processes which became effective March 1, 2024. The PL does not provide guidance or address compliance related to the directives in the bill which, as of September 1, 2023, is now law.
In response to inquiries from providers and provider associations, HHSC has now stated that “at this time ICF/IID surveyors are surveying for compliance with the current regulations located in 26 TAC 551 and guidance issued in PL 2024-04.“
NOTE: HCS/TxHmL: It’s anticipated the rules to implement HB 1009 in HCS/TxHmL will be posted for ‘informal’ comment this fall. Rules to implement HB 4696 are postponed until after the 89th Session.
March 10th, 2024
ICF/IID ANE Webinar- Very Important!
Thursday, March 21
2–3:30 p.m.
Register here for webinar.
HHSC Long-term Care Regulation has published Provider Letter 2024-04 Revised (Replaces PL 17-02 and 17-03) Revised Process for Reporting and HHSC Investigations of Abuse, Neglect, and Exploitation for Intermediate Care Facilities for Individuals with an Intellectual Disability (ICF/IID). Don’t forget, as of March 1st, 2024, this replaces the previous ANE Reporting & Investigations process. Reporting is now done to (CII) Complaint & Incident Intake.
February 25th, 2024
New Reporting Process for ANE Reporting & Investigations for ICF/IID Program
HHSC has released a new letter of guidance regarding the revised ANE reporting process to CII and the ANE investigation process for ICF/IID. Here is the published provider letter (PL) 2024-04
Beginning March 1, 2024, reporting of investigations for allegations of abuse, neglect, and exploitation (ANE) for Medicaid consumers served by an Intermediate Care Facility for Intellectual and Developmental Disabilities (ICF/IDD) will transition from the Department of Family and Protective Services Statewide Intake (DFPS SWI) to HHSC Regulatory Services Complaint and Incident Intake (CII).
Additionally, processes related to investigations of ANE of ICF/IDD will change as of March 1, 2024.
For questions contact LTCRPolicy@hhs.texas.gov.
January 20th, 2024
Surrogate Decision-Making Program (SDMP)
Randy Rowley, Manager, SDMP, HHSC, provided an overview of the surrogate decision-making program to the workgroup. Click here for link to ppt
HHSC December 27, 2023 Bulletin:
The legislatively mandated Surrogate Decision-making Program (SDMP) authorizes Surrogate Consent Committees (SCCs), comprised of trained volunteers, to provide written informed consent for individuals residing in community-based ICFs/IID who have been assessed to lack the capacity to make certain treatment decisions for themselves and have no legal guardian or actively involved family members serving as Surrogate Decision Makers (SDMs) or the treatment decisions are beyond the scope of the SDMs.
The SDMP facilitates compliance with Code of Federal Regulations (CFR) Title 42 and state ICF/IID rules regarding protection of individuals rights.
For the list of treatment decisions that a SCC can make see the HHS SDMP webpage.
Watch for upcoming training event announcements.
For questions about SCCs, or if you want to volunteer to serve on a SCC, email SDMP Manager Randy Rowley or call 512-438-4306.
ICF Rules-TAC Code Draft Title 26 Part I Ch 551
Personal Needs Allowance Information Letter
Personal Needs Allowance (PNA): PNA of individuals residing in a nursing home or ICF/IID from $60/month to $75/month, and for couples from $120/month to $150/month effective January 1, 2024. HHSC posted an information letter regarding this change:
IL 2023-45 Personal Needs Allowance (PNA) Adjustment (Replaces IL 2022-16) (texas.gov).
June 15th, 2023
Personal Needs Allowance Increase Bill passed during 88th legislature session
December 15th, 2022
ICF Resources
These resources can also be found on the ICF Provider Portal page.
September 25th, 2022
HHSC Publishes Updated Guidance on the Amelioration of Administrative Penalties for ALF, ICF/IID, and NF Providers
HHSC Long-term Care Regulation has published Provider Letter 2022-24 – Amelioration of Administrative Penalties (replaces PL 2013-18).
The letter provides guidelines to assisted living facilities,
intermediate care facilities for individuals with an intellectual
disability or related conditions, and nursing facilities about
the amelioration of administrative penalties assessed for state licensure
violations.
Read the provider letter details.
June 12th, 2022
ICF COVID-19 Vaccination Reporting Emergency Rules Expired June 6!!
Emergency rules for Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions that require COVID-19 vaccination reporting expired June 6.
This means that effective June 7, ICFs no longer have to report COVID-19 vaccination data for staff and individuals to HHSC.
The following rules expired June 6:
- 26 TAC §551.48 – ICF/IID Provider COVID-19 Vaccination Data Reporting Requirement.
Here is a copy of the previous rule that expired:
551.48.ICF/IID Provider COVID-19 Vaccination Data Reporting Requirement.
(a) An intermediate care facility administrator and one additional designee must enroll in an emergency communication system in accordance with instructions from Texas Health and Human Services Commission (HHSC).
(b) An intermediate care facility must respond to requests for information received through the emergency communication system in the format established by HHSC.
(c) Within 24 hours of becoming aware of a staff or resident’s COVID-19 vaccination, an intermediate care facility must accurately report COVID-19 vaccination data for staff and individuals in the format established by HHSC.
(d) Subsection (c) of this section does not apply to state supported living centers.
The agency certifies that legal counsel has reviewed the emergency adoption and found it to be within the state agency’s legal authority to adopt.
Filed with the Office of the Secretary of State on August 10, 2021.
Email questions to LTCR Policy.
April 29th, 2022
ICF Visitation Rules Update
An alert went out to remind providers that all visitation must be allowed. Essential caregiver and end-of-life visits must be allowed for all individuals with any COVID-19 status. A facility may be cited if visitation is not allowed.
Review ICF/IID visitation rules from April 4th, 2022, for additional information.
April 10th, 2022
COVID-19 ICF Mitigation, Response Rule Revised Effective April 6
HHSC Long-term Care Regulation has published a revised Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions COVID-19 Mitigation and Response Emergency Rule. It is effective April 6, 2022.
The revised rule:
- Removes the requirements to have plans for obtaining and maintaining a two-week supply of full PPE.
- Clarifies that a facility does not have to provide the name of the person who tested positive for COVID-19 when reporting to CII.
April 10th, 2022
HHSC Publishes Description of Key Changes to 26 TAC 551, ICF/IID (PL 2022-07)
HHSC has published Provider Letter 2022-07, Description of Key Changes to 26 TAC 551, Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions, for ICF/IID providers. This letter describes the key changes to Title 26 of the Texas Administrative Code, Chapter 551, that were effective on Feb. 24.
Throughout the rule, HHSC updated citations, agency names, and terminology; corrected minor grammatical and punctuation errors; and revised sentence structures to make the chapter easier to read. In addition, the following items are addressed in this letter:
– New Requirements for Infection Prevention and Control Policies and Procedures
-HHSC included a state rule that refers to each Centers for Medicare & Medicaid Services (CMS) Condition of Participation (CoP). Additions to 26 TAC 551 include • Governing Body • Client Protections • Facility Staffing • Active Treatment • Client Behavior and Facility Practices • Health Care Services • Physical Environment • Emergency Preparedness • Dietetic Services.
– transition from paper applications to the use of the online licensure portal, called the Texas Unified Licensure Information Portal (TULIP) (Disclose information when applying for “relocation” and application information must be submitted through portal in “TULIP” system)
-Now require evaluation of the emergency preparedness and response plan at least every two years, instead of annually.
-ANE & Incident definitions
-Administrative penalties for each visit are limited to the cap amount, regardless of the number or duration of violations as of Sept. 1st, 2021
****If you have any questions about this letter, please contact the Policy and Rules Section by email at LTCRPolicy@hhs.texas.gov or call (512) 438-3161
April 6th, 2022
COVID Screening in ICF’s
ICF COVID-19 Mitigation and Provider Response emergency rules require an intermediate care facility must screen individuals according to HHSC guidance
.ICFs must screen individuals:
•upon admission or readmission to the facility; and
•at least once a day.
ICFs must screen each employee or contractor for the following criteria (listed below) before entering the facility at the start of their shift.
•Staff screenings must be documented in a log kept at the facility entrance and must include the name of each person screened, the date and time of the evaluation, and the results of the evaluation.
**Staff who meet any of the criteria must not be permitted to enter the facility.
As per ICF/IID Expansion of Reopening Visitation Emergency rules, ICFs are required to screen all visitors for signs or symptoms of COVID-19.
*Visitor screenings must be documented in a log kept at the entrance to the facility, which must include the name of each person screened, the date and time of the screening, and the results of the screening. The visitor screening log may contain protected health information and must be protected in accordance with applicable state and federal law .
*A visitor may not participate in a visit if the visitor has signs and symptoms of COVID-19 or active COVID-19 infection.
Screening Criteria:
•fever, defined as a temperature of 100.4 Fahrenheit and above, or
signs or symptoms of a respiratory infection, such as cough, shortness of breath, or sore throat;
•other signs or symptoms of COVID-19, including
-chills,
-new or worsening cough,
-shortness of breath or difficulty breathing,
-fatigue,
-muscle or body aches,
-headache,
-new loss of taste or smell,
-sore throat,
-congestion or runny nose,
-nausea or vomiting,
-or diarrhea;
•any other signs and symptoms as outlined by the CDC in Symptoms or Coronavirus at cdc.gov;
•contact in the last 14 days with someone who has a confirmed diagnosis of COVID-19, is under investigation for COVID-19, or is ill with a respiratory illness, regardless of whether the person is fully vaccinated, unless the person is entering the facility to provide critical assistance; or
•testing positive for COVID-19 in the last 10 days.
April 6th, 2022
Reporting Confirmed Case of COVID-19 in ICF/IID
A facility must notify the Texas Health and Human Services Commission (HHSC) Complaint and Incident Intake of COVID-19 activity as described below.
(1) A facility must notify HHSC of the first confirmed case of COVID-19 in staff or individuals, and the first confirmed case of COVID-19 after a facility has been without cases for 14 days or more, at HHSC Complaint and Incident Intake (CII) through TULIP, or by calling 1-800-458-9858, within 24 hours of the positive confirmation.
(2) A facility must submit a Form 3613-A Provider Investigation Report, minus the name of the person who tested positive for COVID-19, to HHSC Complaint and Incident Intake, through TULIP, by email at ciiprovider@hhs.texas.gov, or by fax at 877-438-5827, within five working days from the day a confirmed case is reported to CII.
April 6th, 2022
COVID-19 Mitigation and Response Emergency Rule Updated
HHSC Long-term Care Regulation has published a revised Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions COVID-19 Mitigation and Response Emergency Rule.
It became effective April 6, 2022.
The revised rule:
•Points to guidance from the Texas Department of State Health Services and HHSC rather than the CDC.
•Removes the requirements to have plans for obtaining and maintaining a two-week supply of full PPE.
•Removes the requirement to have spaces to don and doff PPE
•Clarifies that a facility does not have to provide the name of the person who tested positive for COVID-19 when reporting to CII.
February 27th, 2022
HHSC Adopts Revised ICF/IID Rules – Effective Feb. 24th, 2022
HHSC Long-term Care Regulation has adopted updates to the Intermediate Care Facilities for Individuals with an Intellectual Disability (ICF/IID) or Related Conditions program rules. The revised rules are in the Texas Administrative Code Title 26, Chapter 551. They are effective Feb. 24, 2022.
Key changes to the rule are to:
- Implement House Bill 1848 from the 86th Legislature, Regular Session, 2019 which requires new infection control policies and procedures in long-term living facilities.
- Implement House Bill 3720 from the 87th Legislature, Regular Session, 2021 which limits the total amount of an administrative penalty assessed against an ICF/IID.
- Reintegrate the conditions of participation from the Code of Federal Regulations.
- Corrects legacy agency terms, update rule citations, and edit for clarity and consistency.
COVID-19 ICF/IID Webinar Recording from Feb. 14 Available
A recording of the Feb. 14 Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions COVID-19 Q&A with HHSC Long-term Care Regulation and DSHS is available for those who could not attend.
There have been changes made to the PowerPoint based on the information provided by DSHS during the webinar.
Listen to the webinar recording.
Email LTCR Policy for the transcript.
February. 20th, 2022
Mar. 07 ICF COVID-19 Webinar with HHSC LTCR
Long-term Care Regulation and the Department of State Health Services will provide the latest information on the COVID-19 pandemic and take live questions from participants in this intermediate care facilities provider webinar.
Provider attendance is critical to staying current with COVID-19 requirements and guidance. ICF/IID providers are strongly encouraged to attend all COVID-19 webinars with LTCR and DSHS.
Those using Internet Explorer may have difficulties registering for the webinar. If so, try using another browser, such as Google Chrome or Microsoft Edge.
March 7, 2022
11 a.m.–12 p.m.
Register for the COVID-19 Webinar.
February 13th, 2022
HHSC is not currently assessing compliance with CMS’s Omnibus COVID-19 Health Care Staff Vaccination rules, published in the Federal Register on November 5, 2021.
ICF COVID-19 Vaccination Data Reporting and Emergency Communication System – Feb 7
HHSC Long-term Care Regulation has published a revised ICF/IID Provider COVID-19 Vaccination Data Reporting Rule (PDF). It became effective February 7, 2022 and includes Emergency Communication System Enrollment for Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions providers.
The rule requires ICF/IIDs to:
- Report COVID-19 vaccine data within 24 hours
- Enroll in an emergency communication system
January 7th, 2022
ICF COVID-19 Response Plan and FAQ Updated – Jan. 7
Document Version Date Change Comments
Version 3.5 1/5/2022 Changes to pages 6, 31, 38, 39, 40, 51, 72 71, and Changes made to reflect the most updated CDC guidance.
Version 3.4 12/07/2021 Changes to pages 15, 16, 25, 26, 31, 35 Edited to include revised ICF COVID-19 Provider Response Mitigation Rules for ICFs/IID
For changes made previous to 12/07/2021, please read the Table of Changes starting with page 7 of 19 of the Response Plan.
Update your Infection Control Policies and other related policies accordingly.
HHSC has revised the ICF COVID-19 Response Plan and Frequently Asked Questions document in response to the most recent CDC guidance.
November 21st, 2021
HHSC Publishes PL 2021-38 Medicaid Bed Reallocation
HHSC published Provider Letter 2021-38 Medicaid Bed Reallocation which explains the process to request reallocated ICF/IID Medicaid beds from HHSC. This letter replaces Provider Letter 2019-21.
November 4th, 2021
Updated ICF/IID COVID-19 FAQ and COVID-19 Response Plan Revised
HHSC has revised the Frequently Asked Questions for ICF/IIDs about COVID-19 (PDF) and the ICF/IID COVID-19 Response Plan (PDF) in response to the revised COVID-19 Expansion of Reopening Visitation for ICF Providers rules.
October 24th, 2021
New PL 2021-21 COVID-19 – Expansion of Reopening Visitation for ICF Providers
Super important!!!!
HHSC has published Provider Letter 2021-21, COVID-19 Response – Expansion of Reopening Visitation (PDF) for ICF/IID providers. This letter replaces Provider Letter 2021-10. This letter describes the criteria for expanded visitation as well as address changes in response to Executive Order No. GA-38(link is external) and updated CDC guidance.
Updated COVID-19 Expansion of Reopening Visitation Emergency Rules for ICF Providers
HHSC Long-term Care Regulation has published revised COVID-19 Expansion of Reopening Visitation Emergency Rules for Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICFs/IID) or Related Conditions (PDF). The rules address changes in response to Executive Order No. GA-38 (PDF)(link is external) and updated CDC guidance.The rules became effective on October 20, 2021.
September 15th, 2021
HHSC Publishes Amended Statutory Cap Regarding Administrative Penalties for ICFs: (PL 21-34)
HHSC published Provider Letter 21-34 Amended Statutory Cap Regarding Administrative Penalties for Intermediate Care Facilities. PL 21-34 notifies providers of changes to how HHSC determines and imposes administrative penalties based on changes made by House Bill 3720 (87th Legislature, Regular Session, 2021).
September 5th, 2021
Guidance for Providers Regarding Entry into LTC Facilities (PL 2021-33)
HHSC Long-term Care Regulation has published Provider Letter 2021-33, Authority to Enter Long-term Care Facilities (PDF), for ALF, HCS, ICF/IID and NF providers. This letter reminds providers that they must allow persons providing critical assistance and providers of essential services to enter the facility if they pass the facility’s COVID-19 screening.
September 5th, 2021
ICF/IID Leave During COVID-19 Rule Reinstated
HHSC has published IL 2021-42 ICF/IID Services During COVID-19 (PDF), which replaces IL 2020-43.
A resident must be discharged from the Intermediate Care Facility for Individuals with an Intellectual Disability or Related Conditions, with or without a contract to hold the resident’s placement in accordance with 26 TAC Section 261.227(j), if the resident is absent from the ICF/IID for one full day or more and the absence is not during leave described in 26 TAC Section 261.226.
August 1st, 2021
HHSC Publishes Updated COVID-19 Response Plan and Frequently Asked Questions for ICF Providers
HHSC Long-term Care Regulation updated the ICF COVID-19 Response Plan and FAQ document on July 29, 2021.
Read the updated ICF COVID-19 Response Plan (PDF).
Read the updated ICF FAQs (PDF).
March 24th, 2021
HHSC Adopts New Expansion of Reopening Visitation Emergency Rules for ICF Providers!!!
HHSC has adopted new Expansion of Reopening Visitation (PDF) emergency rules that establish criteria for expanded indoor and outdoor visitation as well as essential caregiver visits. These rules are effective March 24, 2021.
HHSC Publishes COVID-19 Response – Expansion of Reopening Visitation for ICF Providers (PL 2021-10)
HHSC has published Provider Letter 2021-10, COVID-19 Response – Expansion of Reopening Visitation (PDF) for ICF/IID providers. This letter replaces Provider Letter 2020-43. This letter describes the criteria for expanded indoor and outdoor visitation as well as essential caregiver visits.
March 22nd, 2021
ICF COVID-19 March 22 Webinar Recording Available
A recording of the March 22, 2021, ICF/IID COVID-19 Q&A with HHSC LTC Regulation and DSHS is available for those who could not attend.
Listen to the COVID-19 Q&A recording.
March 11th, 2021
Recording of ICF COVID-19 March 8 Provider Webinar Available
A recording of the March 8, 2021 ICF/IID COVID-19 Q&A with HHSC LTC Regulation and DSHS is available for those who could not attend.
Listen to the COVID-19 Q&A recording.
February 8th, 2021
Draft ICF/IID Rule Changes
- Draft ICF/IID Rule Changes- See link: https://documentcloud.adobe.com/link/track?uri=urn:aaid:scds:US:cf5ea154-04b4-4c75-8aec-7e230c3cfda0
- High Level Summary of Proposed Changes See link: https://documentcloud.adobe.com/link/track?uri=urn:aaid:scds:US:2aa689d6-3018-4ab9-8d75-04578f4c922d
February 7th, 2021
Feb. 8- ICF/IID Provider Bed Hold Payments Webinar &
Reminder to Provide Letter to Families
IL 2020-43, ICF/IID Services During COVID-19 directed program providers to give a copy of the letter attached to that IL to each resident who was:
- Absent from an ICF/IID
- Not on leave
- Was not discharged from the ICF/IID
If you have not provided the letter to residents who meet that criteria, do so immediately. It was to be complete by Oct. 5, 2020. You must assist residents in deciding to do only one of the following:
- Return to the facility.
- Continue to be absent from the facility, be discharged, but enter into an agreement with the ICF/IID to hold your place at the facility.
- Continue to be absent from the facility and be discharged.
HHSC Medicaid and CHIP Services will issue instructions to providers about entering COVID-19 therapeutic leave for days a resident was away from an ICF/IID to reduce the risk of COVID-19 transmission. Register for the following webinar to review the emergency rules authorizing this leave and the instructions for entering it.
ICF/IID Provider Bed Hold Payments Webinar
Friday, Feb. 5
9:30-11 a.m.
Register for the Bed Hold Payment Webinar.
The emergency rule authorizing payment for COVID-19 therapeutic leave (PDF) is effective Jan. 29, 2021.
January 19th, 2021
HHSC Updates the ICF COVID-19 Response Plan and FAQ Document
Please be sure to update your infection control and other related policies based on the updated Response Plan!!!
Let us know if we can help. We will be working on some of these addendums in the next few weeks.
HHSC Long-term Care Regulation updated the ICF COVID-19 Response Plan and FAQ document on Jan. 12, 2021.
Read the updated ICF COVID-19 Response Plan (PDF).
Read the updated ICF FAQs (PDF).
Jan. 25 ICF Provider COVID-19 Webinar with HHSC LTC Regulation
Long-term Care Regulation and the Department of State Health Services provide the latest information on the COVID-19 pandemic and take live questions from participants in this ICF provider webinar. Provider attendance is critical to staying current with COVID-19 requirements and guidance.
ICF/IID providers are strongly encouraged to attend this and all biweekly COVID-19 webinars with LTCR and DSHS.
Those using Internet Explorer may have difficulties registering for the webinar. Please try another browser such as Google Chrome or Microsoft Edge.
ICF Provider Webinar
Jan. 25, 2021
11 a.m. – 12:30 p.m.
Register for the COVID-19 Webinar.
Recording of ICF COVID-19 Jan. 11 Provider Webinar Available
A recording of the January 11, 2021 ICF/IID COVID-19 Q&A with HHSC LTC Regulation and DSHS is available for those who could not attend.
Listen to the COVID-19 Q&A recording.
January 10th, 2021
Informal Comments on Draft Rules for ICF/IID or Related Conditions
HHSC is accepting informal comments from stakeholders on the following draft rules, which are now posted on the HHS Rulemaking page. The comment period ends Jan. 19, 2021.
This project implements two bills from the 86th Legislature, Regular Session, 2019. House Bill (H.B.) 1848 contains required elements for infection prevention and control. H.B. 3803 limits the daily amount of an administrative penalty assessed against an ICF/IID. The project will also update rule references and agency names, amend rules to align with Centers for Medicare & Medicaid Services conditions of participation in the ICF/IID program, and edit the rules for clarity and consistency.
HHSC Publishes Revised Reporting Guidance for Long-Term Care Providers
(PL 20-37)
HHSC has published a revised version of Provider Letter 20-37, Reporting Guidance for Long-Term Care Providers (PDF). The revision includes information for ALF and ICF providers offering point-of-care testing for COVID-19 and clarifies reporting requirements for NF providers.
November 22nd, 2020
November 30 ICF Provider COVID-19 Webinar with HHSC LTC Regulation
LTCR and DSHS provide the latest information on the COVID-19 pandemic and take live questions from participants in this ICF provider webinar. Provider attendance is critical to staying current with COVID-19 requirements and guidance.
ICF/IID providers are strongly encouraged to attend this and all biweekly COVID-19 webinars with HHSC Long-term Care Regulation and the Department of State Health Services.
Those using Internet Explorer may have difficulties registering for the webinar. Please try another browser such as Google Chrome or Microsoft Edge.
ICF Provider Webinar
November 30, 2020
11 a.m. – 12:30 p.m.
Register for the COVID-19 webinar.
Recording of November 16 ICF COVID-19 Q&A Provider Webinar Available
A recording of the November 16, 2020 ICF/IID COVID-19 Q&A with HHSC LTC Regulation and DSHS is available for those who could not attend.
View the COVID-19 Q&A recording.
10/16/20
Important Information!
LTCR FORM 2195: Expansion of Reopening Visitation Status Attestation and Letter PL 20-43 (for ICF Only)
Note: to receive an approved general visitation designation, a small ICF/IID that cannot provide separate areas, units, wings, halls, or buildings for individuals who are COVID-19 positive, COVID-19 negative or unknown COVID-19 status, based on the status of the entire facility, must:
- have no facility-acquired COVID-19 cases in individuals for at least 14 consecutive days; and
- have no COVID-19 cases in staff.
An ICF/IID must provide instructional signage throughout the facility and proper visitor education regarding
- signs and symptoms of COVID-19;
- infection control precautions; and
- other applicable facility practices (e.g., the use of facemasks or other appropriate PPE, specified entries and exits, routes to designated visitation areas, and hand hygiene).
An ICF/IID that does not meet the criteria for a visitation designation must permit closed window visits and end-of-life visits for individuals regardless of their COVID-19 status, as well as essential caregiver visits for individuals with COVID-19 negative or unknown COVID-19 status.
Such an ICF/IID must also develop and implement a plan to meet the visitation criteria and submit the plan to the regional director in the Long-term Care Regulation (LTCR) region where the ICF/IID is located within five days of submitting the new 2195 Expansion of Reopening Visitation Status Attestation Form,
or
within five days of receiving notification from HHSC that the ICF/IID was not approved for general visitation designation.
LTCR Form 2195
Each ICF/IID must submit LTCR Form 2195 to the Regional Director in the LTCR region where the facility is located and must provide information about whether the ICF/IID meets or does not meet the criteria for expanded general visitation.
Each ICF/IID must submit a completed form 2195 to the Regional Director no later than October 31, 2020.
An ICF/IID that does not meet the visitation designation criteria must attest that it:
- is permitting closed window visits, end of life visits, and essential caregiver visits;
- will develop and implement a plan to meet the visitation designation criteria as defined in 26 TAC §551.47; and
- has included the plan with the form or will submit the plan within five business days of submitting the form.
To seek a designation for general visitation, an ICF/IID must complete LTCR Form 2195, Expansion of Reopening Visitation Status Attestation, to notify LTCR that the ICF/IID seeks a designation as a visitation facility.
The form must be emailed to the LTCR regional director in the LTCR region where the facility is located. Any applicable pictures and facility maps must also be included with LTCR Form 2195.
The LTCR regional director or designee will review the form within three working days of submission and notify the ICF/IID whether it has received been approved for a visitation designation.
An ICF/IID with previous approval for visitation does not have to submit LTCR Form 2195 or other documentation unless the previous visitation approval has been withdrawn, rescinded, or canceled, or was for only indoor or outdoor visitation instead of both indoor and outdoor visitation.
If approved, the ICF/IID must allow outdoor visits, indoor plexiglass visits, open window visits, and vehicle parades in accordance with the applicable emergency rule. HHSC LTCR can conduct an on-site visit to confirm an ICF/IID’s compliance with the requirements. If HHSC determines that the ICF/IID does not meet the requirements for the designation as a visitation facility, the ICF/IID must immediately stop all visitation except a closed window visit, end-of-life visit, and visits by persons providing critical assistance, including designated essential caregivers.
If, at any time after a visitation designation is approved by HHSC, the ICF/IID experiences an outbreak of COVID-19, the ICF/IID must notify the Regional Director in the LTCR Region where it is located that the ICF/IID no longer meets visitation criteria, and the ICF/IID must immediately stop all visitation, except a closed window visit, end-of-life visit, or visits by persons providing critical assistance, including essential caregivers.
The ICF/IID can submit a new request for designation when it meets all visitation criteria.
Under Section 37.10 of the Texas Penal Code, a person commits a criminal offense if he or she makes a false entry in a governmental record; makes, presents, or uses any record or document with knowledge of its falsity and intent that it be taken as a genuine governmental record; or makes, presents, or uses a governmental record with knowledge of its falsity. In addition, making a false statement on the attestation form can result in the imposition of an administrative penalty as described in Texas Health and Safety Code, Chapter 252, section 252.065(a)
Contact Information for Submitting LTCR Form 2195 to the LTCR Regional Director: https://hhs.texas.gov/about-hhs/find-us/long-term-care-regulatory-regional-contact-numbers
If you have any questions about this letter, please contact the Policy, Rules and Training Section by email at PolicyRulesTraining@hhsc.state.tx.us or call (512) 438-3161.
10/05/20
Deadline for Decision To Return to Facility/Payment to Hold Bed/Discharge Option
Information Letter No. 20-43 ICF/IID Services During COVID-19
10/03/20
Quick TIPS on New Changes for Expansion of Facility Visitation Rules & Other Policies Concerning COVID-19
Essential Caregiver Visits and Salon Services Visitor (Visitor types above and beyond normal designated visiting facility type)
Essential Caregivers are allowed even if the facility does not have designated visitation. They must be at least 18 years of age. Can be family, friend, guardian.
- 1.They must wear a facemask. 2. They must have evidence of negative COVID-19 test in the past 14 days and must be screened by facility staff prior to the visit. (Pay attention to the new additional symptoms and discontinuation of asking about international travel). 3. There is a 2- hr limit unless the facility allows a longer period of time. 4.They can have physical contact with their individual (and only their individual) 5.They must be limited to access to their person. 6.An assigned person must escort them to and from the location they are going to meet with the individual- room, outside… 7. The facility must approve the face mask they are going to wear or provide an appropriate mask. 8.If they do not have an appropriate face mask or the facility can’t provide one, they will need to reschedule the visit. 9. The facility must create an identifying badge for the essential caregiver or any salon service visitors. 10. The facility must have attestation stating the essential caregiver has visited and when they left (include time arrived, when they left, who they visited). 11. Essential caregivers must be trained on PPE and how to wear PPE, handwashing, and other infection control practices and there must be proof of this training that the facility maintains. 12..The individual must be COVID-19 negative to have an Essential caregiver visit or Salon Service Visitor.
- ***(If client status is unknown, the essential visitor would have to wear a face mask (not N-95, save that for your staff who need to work with COVID-19 + individuals), gown, gloves, goggles or face shield, so the facility might need to provide these other items)
Phase I Visitation Rules, no longer in effect!
Expanded Visitation Rules now in effect: The facility must apply with form 2194 for the Designated Visitation Facility, do not require all these same requirements an essential visitor (or Salon Service Visitors)- Designated visits include: open window visits, closed window visits, parade visits (open window or closed) outside visits, (and in plexiglass separate areas). Must use physical distance, visitor screening, individual will wear face mask or face covering if tolerated and the same for the visitor -they must wear a face mask or face covering. Provider Letter 20-38 has the link with form 2194 at the end of it. We encourage you to email the form. Most staff at HHSC are not in the office Visitation Designation department has 3 days to approve or deny the 2194 form request. Only the administrator or director can fill out form 2194!!
Previous Level 1 Attestation Approval: If you previously submitted the 2192 and received approval, you do not need to request a new one with form 2194, if your status is the same. If you want to change the visitation type, then you will need a new form. ( i.e. you did not want plexiglass partition previously and now you do.)
Small facilities must request visitation designation for the whole facility (unless you have a way to separate all cohort areas completely.) Do not fill out section #3. That is only for NF’s.
The provider must develop and must enforce policies and procedures including testing strategies for Essential Visitors, in addition to the testing that must occur at least 14 days prior to 1st visit and all other polices related, such as essential visitor requirements discussed above. Remember your testing strategies are required to provide expectations for the essential visitor for how often they will be required to test and when, for any visits they are making, after the initial “essential caregiver visit”.
For vehicle parades, the individual needs to remain 10 ft or more from the vehicle for safety.
Plexiglass booths on the inside must be approved by a life safety person for your region. Send in pictures. Does have to be a plexiglass barrier, does not have to be 2 and 3 sided.
**Closed window and End of Life visits are the only visits an individual may have if they are COVID-19 + (positive)
Remember staff should be assigned to an appropriate cohort (COVID-19 +, COVID-19 Negative or Unknown) then they should stay with that Cohort. In addition, there should be a policy at the facility for limiting the sharing of staff. If you need help with your policy concerning “COHORTS” and ” Mitigation of COVID-19 by Limiting Sharing of Staff”, please contact us. I do have some policies you can purchase if needed. Please contact me at: info@twogetherconsulting.com
FAQ’s (June 2020)
Answer: Regulations regarding ICF/IID discharge have not been waived. A discharge, even on a temporary emergency basis, requires that key developmental, behavioral, social, health and nutritional information be shared with the accepting facility in the community or non-facility provider. CMS is aware that staffing shortages and/or client surges due to the PHE create a high demand on available staff time that makes it difficult to complete a full discharge summary for each client. Each ICF will need to evaluate what amount and detail of documentation is necessary to ensure that critical health information is shared with the accepting facility or other provider. When available and if appropriate, the Interdisciplinary Team (IDT) should maximize the use of telehealth for the completion of a client’s discharge plan during the PHE.
Answer: Yes. CMS has temporarily waived certain regulatory requirements providing flexibilities to assist RHCs and FQHCs in furnishing services during the COVID-19 PHE. This includes temporarily modifying the following:(a)50% mid-level staffing requirement for RHCs;(b)Physician supervision requirement for nurse practitioners (NPs), to the extent permitted by State law; and(c)Location requirements for existing RHCs and FQHC to allow additions of temporary service locations.Please see https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf for additional waiver information. Additional flexibilities, including guidance for RHCs and FQHCs furnishing telehealth services during the PHE, are also described in this CMS MLN Article: https://www.cms.gov/files/document/se20016.pdf
Answer: Yes. During the COVID-19 PHE, CMS is allowing currently approved RHCs/FQHCs to provide patient care services in temporary expansion sites to help address the urgent need for supplementary care. These temporary sites are not restricted to the rural/shortage area location requirements. Each location is obligated to follow RHC/FQHC regulations to the extent not waived. Therefore, the RHC/FQHC may provide services provided at a temporary location under the CMS Certification Number (CCN) for the permanent location. The RHC/FQHC is expected to be operating in a manner not inconsistent with its state’s emergency preparedness plan. Note: FQHCs must also have an updated Health Resource and Service Administration (HRSA) Notice of Award, expanding the scope of service to include the temporary location(s) to support response to the COVID-19 PHE.
My RHC participates in Medicare through one of the two CMS-approved RHC Accreditation Organizations (AOs). Do waivers of CMS regulations apply to CMS-approved accrediting programs? Do I need to notify the AO of my desire to temporarily add a service location during the COVID-19 PHE?
Answer: To assist RHCs and FQHCs in furnishing service during the COVID-19 PHE, CMS has provided additional flexibilities related to billing for services. These temporary flexibilities currently include Expansion of Virtual Communication Services for RHCs and FQHCs to include online digital evaluation and management services using patient portals, and Revision of Home Health Agency Shortage Area Requirement for Visiting Nursing Services Furnished by RHCs and FQHCs. Please see the Medicare FFS Billing FAQ document available at https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf. Please see Section II.L of the Interim Final Rule with Comment Period, “Medicare and Expanded Flexibilities for Rural Health Clinics (RHCs) Medicaid Programs; Policy and Federally Qualified Health Centers (FQHCs) During Regulatory Revisions in Response to the COVID-–19 Public Health Emergency (PHE)”(85 FR 19230, 19253), available at https://www.federalregister.gov/documents/2020/04/06/2020-06990/medicare-and-medicaid-programs-policy-and-regulatory-revisions-in-response-to-the-covid-19-public, for more information on regulatory changes for RHCs and FQHCs.
Webinar info: How to prevent infectious diseases and the spread of infectious diseases in ICF-Specifically COVID-19 (May 27th, 2020)
See the following pdf link from HHSC
https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/providers/long-term-care/icfiid-covid-updates-qa-webinar-may-27-2020.pdf
 Survey Operations Resume as of June 15th, 2020
Survey Operations Resume as of June 15th, 2020
 Providers Must Log Residents’ Leave
Providers Must Log Residents’ Leave
All community-based ICF/IID program providers must submit an absence request in the TMHP ICF/IID Online Portal for a resident away from the facility for one or more full days. See the TMHP ICF/IID Online Portal User Guide (PDF) starting on page 52 for more information. The program provider must submit a return request within three days after a resident returns to the facility. See page 58 of the Online Portal User Guide for an explanation.
Please ensure that information entered in the portal for absences is current. HHSC uses the information to determine how many residents are absent from their facilities and the length of those absences.
PolicyRulesTraining@hhsc.state.tx.us or call (512) 438-3161.
Provider Joint Training Opportunities
Check out Joint Provider Trainings link from HHSC, for more info:
https://apps.hhs.texas.gov/providers/training/jointtraining.cfm#course_112
Survey Process for ICF Has Changed: Please Be Aware
You may check your SOMA (Surveyor’s Operational Manual for ICF in Appendix J) for these changes.
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_j_intermcare.pdf
http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R178SOMA.pdf
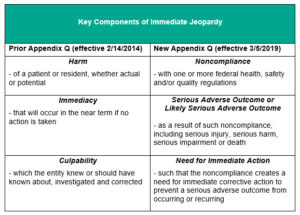
Appendix Q of SOMA (Immediate Jeopardy) Changes
CMS clarifications letter
SOMA appendix Q Section Immediate Jeopardy
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_q_immedjeopardy.pdf
|
LON & Facility Size |
Current Rates |
Proposed Rates |
|
SMALL |
|
|
|
LON 1 |
$144.25 |
$150.31 |
|
LON 5 |
$160.74 |
$167.90 |
|
LON 8 |
$182.82 |
$191.85 |
|
LON 6 |
$223.88 |
$236.59 |
|
LON 9 |
$406.11 |
N/C |
|
MEDIUM |
|
|
|
LON 1 |
$118.04 |
$123.14 |
|
LON 5 |
$134.06 |
$140.24 |
|
LON 8 |
$158.90 |
$166.92 |
|
LON 6 |
$190.24 |
$200.79 |
|
LON 9 |
$385.84 |
N/C |
|
LARGE |
|
|
|
LON 1 |
$112.09 |
$116.30 |
|
LON 5 |
$119.64 |
$124.64 |
|
LON 8 |
$133.22 |
$139.44 |
|
LON 6 |
$179.40 |
$188.96 |
|
LON 9 |
$387.25 |
N/C |
Twogether Consulting Newsletter Library

Subscribe To The Twogether Consulting Mailing List!
2025
April 17th, 2025-correction/addendum
2024
To Read previous newsletter editions from 2023, please click here

If you would like to be on our mailing list for this free publication, please click here to subscribe through Mailchimp for the newsletter subscription or if you prefer, you may click on our website link for newsletter subscription
TMP Merger With Cubhub: Rebranded as Statewise
June 26th, 2025
![]()
What Providers Need To Know
“TMP has joined Cubhub as part of the Statewise family—but nothing’s changing for Texas providers. TMP remains your trusted platform for IDD services.”
Important: What’s changing?
Just the name of the platform (From TMP to Statewise). With the support of Cubhub, TMP will get stronger and gain improved features, but it will continue to serve as the primary platform for Texas-based IDD and personal care providers. You will continue using the TMP platform as you know and trust, and the support team will remain the same.
For more information: https://statewise.com/blog/what-providers-need-to-know-as-tmp-merges-with-cubhub
Press Release: In Dallas, Texas, as of June 16th, 2025
More than a name change, the move to Statewise marks a bold step forward—focused on equipping Medicaid-based providers with the tools, insights, and support they need to deliver exceptional care across every state. The company has plans to expand features and refine modules alongside its partner companies to meet the challenges of a market that is undergoing seismic changes.
ICF Provider 2024 Conference Recordings Available For Viewing
June 25th, 2025
In case you were not aware, and you missed last year’s conference, we wanted to make sure ICF providers knew they could still watch the sessions. Great For your Q’s, Administrators, and QA staff.
HHSC Long Term Care Regulation has posted 4 recorded sessions from the 2024 ICF Conference “Embracing Change to Enhance Value” held Dec. 5, 2024.
No CEs or certificates of attendance are offered for viewing these recorded sessions.
iCareManager EHR System Information
June 25th, 2025

From iCareManager email received on June 25th, 2025
“We are thrilled to introduce you to the innovative & efficient iCareManager
All-In-One EHR Solution!
Whether you connected with us at a conference or online, you’ve just taken the first step towards smarter, simpler, and more efficient IDD service delivery.
To kick things off, we’re attaching our 2025 e-book. It will give you a complete overview of who we are, what we offer, and how our EHR system is built to make life easier for IDD service providers.”
| Download e-Book For FREE |
What Sets iCM Apart From Others?
- A Completely User-Friendly Dashboard
- SOC 2 & HIPAA Certification
- Holistic Solution To All Service Provision Needs
This is just the beginning, and we’re here to support you every step of the way
iCareManager, 6103 Parkway Dr, Laurel, MD 20707, United States
You may unsubscribe or change your contact details at any time.
Joint Training From HHSC For Providers
Joint Training Page Available for HCS/TxHmL/ICF/ISS Providers
The HCS and TxHmL programs now have a Joint Training Opportunities page where providers can register for upcoming classes. Class size will be limited to maximize participation, but classes will be offered regularly. Providers should check the page often for updates. There will be recordings of special presentations available for viewing on-demand later.
June & July 2025 LTCR Provider Webinar Training Opportunities
- Tuesday, June 17, 2025
- 10:00 AM – 11:30 AM
- Registration
Regional Offsite Review Process for Critical Incidents Reported into the Critical Incident Management System for HCS/TxHmL
- Thursday, June 19, 2025
- 3:00 PM – 4:00 PM
- Registration
Medication Management for HCS/TxHmL Providers
Wednesday, July 9, 2025
- 1:30 PM – 3:00 PM
- Registration
Hurricane Season – Ready or Not! Preparedness for Intermediate Care Facilities (ICFs)
- Monday, July 14, 2025
- 1:30 PM – 3:00 PM
- Registration
Reporting Abuse, Neglect, Exploitation Changes and Self-Reporting Incidents for Intermediate Care Facilities
- Wednesday, July 23, 2025
- 9:30 AM – 10:30 AM
- Registration
Hurricane Season – Ready or Not! Preparedness for Home and Community-Based Services, Texas Home Living (HCS/TxHmL), and Individualized Skills and Socialization Providers
- Tuesday, July 29, 2025
- 3:30 PM – 5:00 PM
- Registration
Live Training
Writing Acceptable Plans of Correction for HCS and TxHmL Providers (Longview, Tx)
- Wednesday, June 25, 2025
- 9:30 AM – 4:00 PM
- Registration
Writing Acceptable Plans of Correction for HCS and TxHmL Providers (Victoria, Tx)
- Wednesday, July 16, 2025
- 9:30 AM – 4:00 PM
- Registration
April & May 2025 LTCR Provider Webinar Training Opportunities
Webinars
License Types for Individualized Skills and Socialization Providers (course description)
- Wednesday, April 23, 2025
- 1:00 PM – 2:00 PM
- Registration
- Tuesday, May 6, 2025
- 2:00 PM – 3:00 PM
- Registration
Writing Acceptable Plans of Correction for ISS Providers (course description)
- Thursday, April 24, 2025
- 1:30 PM – 3:30 PM
- Registration
Death Notifications and Provider Investigation Reports for HCS/TxHmL Providers (course description)
- Friday, April 25, 2025
- 2:30 PM – 3:30 PM
- Registration
Understanding Reportable Incidents for Individualized Skills and Socialization Providers (course description)
- Tuesday, May 20th, 2025
- 3:30 PM – 4:30 PM
- Registration
Administrative Penalties and Related Processes in HCS & TxHmL Providers (course description)
- Wednesday, May 21, 2025
- 3:00 PM – 4:00 PM
- Registration
Live Trainings
- Writing Acceptable Plans of Correction for HCS and TxHmL Providers (course description)
- Wednesday, May 14, 2025
- 9:30 AM – 4:00 PM
Edison Plaza
350 Pine Street 9th floor
Room: 9036 B
Beaumont, TX 77701
From Awareness to Action: Responding to Abuse, Neglect and Exploitation
Tuesday, May 6
8:30 a.m. to 4:30 p.m.
Amarillo, TX
Register for in-person training
Infection Control – Break the Chain of Infection
Wednesday, May 7
8:30 a.m. to 4:30 p.m.
Amarillo, TX
Register for in-person training.
Web-Based Training
Top 10 Citations for Home and Community-based Services and Texas Home Living Fiscal Year 2023
Long-Term Care Regulation
https://apps.hhs.texas.gov/business/CBT/deficiences/hcs-txhml-2023/
January 2025 LTCR Provider Webinar Training Opportunities
Reporting Abuse, Neglect, Exploitation Changes and Self-Reporting Incidents for Intermediate Care Facilities
Tuesday, Jan. 14
2–3 p.m.
Register here for the webinar.
Regional Offsite Review Process for Critical Incidents Reported into the Critical Incident Management System for HCS/TxHmL
Wednesday, Jan. 15
2–3 p.m.
Register here for the webinar.
Flu and COVID-19: What You Need to Know
Thursday, Jan. 16
1:30–2:30 p.m.
Register here for the webinar.
Individualized Skills and Socialization Survey Process and ANE Overview
Tuesday, Jan. 21
2–3:30 p.m.
Register here for the webinar.
AlertMedia: Be Prepared. Stay Informed.
Friday, Jan. 24
1:30–2:30 p.m.
Register here for the webinar.
These 3 webinars below are not for HCS/TxHmL/ICF specifically, but they do apply to those in Long-Term Care Facilities or Programs
Weight Loss in Older Adults
Thursday, Jan. 23
1:30–3:30 p.m.
Register here for the webinar.
Dehydration: Prevention and Intervention in Long-Term Care Communities
Tuesday, Jan. 28
9:30–11:30 a.m.
Register here for the webinar.
Pressure Injury Prevention
Thursday, Jan. 30
1:30–3:30 p.m.
Register here for the webinar.
Free IDD Provider Resource Webinar Series
Free Webinars!!
June 22nd, 2025

Here Are Just Some Of Our Previously Recorded Free Webinars of Interest
Please see all recordings of previous webinars on our Gotostage Channel

Core-VA Solutions “Virtual Healthcare Assistants For LTC Programs”
Virtual Healthcare Assistants Services and Training for Long-Term Care Programs, including HCS, TxHmL, and ICF
Twogether Consulting is happy to have Brittney Russo-COO (Chief Operations Officer) from Core-VA Solutions to discuss her company’s “virtual assistant” services.
Core-VA Solutions provides virtual assistance for any type of long-term healthcare setting, whether it be for a small medical office or therapy office or HCS provider. All of our virtual assistants have a degree in nursing and/or health-related fields.
Core-VA is able to serve clients all over Texas and beyond. Some of the clients these virtual assistants work with are those in HCS, TxHmL, and also other IDD programs. This includes assisting with EVV and TMHP billing. Brittney’s team is able to provide appropriate training to her staff to cater to some of your specific needs, including persons with experience in the HCS/TxHmL programs providing some of that training and the IT solutions which they can learn to use using IT fundamentals here to learn for this. They have “virtual assistants” versed in the use of quite a few electronic health records software such as Taskmaster Pro, Focus, and other EHR and billing software. This is a wonderful resource for HCS/TxHmL providers for sure! This is especially true for some of you, who are brand-new HCS/TxHmL providers. Core-VA serves many different clients in other lines of Long-Term Health Services, but it is so nice to have help from a virtual assistant who understands the world of HCS/TxHmL!
-Core-VA team Solutions is part of our free webinar series for the month of January 2023! Click on their postcard below for more information. Services are available at $10-12/hr and no contracts.
core va post card
“Core-VA Solutions aims to positively change how your long-term healthcare facility operates with our virtual assistants with degrees in nursing and/or health-related fields. We understand that you may currently waste precious time and money completing tedious tasks such as medical reception, appointment scheduling, insurance authorization, receiving and submitting medical information, and so much more. Instead of hiring expensive employees to complete these much-needed tasks, hire our affordable virtual assistants instead, as we can provide you with the same level of service, at a fraction of the price. All you have to do is let us know how we can help, and our team will find the perfect assistant match for your facility!”
“Support & Empowerment Program For Persons With IDD & Their Caregivers”
Twogether Consulting is happy to have Diana Chavarria from AACOG discuss an amazing program offered via a grant from TCDD (Texas Council For Developmental Disabilities). This is a wonderful resource for IDD providers, Caregivers of persons with IDD and persons with IDD. Dianne is part of our free webinar series for the month of January 2023!

The Program Provides Support & Empowerment For Individuals and Their Caregivers Concerning The Following:
-General Health and Aging
-Aging With Specific Syndromes (i.e. Down Syndrome)
-Nutrition & Physical Fitness
-Financial Wellness
-Benefits and Employment
-Planning For The Future
-Mental Wellness
-Coping With A Diagnosis
-Crisis Management
Here is a link to a short, introductory video about the HRST: https://hrstonline.com/video/index.php?id=410335893
Topic: Health Risk Screening Tool
HRST (Health Risk Screening Tool) is an assessment tool that can identify & detect health risks in vulnerable populations. This tool and other services offered by HRS are based on person-centered practices. Here is a little more information about HRS from their website. The Health Risk Screening Tool (HRST) identifies and tracks health risks in vulnerable populations, making it possible to design a plan tailored to meet the unique health and safety needs of each individual in the least restrictive setting. The instrument can objectively justify resources allocated both financially and in service intensity. Used by Case Managers, supervisors, and direct support professionals. HRS also helps the provider to comply with CMS Rules and assist with Person-Centered planning and continuity of care. It is field-tested, reliable, and user-friendly
“Health Risk Screening, Inc.’s roots began in 1992. Along with training courses, webinars, and materials, HRS is the sole developer, producer, and distributor of the web-based Health Risk Screening Tool (HRST). The HRST is the most widely used and validated health risk screening instrument for people with intellectual and developmental disabilities.
HRS was established on the principles of person-centered practices. Our founder, Karen Green McGowan was a pioneer in the early formative days of the person-centered movement.. Our focus is on developing tools and training for the person-centered support of vulnerable populations. Through the education of government agencies and service providers, we have helped improve people’s lives. Along with training courses, webinars and materials, HRS is the sole developer and distributor of the web-based Health Risk Screening Tool (HRST). The HRST is the most widely used and validated health risk screening instrument for people with disabilities.”
For more information, please contact Hillary Gaytan at: Phone: 727.754.9539 Email: hilary@hrstonline.com
You can also go to their website: www.hrstonline.com
Check out this great page they have devoted to COVID-19 Resources: https://hrstonline.com/covid-19-resources/

Guest presenter:
Patrick Lane (PCT Mentor & Trainer)
From: HRS
Date: Thursday -November 12th, 2020 (Session ended)
Where: See recorded link below:
https://attendee.gotowebinar.com/recording/1049673375643527182
Topic: Person-Centered Services
Patrick will be talking about some of the Person-Centered Services offered at HRS including software that helps the provider develop Person-Centered Descriptions. These can be used as a resource for making annual plans Person-Centered by using these same person-centered skills practiced in PCT sessions.
“Person-Centered Planning Training is designed to help you approach support from a more holistic angle, with person-centered practices that respect the autonomy of those with intellectual and developmental disabilities while providing them with the highest possible level of care.”
Improve The Quality of Life
- Balancing personal choice with personal responsibility by establishing and maintaining things that are important to the person with things that are important for the person
- Being integrated in one’s community so that the person is known and respected for her or his contributions.
- Being respectfully communicated with as a person, using language consistent with being a typical adult as opposed to using clinical or system language
- Receiving support that is consistent so that new staff and others know and respect the person’s values and choices, as well as how others can help the person.
- Being matches with staff, housemates, or others that the person making life more enjoyable.
You can contact Patrick at: patrick@hrstonline.com For more info about HRS PCT services, please see the following link: https://hrstonline.com/person-centered-services/
Guest presenter:
Steve Cardie
From: Abundant Health
Date: Tuesday -November 17th, 2020 (Session ended)
Where: See link to the recorded session below:
https://attendee.gotowebinar.com/recording/5931551182568587528
Topic: Cellular Blood Pressure Monitoring System (Free To Medicare Patients!)
“Our new Cellular Blood Pressure Monitor System connects automatically to cell towers and transmits your patient’s information directly to your practice. This device makes it simple for seniors who tend to be more technology challenged to utilize Medicare’s RPM program without the difficulty of connecting to cell phones or the internet. No passwords, no Bluetooth, no internet connections required.
The rapid advance of medical device design plus an enormous upgrade in telecommunications makes Remote Patient Monitoring (RPM) suddenly possible for virtually everyone. Anywhere. In November 2018 CMS officially approved three new billing codes for Remote Patient Monitoring (RPM). The telehealth industry experts agree that this is the biggest financial incentive to date in the history of digital medicine.”
Register for the webinar at https://attendee.gotowebinar.com/register/3642654945259750160
Registration is now open! Quality in Long-Term Care Conference-August 27th -28th, 2025 (Austin, Tx)
June 23rd, 2025
HHS, in collaboration with The University of Texas Steve Hicks School of Social Work, will host an informative two-day, free conference on quality in long-term care.
The 2025 Quality in Long-Term Care Conference (QLTCC) will be held at the Renaissance Austin Hotel, Aug. 27-28, 2025.
This year’s theme is “Blazing a Trail to Quality Improvement in Long-Term Care.”
The QLTCC offers presentations from nationally and internationally recognized experts. The topics include caring for people with dementia; infection prevention and control; current heath care trends; and cutting-edge advances in long-term care, aging, and disabilities. Continuing education credits will be available for multiple disciplines. Both in person and virtual options will be available.
The Quality Monitoring Team (QMP) is committed to providing high quality information and research from top-tier speakers to those working in the long-term care community. To provide quality programming of this caliber and that our attendees have become accustomed to, including the offering of a multitude of continuing education units, we have found it necessary to begin charging a fee. We thank you for your understanding and the continued support of this program.
The QLTCC offers presentations from nationally and internationally recognized experts. The topics include:
- Caring for people with dementia.
- Infection prevention and control.
- Current heath care trends.
- Cutting-edge advances in long-term care, aging, and disabilities.
Continuing education credits will be available for multiple disciplines. Both in person and virtual options will be available. Register for the conference here: 2025 Quality in Long-Care Conference
Email UT Steve Hicks School of Social Work for more information about this event
The conference is free to attend, and continuing education credit will be available for various healthcare disciplines.
Renaissance Austin Hotel
9721 Arboretum Blvd.
Austin, TX 78759
New ICF Provider Training Available: Internal Investigations by Providers for ICFs-July 18th, 2025
June 23rd, 2025
HHSC Joint Training is presenting a new webinar for Intermediate Care Facility (ICF) providers on the internal investigation process for ICFs.
This 1.5 hour webinar provides guidance for ICF providers on conducting a required internal investigation when notified of an incident.
The first presentation of this training will be held July 18, 2025.
Register for this training at HHS Provider Joint Training Opportunities.
Register for Long-Term Care Webinars for Nurses & Nursing Facility Administrators: June 25th, 2025
June 22nd, 2025
The Quality Monitoring Program and The University of Texas at Austin School of Nursing are offering a free webinar for nurses and nursing facility administrators.
“Diving into Enhanced Barrier Precautions for Nursing Facilities,” will be hosted by epidemiologist Annie Nutt on June 25 from noon to 1 p.m. Central time.
The webinar aims to guide and improve the care of Texas residents using evidence-based best practices.
Learning objectives will include:
• Understanding the science behind enhanced barrier precautions (EBP).
• Defining and distinguishing standard precautions, contact precautions and EBP.
• Discussing best implementation practices for EBP.
This webinar provides one continuing nurse education credit for registered nurses, certified nurse aides and licensed nursing facility administrators.
For more information, email Jacki Hecht at jhecht@nursing.utexas.edu.
To register for the webinar, click here.
HHSC: HCS Amendment To Rates Effective Sept. 1, 2025
June 21st, 2025
HHSC is accepting comments on the amendment of the 1915(c) Home and Community-based Services Waiver. View the HCS amendment details.
Through this amendment, HHSC updated the attendant rates and increased the HCS individual cost limits. The cost limits were updated as described below:
-
Intermittent (LON 1), Limited (LON 5), and Extensive (LON 8)
-
The amount is going from $167,468 to 210 percent of the annualized cost of care in an Intermediate Care Facility for Individuals with an Intellectual Disability or Related Condition (ICF/IID) using the fiscal year 2026 non-state-operated small facility daily rate for Level of Need (LON) 8, rounded to the nearest dollar, which is estimated to be $169,182 pending finalization of the fiscal year 2026 rates for ICFs/IIDs.
-
-
Pervasive (LON 6):
-
The amount is going from $168,615 to 210 percent of the annualized cost of care in an ICF/IID using the fiscal year 2026 non-state-operated small facility daily rate for LON 6, rounded to the nearest dollar which is estimated to be $211,822 pending finalization of the fiscal year 2026 rates for ICFs/IIDs.
-
-
Pervasive plus (Level of Need 9):
-
The amount is going from: $305,877 to 210 percent of the annualized cost of care in an ICF/IID using the fiscal year 2026 non-state-operated small facility daily rate for LON 9, rounded to the nearest dollar which is estimated to be $392,318 pending finalization of the fiscal year 2026 rates for ICFs/IIDs.
-
Comments will be accepted until July 21, 2025.
Email comments to the Texas Medicaid Waivers inbox.
TxHmL Amendment on Rates Effective Sept. 1, 2025
June 20th, 2025
HHSC Requests Comments on TxHmL Amendment Effective Sept. 1, 2025
HHSC is accepting comments on the amendment of the 1915(c) Texas Home Living Waiver. View the TxHmL amendment details.
Through this amendment, HHSC updated the attendant rates and increased the TxHmL individual cost limit from: $17,000 to 50 percent of the annualized cost of care in an Intermediate Care Facility for Individuals with an Intellectual Disability or Related Condition (ICF/IID) using the fiscal year 2026 non-state-operated small facility daily rate for Level of Need (LON) 1, rounded to the nearest dollar which is estimated to be $31,684 pending finalization of the fiscal year 2026 rates for ICFs/IIDs.
Comments will be accepted until July 21, 2025.
Email comments to the Texas Medicaid Waivers inbox.
CLASS Program Updates
June 20th, 2025
HHSC Requests Comments on CLASS Amendment Effective Sept. 1, 2025
HHSC is accepting comments on the amendment of the 1915(c) Community Living Assistance and Support Services Waiver. View the CLASS amendment details.
Through this amendment, HHSC updated the attendant rates and increased the CLASS individual cost limit from $114,736.07 to 210 percent of the annualized cost of care in an Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Condition (ICF/IID) using the unweighted average of the fiscal year 2026 non-state operated small facility daily rates for Level of Needs (LONs) 1, 5, and 8, rounded to the nearest dollar which is estimated to be $149,774 pending finalization of the fiscal year 2026 rates for ICFs/IID.
Comments will be accepted until July 21, 2025.
Email comments to the Texas Medicaid Waivers inbox.
March 20th, 2025
CLASS Form 3621 and Instructions Update
CLASS Form 3621, CLASS or CFC – Individual Plan of Care and Form 3621-T, CLASS/CFC – IPC Service Delivery Transfer Worksheet have been updated and are now available. The effective date for the forms and forms instructions is February 2025. Click here for the new forms.
March 16th, 2025
CLASS and DBMD Quarterly Webinar Recording Available
The March 19th Community Living Assistance and Support Services (CLASS) and Deaf Blind with Multiple Disabilities (DBMD) Quarterly Webinar with HHSC Long Term Services and Supports is available.
Listen to the webinar recording.
Read the CLASS and DBMD Quarterly Webinar (PDF).
October 8th, 2024
CLASS Program Manual Revised
The Community Living Assistance and Support Services (CLASS) Provider Manual revision 24-2 updates Section 2350 and Form 3595. The revision is effective Sept. 1, 2024.
Monthly Provider Demonstration Webinars For CIMS
June 2nd, 2025
Critical Incident Management System (CIMS) Monthly Provider Demonstrations
Note: All Critical Incidents are entered into the CIMS system for HCS/TxHmL providers. FYI-ISS providers please report all critical incidents to CIIS in Tulip, not CIMS.
FEI Systems will host a monthly provider demonstration webinar on June 10, 2025, from 10–11 a.m. Monthly provider demonstration webinars are offered to providers with access to the Critical Incident Management System. HHSC encourages providers to take advantage of these live training opportunities.
This applies to:
- Community Living Assistance and Support Services providers (CLASS)
- Deaf Blind with Multiple Disabilities providers (DBMD)
- Home and Community-based Services providers (HCS)
- Texas Home Living providers (TxHmL)
- Local intellectual and developmental disability authorities (LIDDAs)
Register for the webinars by logging into CIMS and navigating to Help (top right of dashboard). Click on Help, followed by Training. Choose Register for Provider Demonstrations from the available courses.
Email MCS_CIMS@hhs.texas.gov with any questions or concerns.
Hurricane Season Training & Updating Emergency Preparedness Plans
June 1st, 2025
Hurricane Season – Ready or Not! Preparedness for HCS/TxHmL/ISS
Tuesday, June 17
10–11:30 am
Hurricane Season – Ready or Not! Preparedness for Intermediate Care Facilities
Friday, June 20
10–11:30 a.m.
Click on the following links for more training opportunities:
Individualized Skills and Socialization Training
May 18th, 2025

Planning For Flooding & Hurricane Season
** Please remember to address tornadoes in your emergency and evacuation planning, if they apply to your area, as they often occur during or in conjunction with Hurricane Season. Texas has already been hit by some severe storms, large hail, and tornadoes during the past few months. Don’t forget that May is heating up now and that severe storms and tornadoes can leave many people in Texas without electricity in incredibly hot temperatures.
See HHSC Recommendations Below:
“HHSC reminds long-term care facilities and agencies to review and update safety procedures and emergency plans for extreme weather in the 2024 hurricane season. Emergency plans for extreme weather should include the provider’s plan to address:
- Power loss.
- Water and food needs.
- Communication to families and staff.
- Staffing shortages.
- Sheltering in place and evacuation as applicable.
Providers must follow emergency preparedness rules and their own internal emergency preparedness policies and procedures.
Facilities with generators should perform any maintenance or needed testing. This will ensure the equipment functions in case of power loss.
It is important to review building integrity and identify any areas that may need repair, reinforcement or weatherproofing. Facilities in multi-story buildings should review any other needed measures as well. They should also have a plan in place for how to move residents around or out of the building if there is a loss of power or other identified need to move to a safer location.
Facilities should contact their local HHSC Regulatory Services regional office (RO) if they are impacted by an adverse event caused by severe weather — such as flooding, power loss, etc.
This communication is especially critical if a facility is projected to exceed its licensed capacity due to accepting residents that have been evacuated from another facility. All requests to exceed licensed capacity must be made through the RO and approved by the Deputy Associate Commissioner of Survey and Compliance.
Program rules require specific staff or a designee of each program to register with the emergency communication system and respond to requests through the emergency communication system. Please refer to PL 2025-01 (PDF) for instructions and more information regarding the emergency communication system requirements.
For training opportunities related to emergency preparedness for long-term care providers visit the HHSC Provider Training webpage.

BEHAVIORAL SUPPORT SERVICES PROVIDER POLICY TRAINING
 Behavioral Support Services
Behavioral Support Services
HCS and TxHmL Behavioral Support Services Provider Policy Training
(Has been mandated for HCS & TxHmL providers to ensure their contracted Behavioral Support Services providers to take since March 2015)
This course informs service providers of behavioral support services in the HCS and TxHmL programs related to the provision of behavioral support services in those programs. All new behavior support service providers must complete the WBT before providing services to an individual. All providers must complete the course every three years.
***To document successful course completion, participants must print a copy of the certificate provided at the end of the training and submit a copy to a program provider with whom they are employed or contracted.
Ensure Medicaid Continues To Support Individuals With IDD
May 31st, 2025
Please help ensure Medicaid continues to support Individuals in Texas with IDD. More than ever, we need everyone to focus their efforts on contacting our U.S. Senate representatives.
Call Senator John Cornyn (1-202-224-2934) and Senator Ted Cruz (1-202-224-5922) to continue to ensure we have Medicaid to support programs serving individuals with IDD, as well as directly support individuals with IDD in Texas.
The ARC of TEXAS has supplied a nice script for you, or your person with a disability to contact these senate representatives and share your concerns, issues, and need for Medicaid for services:
“Hi, my name is [NAME] and I live in [CITY]. I am a [Texan with a disability / family member of someone with an intellectual or developmental disability]. Medicaid is essential for [me/my family member] to live independently and access the services we need. Without Medicaid, [I/my family member] would not be able to receive critical support such as help with daily activities, therapies, job support, and community integration. Please do not cut funding for Medicaid. It allows [me/my family member] to live in the community, access education and employment opportunities, and fully participate in society. Thank you for your time, and please support Texans with disabilities like [me/my loved one].”
Bill Creating “Building Better Futures Program” Signed Into Law By Governor Abbott
May 30th, 2025
Governor Abbott signed House Bill 2081, officially creating the Building Better Futures program into law on May 26th, 2025.
This will be a step toward a more inclusive and accessible future for all Texans, including those with disabilities.
Rep. John Bucy III authored the bill, and it was sponsored by Senator José Menéndez. This law takes effect immediately and establishes a grant program within the Texas Higher Education Coordinating Board (THECB) to support colleges and universities in developing and expanding Comprehensive Transition and Postsecondary (CTP) programs across the state. CTP programs provide inclusive higher education opportunities for students with intellectual and developmental disabilities (IDD), and will ensure what is hopefully equitable access to postsecondary education and career pathways.
*As of now, only four CTP programs operate in the entire state.
Now that the bill has been signed into law, the THECB is charged with implementing the program and developing rules and policies necessary to administer this program effectively. We hope to keep you posted on developments as they occur.
Special Needs Attorney and Planning Webinar June 10th, 2025 Noon Central : Presented By Consolidated Planning Group
May 29th, 2025


The Team at Consolidated Planning Group
Greater Inclusion of Children with Disabilities in Early Education Program-Major Bill Passes
May 26th, 2025
As of May 25th, 2025, the House and Senate have passed a bill that will create a plan for greater inclusion of children with disabilities in early education programs.
The Texas Senate gave final passage to House Bill 2310. The bill was authored by Rep. Claudia Ordaz and sponsored by Senator Tan Parker. It would require the TEA (Texas Education Agency), TWC (Texas Workforce Commission), and HHSC (Health and Human Services Commission) to develop a strategic plan to increase the inclusion of children with disabilities in public early childhood education programs.
It is now left up to Governor Abbott for consideration.
IDD Operations Portal Enhanced View Training: May 23rd & May 28th, 2025
May 22nd, 2025
IDD Operations Portal (IDD Ops Portal) Administrators will provide a brief overview of the new and enhanced view of the system.
Attendees are recommended to attend either session as they provide the same information.
Register for the May 23rd IDD Operations Portal
Enhanced View Training 11 a.m. to 12 p.m.
OR
Register for the May 28th IDD Operations Portal Enhanced View Training 2 p.m. to 3 p.m.
Topics include:
- Initial and single user account setup
- Navigation of new portal view
- Types of list views
The webinar will include a handout outlining the new IDD Ops Portal enhanced view. Attendees will receive a copy of the presentation before the webinar starts.
Email questions to idd_ops_portal@hhs.texas.gov.
HHSC has published Information Letter 2025-09 IDD Operations Portal (IDD Ops Portal) Transition to Enhanced View. This letter provides information on the overview of changes in the new enhanced view of IDD Ops Portal.
On Monday, June 2, 2025, the web address, appearance, and tab navigation for the IDD Ops Portal will change.
You may still navigate to the existing web address to log in, and you will be redirected to the new web address: https://ithhs.my.site.com/.
HCBS-Adult Mental Health Program: CBT Trainings
May 20th, 2025
Home and Community-Based Services – Adult Mental Health Program
CBT trainings
- Home & Community-Based Services – Adult Mental Health (contains provider training and resource information)
- Adult Mental Health Home & Community-based Services
Other information about the program:
Frequently Cited Deficiencies-HCS/TxHmL/ICF
May 20th, 2025
These are the most recent postings from HHSC, hopefully, those for 2024 will be posted soon,
Home and Community-based Services
- 10 Most Frequently Cited Deficiencies in Home and Community-based Services (HCS) & Texas Home Living (TxHmL) — Fiscal Year 2023 (July 16, 2024)
Texas Home Living
- 10 Most Frequently Cited Deficiencies in Home and Community-based Services (HCS) & Texas Home Living (TxHmL) — Fiscal Year 2023 (July 16, 2024)
Intermediate Care Facilities
Texas Parks & Wildlife Explore Webinar: New Initiatives Focusing on Accessibility & Inclusivity
May 18th, 2025
From HHSC Deat & Hard of Hearing Services:
“Join the Texas Health and Human Services Commission Deaf and Hard of Hearing Services for EXPLORE!, a webinar presented by the Texas Parks and Wildlife Department (TPWD) Accessibility Team. Discover the latest updates and initiatives across Texas public lands, focusing on accessibility and inclusivity. From camping in a state park to touring a fish hatchery or renewing your hunting license at a law enforcement office, TPWD is committed to outdoor access for all Texans and is making strides every day to increase accessibility to facilities, programs, and services.
Learn about the different programs offered by the agency, including boating education, learn-to-hunt programs, camping, and online education opportunities you can enjoy from home. TPWD staff will share resources for visitors with disabilities and demonstrate how to navigate the TPWD website to find the information you need to visit.”
When: Tuesday, May 27, 2025, 11:30 a.m. – 1:00 p.m.
Presented by: Cole Johnson, Accessibility Training Specialist, Texas Parks and Wildlife Department
To register, click here or scan the QR code below.
During this session, TPWD will highlight accessible facilities and outdoor spaces and discuss the role that accessibility plays in new parks and projects. Get information on adaptive equipment and all-terrain wheelchairs, making modification requests, and employment and volunteer opportunities that allow you to make a difference in our parks and beyond.
Make sure that you have everything you need to make an informed decision about visiting a TWPD facility and participating in a program.
This webinar will be presented in spoken English; CART (captioning) and ASL/English interpretation will be provided.
Certificates of Attendance will be awarded to attendees that may be used for continuing education documentation. In addition, participants may earn 0.15 DHHS CEUs (accepted by BEI).
Email questions to DHHS Training & Education.

Employment Readiness Updates
May 17th, 2025
New Employment Readiness Assessment Tool
On January 1, 2025, the Health and Human Services Commission (HHSC), implemented the new employment readiness benefit available to individuals enrolled in the Home and Community-based Services (HCS), Texas Home Living (TxHmL), or Deaf Blind with Multiple Disabilities (DBMD) waiver programs for individuals with intellectual or developmental disabilities. HHSC is required to assess all settings where employment readiness is provided for compliance with federal Home and Community-Based Services (HCBS) Settings requirements at 42 CFR 441.301(c)(4) before employment readiness can be provided in the setting.
All settings not previously assessed for compliance with the HCBS Settings Rule must conduct a self-assessment using the Employment Readiness Self-Assessment tool and submit it to Medicaid_HCBS@hhs.texas.gov for review and approval before providing employment readiness.
This tool is now available to providers at Employment Readiness Provider Self-Assessment Tool: HCBS Settings Rule Compliance. See Information Letters 2025-05 and 2025-01 for more details.
March 30th, 2025
Additional Information on HCBS Settings Rule Compliance for Employment Readiness Providers
HHSC has published Information Letter 2025-05 with additional information concerning Employment Readiness (ER). This letter provides information for financial management services agencies (FMSAs), local intellectual and developmental disability authorities (LIDDAs), and providers of Deaf Blind with Multiple Disabilities (DBMD), Home and Community-based Services (HCS) and Texas Home Living (TxHmL) services regarding the steps to ensure compliance with the HCBS settings rules for settings where employment readiness services are provided.
An on-site visit is required to beassessed for compliance with HCBS settings compliance rules, before providing ER services.
Current Individualized Skills and Socialization Providers In 2023, HHSC’s Contract Administration and Provider Monitoring (CAPM) staff conducted on-site visits to individualized skills and socialization provider settings to assess for compliance with HCBS Settings requirements (IL 2023-28). Providers previously assessed by CAPM staff for compliance with the HCBS Settings requirements do not need to be reassessed before the provider delivers employment readiness services in the same setting. Appropriate evidence of compliance is an email from HHSC confirming compliance. Providers who have been assessed but did not receive confirmation of compliance may reach out by email to Medicaid_HCBS@hhs.texas.gov using the subject heading: “Employment Readiness Request for Confirmation of Settings Compliance.”
If the provider of ER has not already had CAPM staff conduct an on-site visit, then they will have to complete a “self-assessment”, submit it, and then have an on-site visit to check for HCBS settings compliance.
First the ER provider must complete the self-assessment prior to the on-site visit and submit the self-assessment along with policies and other requested documents. The provider should conduct a self-assessment using the HHSC-developed assessment tool. The tool can be obtained by emailing Medicaid_HCBS@hhs.texas.gov using the subject heading “Request for Employment Readiness Self-Assessment.”
March 20th, 2025
Employment Readiness Q&A with Examples Document
HHSC has published the Employment Readiness Questions & Answers with Examples Document for Local Intellectual and Developmental Disability Authorities (LIDDAs), Deaf Blind with Multiple Disabilities (DBMD), Home and Community-based Services (HCS) and Texas Home Living (TxHmL) Programs. The document provides answers to questions about employment readiness and examples of scenarios that differentiate between employment readiness, individualized skills and socialization and employment assistance services.
January 14th, 2025
HHSC Publishes Information on Implementation of Employment Readiness
Note: The previous publication had a broken link. Please find the correct link below.
HHSC has published Information Letter 2025-01 Implementation of Employment Readiness. This letter provides a description of employment readiness and guidance related to the implementation of the new service.
***Don’t forget, the IPC form for TxHmL and HCS have been updated to include Employment Readiness Link to TxHmL form 8582 and Link to HCS form 3608 IPC
December 1st, 2024
New Service: Employment Readiness is available in the following waiver programs: HCS, TxHmL, and DBMB
As required by House Bill 4169 (88th Legislature, Regular Session, 2023), the Health and Human Services Commission (HHSC) is adding a new service similar to prevocational services to the Home and Community-based Services (HCS), Texas Home Living (TxHmL), and Deaf Blind with Multiple Disabilities (DBMD) waivers. The new service, employment readiness, will be available on Jan. 1, 2025.
Employment Readiness and Provider Fiscal Compliance Review Process Webinar
HHSC will host a webinar on Dec. 11 from 10 a.m. to noon for the Home and Community-based Services (HCS), Texas Home Living (TxHmL), and Deaf Blind with Multiple Disabilities (DBMD) program providers, local intellectual and developmental disability authorities, financial management service agencies and other interested parties.
The webinar will provide information on the new:
- Employment readiness service coming to the HCS, TxHmL and DBMD Programs on Jan. 1, 2025.
- Provider fiscal compliance review process in the HCS and TxHmL Programs, effective on Jan. 1, 2025.
Email questions about the webinar to your program policy:
What’s Employment Readiness?
Employment readiness provides assistance that prepares an individual for employment in the community. It helps an individual develop basic habilitative skills or achieve generalized vocational goals. Employment readiness activities cannot be directed at developing skills related to a specific type of employment.
Maintaining Records: Your Responsibility As A Provider
May 16th, 2025
In accordance with 26 TAC §52.113 (relating to Record Retention and Disposition) and the requirements of the Community Services Provider Contract or Provider Agreement, all records must be developed and retained in the form in which they were created until the latest of the following:
- seven (7) years after a claim is submitted;
- seven (7) years after all issues involving the record have been mitigated; or
- the individual about whom the record relates becomes 21 years of age.
If a contract is expiring or being terminated, the provider must adhere to 26 TAC §52.601 (relating to HHSC Review and Contractor Requirements Related to Expiring or Terminated Contract) and 26 TAC §52.113 (relating to Record Retention and Disposition) until the record retention period is satisfied.
Important: Providers are required to report the location of where the records will be stored and provide the name, address, phone number, and e-mail address of a person HHSC may contact to arrange access to the records. This information must be submitted to the assigned HHSC contract manager at the time of expiration, termination, when an update is necessary, or upon request.
IDD and PI Quarterly Webinar with HHSC LTCR (HCS & TxHmL Providers)
May 16th, 2025
April 30 IDD and PI Quarterly Webinar with HHSC LTCR Recording Available
The April 30 recording of the Intellectual and Developmental Disability (IDD) Programs and Provider Investigations (PI) Quarterly Webinar with Long-term Care Regulation is available.
Listen to the IDD and PI Quarterly Webinar recording.
Read the IDD and PI Quarterly Webinar (PDF).
Email LTCR Policy for the transcript.
Future Webinar Dates
July 30, 2025
Oct. 29, 2025
February 12th, 2025
IDD and PI Quarterly Webinar with HHSC LTCR Recording Available
The Jan. 30 recording of the Intellectual and Developmental Disability Programs (IDD) and Provider Investigations (PI) quarterly webinar with Long-term Care Regulation (LTCR) is available.
Listen to the webinar recording.
November 13th, 2024
IDD and PI Quarterly Webinar with HHSC LTCR Recording Available
The Oct. 31 recording of the Intellectual and Developmental Disability Programs (IDD) and Provider Investigations (PI) quarterly webinar with Long-term Care Regulation (LTCR) is available.
Listen to the webinar recording.
Read the IDD and PI Quarterly Webinar (PDF).
Email LTCR Policy for the transcript.
October 30th, 2024
IDD and PI Quarterly Webinar with HHSC LTCR
HHSC Long-term Care Regulation will host a webinar for Individualized Skills and Socialization, HCS and TxHmL providers regarding the latest information from LTCR.
Those using Internet Explorer may have difficulties registering for the webinar. If so, try using another browser, such as Google Chrome or Microsoft Edge.
IDD/PI Quarterly Webinar
Oct. 31, 2024
3:30–4:30 p.m.
Register for the webinar.
IDD Conferences & Conventions 2025
May 15th, 2025

-
AAIDD Annual Meeting- The American Association on Intellectual and Developmental Disabilities (AAIDD) will hold its 149th annual meeting from June 23-25 inWashington D.C. This conference will focus on mentorship, access, equity, and collaboration in the IDD field.
- Texas State Chapter of AAIDD Convention- Takes place Sept. 29th-Oct. 2nd in Corpus Christi, Tx
-
CR Unite Autism and IDD Care Conference-Hosted by CentralReach, this conference for therapy providers, special educators, and supported employment agencies will be held October 20-22 inChicago, IL
-
One Voice Conference: Hosted by The American Academy of Developmental Medicine and Dentistry (AADMD) will host this conference June 5-8 inPhoenix, Arizona The theme is “Rising Phoenix: A New Era in IDD Health” and will cover topics like inclusive curriculum, intersectionality, brain & behavioral health, and clinical practice.
-
Pacific Rim International Conference on Disability and Diversity-Celebrating its 40th anniversary, this conference will be held April 15-16 inHonolulu, Hawaii
-
National Centre of Excellence in Intellectual Disability Health Conference- This conference will take place in Sydney, Australia and online, with the theme “Working together every step of the way”.
-
Global Disability Summit- Co-hosted by Germany, Jordan, and the International Disability Alliance (IDA), this summit took place April 2-3 in , Germany.
-
International Conference on Intellectual and Developmental Disabilities (ICIDD)- Organized by the World Academy of Science, Engineering and Technology, this conference will be held September 20-21 inLisbon, Portugal
.
-
DADD Conference- The Division on Autism and Developmental Disabilities (DADD) of the Council for Exceptional Children (CEC) will hold its 26th annual international conference January 22-24 inClearwater Beach, Florida
.
-
IASSIDD Congress- The International Association for the Scientific Study of Intellectual and Developmental Disabilities (IASSIDD) will host its congress inSingapore with the theme “Person-centricity as an approach to well-being of People with Intellectual and Developmental Disabilities”.
-
National Centre of Excellence in Intellectual Disability Health Conference- This conference will be held in Sydney, Australia and online.
- Aging and Developmental Disabilities Conference: The 34th annual conference will be held May 12-13 in St. Louis, MO
-
Developmental Disabilities Awareness Day Conference- This conference will take place on May 20 in Niagara Falls, NY.
-
Evidence for Success Disability Conference- This conference will be held June 22-24 in Chandler, Arizona
.
Interagency Reportable Conduct Search Engine: Informal Comments Deadline For Draft Rules
May 15th, 2025
Deadline for Informal Comments: May 30
Texas Health and Human Services Commission (HHSC) is accepting comments from stakeholders on the following draft rules related to an interagency reportable conduct search engine. The comment period ends May 30, 2025.
- Texas Administrative Code, Title 26,
- Chapter 550,
- Chapter 551,
- Chapter 553,
- Chapter 554,
- Chapter 555,
- Chapter 556,
- Chapter 557,
- Chapter 558,
- Chapter 559,
- Chapter 560,
- Chapter 565, (HCS) and
- Chapter 566 (TxHmL), concerning Long-Term Care Regulation (LTCR) Interagency Reportable Conduct Search Engine.
Questions and comments can be emailed to HHSC LTCR Rules.
Cost Report For 2024 & 2025 Accountability Report Training Information
May 6th, 2025
Additional Cost Report Training for HCS/TxHmL and ICF/IID or Related Conditions
The HHSC Provider Finance Department (PFD) has scheduled an additional 2024 Cost Report Training for Home and Community-based Services/Texas Home Living (HCS/TxHmL) and Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) on Wednesday, May 7, 2025, at 9 a.m.
Register here for this training or visit the HHSC PFD Cost and Accountability Report Training webpage to register.
December 15th, 2024
HHSC has published the Information Letter (IL) 2024-XX regarding the 2024 Cost Report and 2024 or 2025 Accountability Report Training Information.
Information on Cost and Accountability Report Training Information can be accessed on the Provider Finance Department’s (PFD) webpage.
Review the IL for more information. If you have further questions, contact PFD-LTSS@hhs.texas.gov or (737) 867-7817.
LTC Provider Bulletin Now Available
May 5th, 2025

The May 2025 Long-Term Care (LTC) Provider Bulletin has been published on the LTC homepage on TMHP.com.
Visit the TMHP LTC homepage regularly for news, reminders, training opportunities, and other important program updates.
February 15, 2025
The February 2025 Long-Term Care (LTC) Provider Bulletin has been published on the LTC homepage on TMHP.com.
Recording Of April 24th DAHS and ISS Webinar with LTCR
May 4th, 2025
A recording of the April 24 DAHS and Individualized Skills and Socialization provider webinar with HHSC Long-term Care Regulation is now available. The presentation (PDF) is also available.
Listen to the webinar recording.
Email LTCR Policy for a transcript.
HCS Handbook Revision 25-1
May 4th, 2025
The HCS Handbook Has Been Revised
The Home and Community-based Services (HCS), Handbook revision 25-1, updates Section 11000.
11000, Maintaining Medicaid Eligibility
Financial Eligibility Guidelines for Texas Home Living and Home and Community-based Services
This revision is effective April 29, 2025. Review the updates linked here.
November 26th, 2024
The HCS Handbook Has Been Revised
The Home and Community-based Services (HCS) Handbook revision 24-1 updates Appendix X.
This revision became effective Oct. 1, 2024. Click this link to see the updates.
Local Intellectual and Developmental Disability Authority Handbook (LIDDA) 24-4 Revision
May 3rd, 2025
The LIDDA Handbook Has Been Revised
The Local Intellectual and Developmental Disability Authority (LIDDA) Handbook, revision 25-3, updates form references.
This revision is effective May 1, 2025. Review the updates linked here.
February 26th, 2025
The LIDDA Handbook Has Been Revised
The Local Intellectual and Developmental Disability Authority Handbook (LIDDA) revision 25-2 updates sections 19220, 19230 and Form 8591.
This revision is effective Feb. 26, 2025.
Click this link to see the updates.
February 7th, 2025
The LIDDA Handbook Has Been Revised
The Local Intellectual and Developmental Disability Authority (LIDDA) Handbook revision 25-1 updates Sections 4000, 4100, 4200, 4300, 4400, 17000, 17100, 17200, 17300, 17400, 17500 and Resources.
This revision is effective Jan. 28, 2025.
Click this link to review the updates.
November 16th, 2024
The LIDDA Handbook Has Been Revised
The Local Intellectual and Developmental Disability Authority (LIDDA) Handbook revision 24-4 updates Appendix V.
This revision is effective Nov. 16, 2024. Click this link to see the updates.
October 7th, 2024
The LIDDA Handbook Has Been Revised
Local Intellectual and Developmental Disability Authority Handbook (LIDDA) 24-3 revision updates sections throughout the handbook.
The revision is effective Sept. 30, 2024. Click here for a full-size view of the updates.
| 12000 | Protocol for Offering an HCS Crisis Diversion Slot | Updates language for clarity. |
| 12100 | Purpose | Updates reference to Section 12300.
Updates language for clarity. |
| 12300 | Qualifications for the HCS Reserved Capacity Group for Crisis Diversion | Changes title to Criteria for Requesting an HCS Reserved Capacity Group Crisis Diversion Slot.
Changes language in first paragraph about how a person meets the criteria for the LIDDA to request an HCS Reserved Capacity Group Crisis Diversion slot. Removes language in fourth bullet about ICF/IID LOC I criteria, replaces it with how a person meets the criteria for LIDDA priority population per Title 26 Texas Administrative Code (TAC), Section 304.102, Diagnostic Assessment. Updates the Note to require persons to meet the diagnostic and financial criteria specified in 26 TAC Section 263.101, Eligibility Criteria for HCS Program Services and CFC Services to enroll in HCS. Updates language for clarity. |
| 12400 | Process | Removes language about ICF/IID LOC I criteria and adds language that requires a person to meet the criteria for LIDDA priority population per 26 TAC Section 304.102, Diagnostic Assessment.
Adds information about Form 1058 and submission. Removes requirements to submit a packet with a Determination of Intellectual Disability (DID) and Inventory for Client and Agency Planning (ICAP) booklet/scoring sheet. Updates HCS Program TAC reference to 26 TAC Section 263.104. Updates language for clarity. |
AAIDD: Annual National Conference 2025
May 1st, 2025
Annual National AAIDD Conference 2025
Washington D.C.
July 23rd-25th, 2025
General Registration
Conference Registration includes:
- Pre-Conference Sessions
- Featured plenary presentations
- More than 100 educational presentations were organized into Concurrent Sessions, Issue Briefs, Poster Symposia, and Poster Presentations
- Awards Breakfast
- Sunday night President’s Reception
- Exhibit Hall Tuesday’s Continental Breakfast and Breaks
- Posters, Publications, and SECP Receptions
Registration Includes: All conference sessions and exhibits will take place at the Crystal Gateway Marriott Hotel. We encourage you to stay at our conference hotel because it will be convenient to you and it helps keep the meeting costs as low as possible. Note that AAIDD and/or Crystal Gateway Marriott will NOT contact you to offer to assist you in making hotel reservations. The only two ways to reserve a hotel room under our special group rate are by booking online using the customized link below or by calling the hotel directly
Hotel Information: Crystal Gateway Marriott
“Caytlin Handley Act”-House Bill 1188
April 25th, 2025
“Caytlin Handley Act”
On April 8, the House Committee on Public Education heard House Bill 1188, filed by Rep. Christian Manuel.
This bill would require school districts to provide families of students identified as eligible to receive special education services due to a diagnosis of IDD or developmental delay to their (LIDDA), ensuring students and families are informed about Medicaid waiver programs, long-term services and supports, and other community resources.
From the ARC of Texas Legislative Newsletter April 18th, 2025 Edition
“The Handley Family of Katy, Texas—Caytlin, Carey, and Boyd—have championed this bill from the start, using their voices and lived experience to lead the charge for better access to information and services for families of students with disabilities. In recognition of Caytlin’s advocacy, Rep. Harold Dutton Jr. motioned to rename the bill the “Caytlin Handley Act,” and in a rare and powerful moment, the committee voted to advance the bill immediately following testimony from the Handley family and supporters, including The Arc of Texas.”
WATCH the testimony (see timestamps of interest below).
- Rep. Manuel lays the bill out: 15:23
- The Handley Family testifies: 19:46
- Carey testifies: 20:27
- Caytlin testifies: 22:13 and 25:37
- Boyd testifies: 22:52
- Motion by Rep. Dutton: 46:23
Provider Job Openings & Employment Opportunities: HCS/ICF/ISS

Job Position
Lone Star HCS (Conroe, Tx)

Job Position: Host Home/Companion Care Service Provider
Please see information below and contacts to respond.
Looking for Host Home/Companion Care provider who wants to care for 3 young men, 2 of which are fairly independent. The 3rd individual needs a bit more help with hygiene and meal preparation. The host home is located in the Woodlands, Texas area near Conroe and Houston. If you are interested in the position, please contact Rhonda Wilson for more details.
Note: You would not be using your own home. The home would be provided by one of the individual’s family members, for the host home/companion care provider to rent along with the individuals they are caring for.
Rhonda Wilson (Program Director/Provider Coordinator)
936-777-2028 (Phone) 936-228-7641 (Fax)
March 1st, 2025
The Harris Center for Mental Health and IDD
Job Position Now Available: Program Director V, Residential & Day Services.
Please see information about the position below. We have also provided a link you may click on to apply.
**Note, this position is on page 2.
The Harris Center is now accepting candidates and will begin scheduling interviews this week. If you know any interested parties, please feel free to share.
I believe this position will be with their internal ICF/IID program
Based on the many phone calls, emails, and contacts through our social media pages concerning employment needs and job openings in the HCS/ICF/ISS programs, we will continue to use our “Updates” page as a platform to assist providers in posting these openings and opportunities.
If you contact Meghan Jones at meghanjones.tx@gmail.com and let her know where you are posting a position and who to contact, we can also just put a link and the contact person’s name, # and/or email for free at no cost. For example, you are posting on Indeed, Linkedin, BenefitMall, Facebook, PACSTX job postings, an online newspaper, etc… If you would like to post an opening with a complete job description (or longer than a few paragraphs), the cost is $15 for a one-time fee. We will continue to run this post until you notify us otherwise. All current updates are also noted in our bi-weekly newsletter.
We will also continue to repost openings when we can on our Linkedin page as well as our Facebook and Instagram pages for Twogether Consulting.
There is no charge, we just ask you all to keep referring us to others who don’t know about us for their IDD program needs and of course, we hope you will continue to use our services to assist you with your training needs, on-site and off-site assistance.
Julie Blacklock/ Owner
CFC Proposed Billing Requirements (HCS/TxHmL)-Drafts
April 15th, 2025
The proposed billing requirement revisions and a summary of changes are located on the Long-term Care Providers webpage and are outlined below:
HCS
PEMS Provider Credentialing Process Update As Of May 30th, 2025
April 15th, 2025
Beginning May 30, the Provider Enrollment and Management System (PEMS) will be enhanced to streamline the process for Texas Medicaid enrollment, managed care organization (MCO) and dental maintenance organization (DMO) credentialing.
PEMS will feature a new Credentialing Tab for the credentialing application that will allow providers to complete and submit their credentialing information as part of the enrollment process, the reenrollment process, or as a maintenance request.
For more information, refer to Coming Soon: PEMS to Be Updated to Allow Provider Credentialing on TMHP’s Provider Enrollment webpage.
Texas Council on Developmental Disabilities News This Week
April 15th, 2025
From our friends at Texas Council on Developmental Disabilities:
IDD Coordinating Council
TCDD Senior Public Policy Analyst Lauren Gerken provided verbal testimony on March 25 to the House Human Services Committee on House Bill (HB) 2807, which would establish a statewide intellectual and developmental disability (IDD) coordinating council. She discussed how this new council would bring multiple agencies together to develop strategies on optimizing the complex system of Medicaid waivers, education, and more. The council would also ensure implementation and proper oversight of a five-year statewide IDD strategic plan. Gerken detailed how this new council would differ from other state disability entities (PDF) such as TCDD and the Texas Governor’s Committee on People with Disabilities. HB 2807 was featured as a TCDD Bill of the Week.
Soft-Skills Training
Gerken also gave verbal testimony on March 25 to the House Subcommittee on Workforce on HB 1147, which would require the Texas Workforce Commission to establish a workplace soft-skills training pilot program. Gerken said that, while the bill is not specifically related to disability, it could allow people with disabilities to gain a certificate for soft skills that they were unable to qualify for previously. The bill would also give people with disabilities an opportunity to engage in the workforce in a more meaningful way to increase their employability.
Resources to Contact Lawmakers and Give Testimony
The House Research Organization recently published its list of legislative staff (PDF, 28 pages, 3.9 MB) for the 89th Legislature. The document provides the names and titles of staff in lawmaker and committee offices, both for the House and the Senate. It is a helpful tool for making initial contact with staff, or for following up after you’ve spoken with an office.
If you’d like to give remarks at an upcoming hearing but aren’t sure how to craft your comments, we’ve created a My Testimony Blueprint (PDF) that can be used as a guide. For more legislative advocacy resources, visit our website.
HB 1936 would strengthen the enforcement of accessible parking violations. It was authored by Rep. David Cook.
**For More information from TCDD or to subscribe to their newsletter please click on this link: TCDD
Notification of Intergovernmental Transfer -2nd Qtr. 2025 Payment-ICF UPL Program
April 12th, 2025
HHSC is providing notification of the Intergovernmental Transfer (IGT) call for the Intermediate Care Facilities Upper Payment Limit (ICF UPL) 2Qtr2025 payment.
The federal fiscal year 2025 ICF UPL Quarterly Payments file was updated on April 15, 2025, and can be found on the Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) UPL Supplemental Payment Program website. IGT amounts due are in Column J, under the “2nd Quarter Maximum IGT” heading.
Below are the pertinent dates associated with the 2025 ICF UPL 2nd Qtr. 2025 Payment:
- May 7, 2025: Last date to schedule transfer in TexNet.
- May 8, 2025: IGT Settlement Date.
- May 28, 2025: Payments expected to be released by the Comptroller.
Select the ICF UPL bucket in TexNet when you enter your IGT. Funds should be transferred through TexNet using the TexNet instructions. After transferring funds, send a screenshot or PDF copy of the confirmation or trace sheet from TexNet to the Provider Finance Department Payments Team.
Updates on Budget Proposals For IDD Services
April 10th, 2025
Resource Links:
Consideration of the budget as well as HB 500, the supplemental budget, by the House will occur today at 9:00am, Thursday, April 10th.
HB 500 (supplemental): https://www.capitol.state.tx.us/tlodocs/89R/billtext/pdf/HB00500H.pdf#navpanes=0
House Rules Adopted related to Consideration of the Budget: To view the rules adopted by the House on April 2, 2025 related to consideration of the budget (SB 1), see pages 2 – 4 at the following link:
https://journals.house.texas.gov/hjrnl/89r/pdf/89RDAY37FINAL.PDF#page=2
Link to Watch Today’s Debate: Though the House proceedings on the budget and HB 500 will make for a long day, interested persons may view at: https://house.texas.gov/videos
Representative Donna Howard’s Proposed Accountability Amendment to Rider 23:
This amendment adds the provision below to Rider 23 which parallels the same provision in the Senate Rider. However, unlike the Senate Rider 23 which requires HHSC to create list of providers whose calculated direct care staff wage and benefits expense ratio is less than 0.95 and submit to certain legislative offices, Howard’s amendment sets it at less than 0.90.
(c) Out of funds appropriated in Strategy B.1.1, Medicaid & CHIP Contracts and Administration, HHSC shall continue to collect biennial cost reports from providers to monitor the average hourly wage and associated payroll costs, taxes, and benefits.
HHSC shall calculate for each provider the total amount that was paid to the provider that is attributable to the direct care wages, payroll costs, taxes, and benefits, the amount expended by the provider for that purpose, and the ratio of expenses to revenue to determine a direct care wage and benefits expense ratio. HHSC shall report to the Legislative Budget Board, the Lieutenant Governor, the Speaker of the House of Representatives, and the Office of the Governor on an annual basis by November 1 of each year on the findings, including a list of providers whose calculated direct care staff wage and benefits expense ratio is less than 0.90.
ISS Updates & New Rules (HCS/TxHmL)
April 6th, 2025
Register Now for April 24 DAHS and Individualized Skills and Socialization Provider Webinar with HHSC LTCR
HHSC Long-term Care Regulation will host a webinar for Day Activity and Health Services (DAHS) and Individualized Skills and Socialization providers on April 24 from 11 a.m. to noon.
DAHS and Individualized Skills and Socialization providers should attend this and all webinars with HHSC LTCR.
LTCR will provide the latest updates and answer questions from participants.
October 26th, 2024
HHSC Publishes Revised PL 2023-01
HHSC has published revised Provider Letter 2023-01 New Regulatory Rules for Long-term Care Regulation (LTCR) Individualized Skills and Socialization Services.
Revisions include information regarding the issuance of temporary initial licenses to applicants for DAHS-Individualized Skills and Socialization Only licensure, clarification on capacity, LTCR surveys, Form 3613-A requirements, emergency response plan requirements, and updates to contact information for TULIP Support.
September 9th, 2024
HHSC Publishes PL 2024-15: Return To Temporary Licensure for DAH’s ISS Only Providers
HHSC has published Provider Letter 2024-15 Temporary Initial Licensure for DAHS-Individualized Skills and Socialization Only Providers.
Beginning September 9th, 2024, HHSC will resume issuing temporary initial licenses to DAHS-Individualized Skills and Socialization Only providers prior to conducting a health survey.
May 5th, 2024
UPDATED ISS FAQ’S
- Pages 18, 21 & 24
- Pages 32, 33, and 36 thru 39
- Pages 41, 57 & 58,
- Pages 63, 68, 71, 73 and 75 thru 80.
HHSC Long-term Care Regulation updated the Individualized Skills and Socialization frequently asked questions document on May 2, 2024.
April 1st, 2024
ISS Administrative Penalties Scope and Severity Grid
Figure: 26 TAC §559.253(b)
| SCOPE AND SEVERITY GRID FOR ADMINISTRATIVE PENALTIES | |||
| ISOLATED | PATTERN | WIDESPREAD | |
| Immediate threat | Substantial=NRTC | Substantial=NRTC | Substantial=NRTC |
| J | K | L | |
| Initial | $400–$600 | $450–$650 | $500–$700 |
| Repeat | $500–$700 | $550–$750 | $600–$800 |
|
Actual harm |
Substantial=NRTC | Substantial=NRTC | Substantial=NRTC |
| G | H | I | |
| Initial | $250–$450 | $300–$500 | $350–$550 |
| Repeat | $350–$550 | $400–$600 | $450–$650 |
|
No actual harm with a potential for more than minimal harm |
Non-Substantial=RTC | Non-Substantial=RTC | Substantial=NRTC |
| D | E | F | |
| Initial | $100–$300 | $150–$350 | $200–$400 |
| Repeat | $200–$400 | $250–$450 | $300–$500 |
|
No actual harm |
Non-Substantial=RTC | Non-Substantial=RTC | Non-Substantial=RTC |
| A | B | C | |
| Initial | $0–$0 | $0–$0 | $0–$0 |
| Repeat | $0–$0 | $0–$0 | $0–$0 |
March 18th, 2024
New Rules For ISS
PL-2023-01(Revised)
https://www.hhs.texas.gov/sites/default/files/documents/pl2023-01.pdf
March 7th, 2024
HHSC Hold Harmless Period Ending
This “hold harmless” period is ending for ISS providers on March 17, 2024.
Beginning March 18, 2024, HHSC will survey for compliance with all regulatory requirements, including off-site provision of services, and move forward with applicable enforcement actions as outlined in Title 26 Chapter 559, Subchapter H, Division 4 (Survey, Investigations & Enforcement)
Draft Amendments to ISS Licensing Rules
February 14th, 2024
Delays In Receiving ISS Licenses
December 15th, 2023
Clarification on Licensure Renewals
All licensed long-term care providers must submit a renewal application in the Texas Unified Licensure Information Portal (TULIP) before their current license expires. While a re-licensure/recertification survey is part of the renewal process, it doesn’t take the place of submitting a renewal application in TULIP.
HHSC encourages providers to submit the application as soon as possible within the 120 days prior to the expiration of their license, so that if there are issues with TULIP — such as the renewal application not being in the TULIP account — the provider has time to work with TULIP Support prior to their license expiring.
If the provider is waiting on pending documentation — such as a current fire marshal report — it’s better to go ahead and submit the renewal application with the deficiency and upload a letter explaining why they don’t have the required documentation.
***If the application isn’t submitted before the license expires, the provider risks providing services without a license. This is only for licensed LTC providers. Does not include HCS/TxHmL providers as they are contracted, not licensed.
December 14th, 2023
ISS UPDATE WEBINAR DECEMBER of 2023
Please review webinar handout for changes to the Implementation Plan and Person-Directed Plan for ISS.
*PDP’s need to reflect type of ISS (In-Home, On-Site, Off-Site) and activities and schedule.
*IP’s need to also reflect type and objectives for type as well as hourly amount and dollar amount for each type of ISS.
August 18th, 2023
Transition to Individualized Skills and Socialization Survey Deadline Extended
HHSC implemented individualized skills and socialization services in the Home and Community-Based Services (HCS) and Texas Home Living (TxHmL) Medicaid 1915(c) waiver programs, effective Jan. 1, 2023.
HHSC is requesting feedback from HCS and TxHmL program providers only on the impact this change has had on individuals receiving services in the form of a short survey.
Take the survey to provide your feedback.
We thank you for your input. HHSC is extending the deadline to submit responses until Aug. 31, 2023.
All HCS and TxHmL program providers who have not submitted a response must complete the survey by this deadline. Providers who have already completed the survey do not need to submit an additional response.
July 17th, 2023
HHSC Updated the Individualized Skills and Socialization Hold Harmless Period through March 17th, 2024
On Jan. 1, 2023, HHSC implemented the DAHS Individualized Skills and Socialization program and offered an initial hold harmless period from Jan. 1, 2023, through June 30, 2023.
HHSC agreed to extend part of the hold harmless period related to the provision of off-site services.
HHSC will survey for compliance with off-site service delivery but will not move forward with enforcement action.
For all other regulatory requirements, beginning July 1, 2023, HHSC will survey for compliance and move forward with applicable enforcement actions as outlined in Title 26 Chapter 559, Subchapter H, Division 4.
The new hold harmless period related to the provision of off-site Individualized Skills and Socialization services begins July 1, 2023, and ends March 17, 2024.
March 28th, 2023
Host Home Companion Care Providers Concerning ISS & PHE Flexibilities For In-Home ISS
Clarification Concerning Information Letter No. 2023-10 (Replaces IL 2023-06) from February 2023
In-Home Individualized Skills and Socialization Information for Program Providers for COVID-19 PHE
In response to COVID-19 and to provide access to day habilitation services, the Health and Human Services Commission (HHSC) temporarily waived certain requirements in Sections 3710, 4381.3, 4381.7(6) and 4381.7(7) of the HCS Billing Requirements and the TxHmL Billing Requirements. Until the end of the COVID-19 PHE, this flexibility will continue as part of in-home individualized skills and socialization.
Effective May 12, 2023, these flexibilities will no longer be in effect:
The flexibility has allowed HCS and TxHmL program providers to provide in-home individualized skills and socialization to an individual in the individual’s residence, including those residing in their own homes or family homes, without having the required justification outlined below. Program providers and LIDDAs need to have transition plans ready for individuals who receive in-home individualized skills and socialization prior to this end date (before May 12th, 2023).
Beginning May 12th, 2023:
in order to receive in-home individualized skills and socialization, individuals must meet all requirements outlined in the HCS and TxHmL Program Rules, the HCS Billing Requirements, and the TxHmL Billing Requirements, which include:
• A physician has documented that the individual’s medical condition justifies the provision of in-home individualized skills and socialization; or
• A licensed professional or behavioral support service provider has documented that the individual’s behavioral issues justify the provision of in-home individualized skills and socialization; or
• The individual is 55 years of age or older and requests to receive in-home individualized skills and socialization.
In addition, after May 11, 2023, a service provider of host home/companion care will not be permitted to provide in-home individualized skills and socialization to the individual to whom they provide host home/companion care services.
Clarification & Answer to Question From Some of Our Readers:
This letter indicates that HHSC does not appear to prevent a host home provider from becoming an ISS provider, nor does it prevent that licensed ISS provider from providing on-site and/or off-site services to their own individuals living with them. In other words, it would appear they can be a HH/CC provider and licensed ISS provider at the same time and they can provide ISS services to their own individuals they are serving as HH/CC providers. They can not provide their own in-home ISS (anymore) as an HH/CC provider as of May 12th, 2023. The only ISS they can provide after May 11th, is if they are a licensed on-site and/or off-site provider.
March 1st, 2023
Reminder Must Be Licensed As ISS Provider To Bill As Of March 1st, 2023
![]()
For HCS/TxHmL Providers, you can’t bill for On-site &/or Off-site ISS as of today March 1st, 2023, if you send someone to an ISS location or have staff providing Off-site services (previously Community DH), if they are not listed as a licensed ISS program.
The directories may be accessed at: https://www.hhs.texas.gov/providers/long-term-care-providers/day-activity-health-services-dahs to find out if the ISS program is licensed.
**You can bill for In-Home ISS as persons providing In-Home ISS do not have to be licensed! No justification is needed for In-Home through May 11th, 2023 I believe. I believe HH/CC providers can still provide In-Home (This was part of the PHE exception prior to March 1st) up through May 11th, 2023, but I am still unclear and will inquire and update everyone when I get some kind of definitive answer.
Previous DH providers & New ISS Provider applicants: If you do not have a temporary ISS license by March 1, 2023, you may not provide or bill HCS, TxHmL, or DBMD providers for on- and off-site ISS services until the temporary license is received. HCS/TxHmL, DBMD Providers who have individuals attending an ISS program may not send persons to the program until they confirm that the operator of the program has received the license. There are no exceptions.
February 21st, 2023
More ISS Training
Very Important: Surveys of ISS Providers With Temporary Licenses
In case this information was overlooked by new ISS providers:
- Once HHSC issues a temporary license, HHSC may conduct a survey at any time.
- HHSC may conduct a survey of any licensed Individualized Skills and Socialization Providers prior to March 1, 2023.
- i.e. if HHSC issues a temporary license on Feb. 21, 2023, HHSC may conduct an initial survey on Feb. 27, 2023.
- HHSC conducts unannounced surveys of ISS Providers.
- For on-site ISS providers, the address on the license must match the address for service provision.
- ISS providers must allow HHSC surveyors access to the on-site location and off-site activity locations.
Please refer to Texas Administrative Code Title 26, Chapter 559 for more info on the LTCR survey process.
February 10th, 2023

How Do I Find A Licensed ISS Provider?
HHSC has now posted directories on the DAHS webpage to help people find a licensed ISS Provider.
The directories may be accessed at: https://www.hhs.texas.gov/providers/long-term-care-providers/day-activity-health-services-dahs
Please note the following:
- There are 2 directories: DAHS with ISS and DAHS-ISS Only.
- The DAHS with ISS Directory is intended to reflect entities licensed as just a DAHS, and entities licensed as DAHS with ISS.
- At this time, this particular directory lists all entities as just having a DAHS license. This is because the commission has yet to approve any DAHS with ISS licenses. The process for approving a DAHS with ISS application takes longer than that of a provider applying as an ISS-only entity. According to HHSC, the entity must undergo an LSC and Health survey before a license is issued to a DAHS with ISS entity. Once these have been approved, they will be listed in this directory as DAHS with ISS.
- Entities listed in the DAHS – ISS Only Directory, currently reflect a 6-month license. This is because these licenses are considered ‘temporary’ at this time. Once the health survey is conducted the entities will receive a one, two or three-year license.
February 5th, 2023
HHSC LTCR Updates the ISS FAQ’s
HHSC Long-term Care Regulation updated the Individualized Skills and Socialization frequently asked questions document on Feb. 01, 2023.
January 27th, 2023
FYI- somehow I missed this alert back in November for Licensed ISS providers. Please be sure to log in and set up your account.
PL 22-32 letter issued 11/28/22 to ISS providers that was sent out concerning Blackboard Connect Emergency System
The purpose of this letter was to inform providers of the emergency communication system called Blackboard Connect, how it will be used, and your responsibility in signing up for the system if you are an ISS provider. This system will be used to send emergency and outreach notifications through email, phone, voice and text if available.
The rules require program providers to assign a designee to enroll in and respond to requests through the system. The designee should be someone who is associated with the licensed building or someone who is responsible for communicating emergency communications. However, you may also have other designees, such as corporate headquarters staff, sign up.
Blackboard Connect sign-up process:
Go to this link and click “Sign Me Up!”
If you have any questions, please contact the Policy and Rules Section by email at LTCRPolicy@hhs.texas.gov or call (512) 438-3161.
Rember, this also applies to HCS, TxHmL and ICF providers among other services.
January 16th, 2023
- The ‘new’ IPC referenced in IL 2022-03 will most likely not be ready until March. They did not have answers as to what providers should do in the interim or even how service logs should be revised until new ones are available. (The letter does indicate that those individuals receiving DH at the time of the switch to ISS (March 1st, 2023) will initially roll over automatically to ISS ).
- After Feb. 28th this would apply to all current clients as far as IPC units are concerned. Persons who don’t have any Day Hab units/days on their plan as of Feb. 28th, 2023 and want ISS hours, will have to do a new PDP and request IPC hours. Providers will have a new IPC form, with ISS on it, before March 1st, 2023.
- To date, no provider has been issued an ISS license.
- Providers can confirm that an entity has an ISS license by checking the DAHS directory on the DAHS webpage: https://www.hhs.texas.gov/providers/long-term-care-providers/day-activity-health-services-dahs
ISS FAQs and Upcoming Webinars:
On January 26, 2023, from 9:00 to 10:30 HHSC will conduct its quarterly LTC webinar which will focus on ISS. To register for the webinar, go to: https://register.gotowebinar.com/register/5204373791714060639
January 12th, 2023
Information Letter No. 2023-03 Individualized Skills and Socialization Automatic Service Authorizations
Effective January 1, 2023, individualized skills and socialization became an available service in the HCS and TxHmL Programs. For the time period of January 1, 2023 to February 28, 2023 both day habilitation and individualized skills and socialization will be allowable program services.
Day habilitation will no longer be a Medicaid-billable service in the HCS or TxHmL Programs for dates of service beginning March 1, 2023, and ongoing.
On January 9, 2023, HHSC will automatically add units of individualized skills and socialization for all individuals with day habilitation (including individuals receiving in-home day habilitation through the COVID-19 flexibility) currently authorized on their individual plan of care (IPC). The units will be available for billing immediately for the provision of on-site, off-site, or in-home individualized skills and socialization and will be visible to program providers in the Medicaid Eligibility Service Authorization Verification (MESAV). The added units will be authorized beginning January 1, 2023 through the end of the individual’s current IPC period. For individuals with an IPC period that must be renewed between January 1, 2023 – April 30, 2023, the added units will be authorized until December 31, 2023.
These units for individualized skills and socialization will not be visible to program providers or service coordinators on the IPC in the Long-term Care Online Portal (LTCOP) on the Texas Medicaid & Healthcare Partnership (TMHP) website nor on the dashboard until a revision or renewal IPC is entered. This automatic service authorization will give service coordinators additional time to meet with the individual’s service planning team (SPT) to update the individual’s person-directed plan (PDP) and for program providers to update the individual’s implementation plan (IP) as this new service takes effect. HHSC is implementing this process to minimize disruption to an individual’s desired services.
Service Plan Revisions
At the individual’s next service planning team meeting to complete a revision or renewal IPC (whichever occurs first) for individuals receiving individualized skills and socialization, service coordinators should update the individual’s PDP to reflect the new individualized skills and socialization service. During the service planning team meeting, any new goals related to the provision of on-site and off-site individualized skills and socialization should be discussed and documented in the new action plan. Until the PDP is updated, the individual’s current day habilitation goals, frequency, and duration should be followed for the individualized skills and socialization service.
Following the update to the PDP, the IPC and IP must be updated in accordance with applicable HCS or TxHmL Program rules with the appropriate units of individualized skills and socialization. HHSC will update the IPC and IP form to add individualized skills and socialization by March 1, 2023.
All individual’s PDPs, IPCs, and IPs must be updated with the appropriate units of individualized skills and socialization in accordance with applicable HCS or TxHmL Program rules by December 31, 2023.
For new enrollees and current enrollees who are not currently receiving day habilitation, individualized skills and socialization will need to be added, once the IPC and IP form have been updated, to the individual’s service plan because units will not be auto-authorized for these individuals. Day habilitation can be added and delivered until February 28, 2023.
To read more, please click on link below, for Information Letter 2023-03 related to ISS automatic service authorizations and EVV
January 3rd, 2023
Easier Format For ISS Licensing Rules effective Jan. 1, 2023
The link below provides a format that is easier to read and understand the newly adopted licensing rules rather than those when published as adopted in the Texas Register
Effective Jan. 1, 2023, HHSC adopts new Individualized Skills and Socialization rules for providers who want to deliver individualized skills and socialization services. New rules provide guidance regarding:
- applying for an Individualized Skills and Socialization license;
- provider requirements; and
- HHSC survey and enforcement actions.
Read the new rules in Title 26 of the Texas Administrative Code, Chapter 559, Subchapter H.
HHSC also published Provider Letter 2023-01 New Regulatory Rules for Long-term Care Regulation (LTCR) Individualized Skills and Socialization Services. This PL provides guidance to Individualized Skills and Socialization providers about the new rules.
Read PL 2023-01.
December 23rd, 2022
NEW RULES FOR ISS & ISS LICENSE
HHSC Adds Individualized Skills and Socialization to Email and Text Updates
HHSC added an option to the HHSC email and text update GovDelivery system that subscribers can select to receive updates related to the Individualized Skills and Socialization services program. Users can select to receive Individualized Skills and Socialization program alerts from the “Provider Alerts” drop-down menu.
To sign up for updates, select this link Texas Health and Human Services Commission (govdelivery.com).
For questions about Individualized Skills and Socialization, please email LTCRPolicy@hhs.texas.
November 28th, 2022
Webinar for New Licensing Process Nov. 30th, 2022 Extended to 2 hrs
All providers interested in the new licensing process for the Day Activity Health Services Individualized Skills and Socialization program are invited to a 2-hour webinar on Nov. 30. Originally it was a 1 hr session but has now been extended to have enough time for questions and explanations.
HHSC Long-Term Regulation staff will discuss how to navigate TULIP, the licensing system, explain the license application process and provide an overview of the survey process. There will also be a Q&A session as time allows.
Register for the webinar: Licensing Process Webinar
November 19th, 2022
DAHS ISS Licensing Application Available!
On Dec. 1, 2022, HHSC will launch the Day Activity Health Services (DAHS) Individualized Skills and Socialization License Application in the Texas Unified Licensure Information Portal (TULIP).
Link to TULIP: https://txhhs.force.com/TULIP/s/
Email TULIP_Support@hhsc.state.tx.us with questions related to TULIP functionality or if you have issues gaining access.
Email LTC_NF_DAHS_Licensing@hhs.texas.gov with questions related to the DAHS Individualized Skills and Socialization licensing application
October 13th, 2022
Licensing Application Process For ISS:
October 2nd, 2022
Register for Individualized Skills and Socialization Provider Portal Trainings
Individualized Skills and Socialization Provider applicants are required to complete HHSC Individualized Skills and Socialization Provider Trainings. Below are two computer-based trainings, which will assist Individualized Skills and Socialization Providers with applying for a license and preparing for an inspection.
- Prelicensure Training for Individualized Skills and Socialization Providers
This training was designed for providers who wish to offer individualized skills and socialization services. Prior to surveys or inspection, an entity must submit an application for a Day Activity and Health Services license. Information about the requirements to obtain a license will be shared. Register for the training. - Preparing for an Inspection
This training was designed to assist Individualized Skills and Socialization Providers to prepare for an inspection. In this course, information about the inspection process and licensure rules will be shared. Register for the training.
September 24th, 2022
HHSC Moved The Individualized Skills and Socialization Webpage
The Individualized Skills and Socialization webpage moved from the Resources webpage to the main Long-term Care Providers webpage. This was done so its location is consistent with other Long-term Care Regulation programs and is easier to find.
Individualized Skills and Socialization can be found under the “Community-based Programs” heading.
August 23rd, 2022
No Public Hearing on ISS Licensing Rules
Comments must be submitted no later than 31 days after the date the rules were published in the Texas Register; i.e., 31 days after August 12, 2022.. Comments must be (1) postmarked or shipped before the last day of the comment period; (2) hand-delivered before 5:00 p.m. on the last working day of the comment period; or (3) emailed before midnight on the last day of the comment period. If the last day to submit comments falls on a holiday, comments must be postmarked, shipped, or emailed before midnight on the following business day to be accepted. When emailing comments, please indicate “Comments on Proposed Rule 22R050” in the subject line.
Public Hearing on ISS Program Rules
HHSC will conduct a public hearing on the proposed HCS, TxHmL and DBMD ISS program rules on September 7, 2022 from 8:00 am. until Noon. To register for the virtual hearing, go to: https://attendee.gotowebinar.com/register/927810115195515152
For a copy of the proposed ISS license rules or go to: https://www.hhs.texas.gov/regulations/policies-rules/health-human-services-rulemaking/comment-proposed-draft-rules
August 13th, 2022
Texas HHSC has developed the Individualized Skills and Socialization Provider Portal, an online source of information for providers of individualized skills and socialization.
The Individualized Skills and Socialization Provider Portal will allow providers to:
- Complete and review trainings on the Individualized Skills and Socialization service.
- Find and review provider letters and other information and releases related to Individualized Skills Socialization.
- Link to rules and other services related to Individualized Skills and Socialization.
Provider Communications
- PL 2021-42 – This Provider Letter offers a brief introduction to the new individualized skills and socialization service and what providers can expect as HHSC implements the service.
- Individualized Skills and Socialization Services webinar – This helpful webinar provides an introduction and overview to Individualized Skills and Socialization
- Individualized Skills and Socialization FAQs – revised April 26, 2022
- July 2022 – Individualized Skills and Socialization Provider Webinar – This webinar covers the service description, ratio requirements, and licensing information based on HHSC’s draft individualized skills and socialization rules.
August 6th, 2022
See Draft/Proposed Rules for ISS in HCS and TxHmL below:
Proposed ISS Rules (Main portion of rules start on page 13-52)
- The anticipated adoption date is October, 2022 with an effective date of November 2022. These dates also apply to the proposed rules for the DBMD waiver program.
- Very few changes were made from comments HHSC received during the informal comment period earlier this year. Though we had been apprised of such before this positing, know that any comments you submitted during the informal comment period will need to be resubmitted.
- Carefully review the introduction to the HCS and TxHmL rules on pages 1 -4, including the sections on Issues and Alternatives and Stakeholder Involvement on page 3.
- Carefully review the preamble to the rules before reading the actual rules and pay attention to the sections on Impact to Small Businesses.
- The proposed HCS and TxHmL rules are included in one document. To help you navigate the document, the following is offered:
Gofundme Fundraiser Link For Our Friend Marie “Lynn” Palmares
March 31st, 2025

Many of you may know our friend and colleague Marie “Lynn” Palmares. Lynn has worked in ICF and HCS programs in the Dallas/Ft. Worth area for many years. In the past 8 years or so she has been working with the YES waiver program. Lynn has helped many providers as an independent contractor and as a consultant for Twogether Consulting over the past 10 years with their HCS and YES waiver programs. In addition, Lynn has assisted our clients at Twogether Consulting with their HCS-Adult Mental Health and YES waiver applications.
Lynn has been very ill over the past year and was recently diagnosed with stomach cancer. She really needs some help with her bills for treatment and medications. Even with insurance, out-of-pocket expenses for treatments and medication are very high. The medication she needs the most now costs thousands per month. I have posted her daughter’s “gofundme” page she set up for Lynn, if anyone would like to help.
Previous Temporary Exception Now A Permanent Policy Change in HCS/TxHmL For Respite and CFC PAS/HAB
March 30th, 2025
Permanent Policy Change for CFC PAS/HAB- Letter 2025-04
HHSC has published Information Letter 2025-04 Permanent Change to HCS and TxHmL Policy for Community First Choice (CFC) personal assistance services (PAS)/habilitation (HAB) service providers. This letter informs financial management services agencies (FMSAs), local intellectual and developmental disability authorities (LIDDAs), and providers of Home and Community-based Services (HCS) and Texas Home Living (TxHmL) services that the temporary policy allowing the service providers of CFC PAS/HAB to live in the same home as the person receiving CFC PAS/HAB services is now permanent.
March 15th, 2025
Permanent Policy Change for CFC PAS/HAB
In March 2020, HHSC started a temporary policy change for respite and Community First Choice (CFC) Personal Assistance Services (PAS)/Habilitation (HAB) provided in the Home and Community-based Services (HCS) and Texas Home Living (TxHmL) waiver programs.
This change allowed service providers of respite and CFC PAS/HAB to live in the same home as the person receiving these services. A person’s spouse, or parent if the person is under 18, was not allowed to be a paid service provider of these services in accordance with the HCS, TxHmL and CFC Billing Requirements.
This temporary policy change that was extended and effective through March 31st, 2025, has now been made a permanent policy change, effective April 1st, 2025!
Program providers must complete the required background checks for all service providers, including respite and CFC PAS/HAB providers living in the same home as the individual receiving services. Requirements can be found in the following references:
- The Texas Administrative Code (TAC), Title 26, Part 1, Chapter 263, and Chapter 262.
- HCS and TxHmL Rules, 26 TAC §565.9(b) and §566.9(r) and (s).
- The HCS Program Billing Requirements and the TxHmL Program Billing Requirements, Section 3400 for service provider qualifications, and the CFC Billing Requirements for HCS and TxHmL Program Providers.
If you have any additional questions, please feel free to reach out to LTCR Policy at: LTCRPolicy@hhs.texas.gov.
Exception Ending August 31st, 2023
REMINDER: COVID-19 Update to Temporary Change to HCS and TxHmL Policy for Respite, CFC PAS/HAB Service Provider
In March 2020, HHSC implemented a temporary policy change for respite and Community First Choice Personal Assistance Services/Habilitation provided in the Home and Community-based Services and Texas Home Living waiver programs. This change allows service providers of respite and CFC PAS/HAB to live in the same home as the person receiving these services.
This change has given greater access to needed services for people living in their own home or family’s home. A person’s spouse or the person’s parent, if the person is under 18, is not allowed to be a paid service provider of these services in accordance with the HCS, TxHmL and CFC Billing Requirements.
This temporary policy change is effective March 27, 2020, through Aug. 31, 2023. HHSC will provide guidance if anything changes.
Program providers must complete the required background checks for all service providers. They must follow:
- The Texas Administrative Code, Title 26, Part 1, Chapter 263 and Chapter 262.
- HCS and TxHmL Rules, Section 9.177 (n) and (o), and Section 9.579 (r) and (s).
- The HCS Program Billing Requirements and the TxHmL Program Billing Requirements Section 3400 for service provider qualifications and the CFC Billing Requirements for HCS and TxHmL Program Providers.
Where To Find Medicaid Eligibility Information for LTC Providers: TexMedConnect
March 25th, 2025
Video About Medicaid Eligibility Reports on the LTCOP Dashboard Now Available on YouTube
An educational video focused on Medicaid eligibility reports on the Long-Term Care Online Portal (LTCOP) Dashboard has been added to the Texas Medicaid & Healthcare Partnership’s HCS and TxHmL YouTube Playlist. Read the full alert.
November 14th, 2024
Eligibility Information Available for Long-Term Care Providers and LIDDAs
LTC providers and LIDDAs that are seeking eligibility information can pull Medicaid Eligibility and Service Authorization Verification (MESAV) using any of the following field combinations through TexMedConnect.
This service can be accessed 24 hours a day, 7 days a week
. • Medicaid/Client No. and Last Name
• Medicaid/Client No. and Date of Birth
• Medicaid/Client No. and Social Security Number
• Social Security Number and Last Name
• Social Security Number and Date of Birth (DOB)
• Last Name, First Name, and DOB
MESAV can provide the Medicaid eligibility Program Type, Coverage Code, and Medicaid Recertification Due Date to help providers ensure appropriate and continued Medicaid eligibility for long-term care services.
Overview Presentation of Specialized Telecommunications Assistance Program (STAP) For Deaf and Hard of Hearing
March 14th, 2025
![]()
Deaf and Hard of Hearing Services From HHSC Presents
Overview of the Specialized Telecommunications Assistance Program (STAP)
Wednesday, March 26, 2025
11:00 a.m. – 12:30 p.m., CST
Join Aaron Mowell, STAP manager, for an overview of the Specialized Telecommunications Assistance Program (STAP). The purpose of STAP is to allow people with disabilities to access the telephone network, enabling them to call family and friends, make doctor’s appointments, and reach emergency services. This informative session will explain the program requirements and application process and provide an opportunity for you to ask questions.
This webinar will be presented in American Sign Language (ASL) and spoken English; CART (captioning) and ASL/English interpretation will be provided.
Certificates of Attendance will be awarded to attendees that may be used for continuing education documentation. In addition, participants may earn 0.15 DHHS General CEUs (accepted by BEI).
Click on link below to register and for more information:
Registration Link & Details
HCS/TxHmL Providers & FMSAs: Technical Assistance Session For TMHP on April 2025
March 15th, 2025
Medicaid and CHIP Services (MCS) will be hosting monthly sessions for Program Providers and Financial Management Services Agencies (FMSAs), who use the Long-term Care (LTC) online portal for the Home and Community-based Services (HCS) and Texas Home Living (TxHmL) waiver programs.
- TMHP and HHSC staff will be available to troubleshoot and potentially resolve issues with forms and claim submissions in the LTC online portal.
- All attendees should be prepared to discuss and show, if needed, the issues they encounter when attempting to submit forms or claims in the LTC online portal.
Save the Date
The technical assistance session will be held on:
- Thursday, April 24, from 10am-11:30am
EVV (Electronic Visit Verification) Updates
March 12th,
The EVV Policy Handbook Revision
The Electronic Visit Verification Policy Handbook (EVV) has been revised. This revision is effective March 12, 2025.
The Electronic Visit Verification Policy Handbook as well as Revision Log has been revised.
These revisions are outlined in the new revision log (PDF) located on the EVV webpage. The Revision Log outlines the specific changes and allows users to identify which policies have been updated in each section of the EVV Policy Handbook.
The handbook’s policies include EVV standards and policy requirements for:
- Program providers
- Proprietary System Operators
- Financial Management Services Agencies
- Consumer Directed Services employers
- Payers, such as HHSC and managed care organizations
Review the revisions here and Email HHSC EVV Operations with questions.
March 08, 2025
EVV System Daylight Savings Time Change
On March 9, the state provided EVV system, HHAeXchange, and EVV proprietary systems, will automatically adjust for Daylight Savings Time.
This means that the actual hours worked and billable time for EVV Visits recorded during the time change will decrease by one hour in the EVV systems.
For manual visits, the actual time should be recorded in the EVV system based on when the service provider started and ended delivery of services.
The EVV system will automatically account for the daylight savings time change.
No action is required from program providers, financial management services agencies, or CDS Employers.
Reminder: Register for HHAeXchange EVV System Training for CDS Employers
HHAeXchange is hosting an EVV system training webinar on Wednesday, Feb. 12, from 11 a.m. – 12 p.m. Central time for Consumer Directed Services (CDS) employers who use HHAeXchange as their EVV system.
Attending the webinar will complete the annual EVV system training requirement for CDS employers.
Agenda
- HHAeXchange System Login
- Managing the HHAeXchange Services Portal
- Walkthrough of the EVV Clock in and Clock Out Methods
- Support Resources
- Q&A Session
Email HHAeXchange with any questions.
January 19th, 2025
EVV Visit Maintenance Unlock Request Updates
Texas HHSC has updated the Electronic Visit Verification (EVV) Visit Maintenance Unlock Request (VMUR) templates, VMUR job aids, and VMUR policy on the EVV webpage.
Policy
HHSC has posted an advanced notice of the revised 9060 VMUR policy that will be added to the EVV Policy Handbook in an upcoming handbook revision. These revisions are outlined in the 9060 Visit Maintenance Unlock Request (PDF) and became effective Nov. 12, 2024. The revisions are also available on the EVV webpage.
Revisions include:
- Standardizing the timeframes for processing a VMUR.
- Clarifying the roles of program providers, financial management services agencies (FMSAs), consumer directed services (CDS) employers, proprietary system operators (PSOs), payers, state provided EVV system vendors, and EVV proprietary system vendors.
Updates to VMUR Templates and VMUR Job Aids
HHSC published EVV VMUR templates for Program Providers and FMSAs (Excel) and for CDS employers (Excel) on the EVV webpage.
These updates include:
- A new option to select a Former EVV System from the drop-down list when submitting a VMUR for legacy visits.
- Adding all approved PSOs in the Current EVV System and Former EVV System drop-down list.
- Removal of the Service Area column.
- Revised instructions tab to reflect these changes.
The VMUR job aids contains information on the VMUR process, including examples of the most common VMURs. The EVV VMUR Job Aid for Program Providers and FMSAs (PDF) and EVV VMUR Job Aid for CDS Employers (PDF) are available on the EVV webpage.
Email questions to your payer, EVV or your managed care organization.
January 14th, 2025
Correction to the EVV PSO Operation Readiness Review Sessions Updates
HHSC published a notice on Dec. 4 about the EVV Proprietary System Operator (PSO) Onboarding Process Overview and Timeline to the TMHP EVV Proprietary Systems webpage.
The correction includes the revised document titles and publications of the EVV PSO Onboarding Paths:
- EVV PSO Onboarding Overview and Timeline Standard Path Process (PDF).
- EVV PSO Onboarding Overview and Timeline Expedited Path Process (PDF).
Standard Path Demonstration note:
Proprietary system vendors onboarding with a program provider or financial management services agencies (FMSA) in a Standard Path onboarding session are strongly encouraged to consider all EVV system functionality that onboarding program providers or FMSAs and future program providers or FMSAs may require to support their EVV-required service delivery when preparing for demonstrations during the Standard Path ORR.
A program provider or FMSA wishing to onboard with a previously approved proprietary system who isn’t approved for EVV functionality that the program provider or FMSA requires, must complete a modified Standard Path ORR with the previously approved proprietary system vendor to get approval to use the new functionality.
Email TMHP EVV PSO with any questions.
December 5th, 2024
Reminder – Compliance Review Grace Period Ends Dec. 31, 2024
The compliance reviews grace period for EVV Usage and EVV Landline Phone Verification reviews for, personal care services and home health care services, will end on Dec. 31, 2024. Beginning Jan. 1, 2025, program providers, financial management service agencies (FMSAs) and Consumer Directed Services (CDS) employers, that do not fully comply with the EVV usage and landline review requirements will be subject to enforcement actions.
October 30th, 2024
Don’t Forget Your Annual EVV Training Requirement!
HHSC has stated the following: Program providers, FMSAs, CDS employers, or any staff who performs EVV system operations (such as visit maintenance) must complete required EVV training initially before using the EVV system, and then annually after that.
Note: Service providers and CDS employees are not required to take clock in and clock out methods training annually after they’re trained initially. However, if a service provider or CDS employee switches the clock in and clock out method they’re using, they may need some refresher training on how to use another method. In addition, if a program provider or FMSA transfers from one EVV system to another, then the program provider is required to train the service provider on the new EVV system’s clock in and clock out method(s), and the CDS employer is required to provide training to the CDS employee on the new EVV system’s clock in and clock out method(s). We will clarify that in the Training Checklist the next time we update it.
The EVV Training Policy is located in the EVV Policy Handbook in sections 4200–4250.
October 2nd, 2024
Compliance Review Grace Period Ends Dec. 31st, 2024!
The compliance reviews grace period for EVV Usage and EVV Landline Phone Verification reviews for, personal care services and home health care services, will end on Dec. 31, 2024.
Beginning January 1, 2025, program providers, financial management service agencies (FMSAs) and Consumer Directed Services (CDS) employers, that do not fully comply with the EVV usage and landline review requirements will be subject to enforcement actions.
Payers conduct EVV compliance reviews to make sure program providers, FMSAs and CDS employers are in compliance with EVV requirements and policies.
Payers will conduct reviews and initiate contract or enforcement action if the program providers, FMSAs or CDS employers do not meet any of the following EVV compliance requirements:
- Usage Reviews
- Meet and maintain the minimum EVV Usage Score of 80%.
- Ensure staff is properly trained and consistently using EVV to record visits.
- Landline Reviews
- Payers will review landline reports generated from the EVV systems to determine compliance with the EVV Landline requirements.
- Program providers and FMSAs must ensure the phone number entered in the EVV system is a valid landline for members and CDS employers who have chosen to use a landline for clocking in and clocking out.
Next Steps
Program Providers, FMSAs, and CDS employers are encouraged to review their EVV Usage Reports monthly to ensure compliance with EVV requirements.
- Program providers and FMSAs can generate EVV Usage reports from the TMHP EVV Portal.
- Option 1 and Option 2 CDS employers can generate EVV Usage reports directly from their EVV system.
- Option 3 CDS employers must request a copy of their EVV Usage report from their FMSA.
Resources
Review section 11000 of the EVV Policy Handbook for more information about EVV Compliance Reviews.
Contact HHSC EVV Operations for questions.
September 12th, 2024
How to bill for HHCS delivered in-home versus out-of-home.
Refer to the EVV Home Health Care Services Bill Codes Table (PDF) on the HHSC EVV webpage to ensure you’re using the appropriate Healthcare Common Procedure Coding System (HCPCS) and Modifiers before submitting the EVV claim.
Billing Combinations for HHCS
HHSC created new Long-Term Care billing combinations to submit claims for EVV and non-EVV service delivery locations.
- HCS and TxHmL Own Home/Family Home (OHFH) should be billed as outlined in the EVV HHCS Service Bill Codes Table – version 2.1 (Excel).
- Out-of-home should use the existing billing combinations with the KX modifier found in the HCS and TxHmL Bill Code Crosswalk (Excel).
- Other Residential Types should use the existing billing combinations with the HQ modifier found in the HCS and TxHmL Bill Code Crosswalk (Excel).
**Services that begin or end in a member’s OHFH setting will require an EVV visit match.
**Services provided out-of-home in the Community or in Other Residential Type settings will not require an EVV visit match.
HHSC has published training resources for program providers and FMSAs to prevent EVV claim mismatches when submitting EVV claims for HCS and TxHmL services:
- Best Practices to Avoid Claim Mismatches for HCS and TxHmL (PDF)
- HCS and TxHmL Best Practices to Avoid EVV Claim Mismatches (Video)
June 19th, 2024
FYI- there are also additional modifiers for EVV-required services (such as TG for Specialized Nursing and UC for CDS Nursing).
Useful EVV tool:
June 7th, 2024
Reminder:
Please Use Appropriate Modifiers To Be Reimbursed Properly For Nursing & Other Specific Therapies That Occur In (OFH) In-Home Services!
Updates LTC HCS and TxHmL Bill Code Crosswalks for EVV Home Health Care Services
Please Note The In-Home Billable Activities for Nursing & Specific Therapies in Own Family Home (OFH) EVV Crosswalk Changes
Electronic Visit Verification (EVV) claims matching for home health care services (HHCS) began Jan. 1, 2024.
EVV claims with dates of service of Jan. 1, 2024, and after that do not have an EVV visit match will be denied.
HHSC created new Long-Term Care billing combinations to submit claims for EVV and non-EVV service delivery locations.
- Existing HHCS billing combinations have new descriptions for EVV services in the member’s own home/family home (OHFH).
- New out-of-home services use the existing billing combinations with the KX modifier.
- New in-home or other residential-type settings use the existing billing combinations with the HQ modifier.
Services that begin or end in a member’s OHFH setting will require an EVV visit match. Services provided out-of-home in the community or in other residential-type settings will not require an EVV visit match.
Home and Community-based Services (HCS) and Texas Home Living (TxHmL) EVV claims require the Texas EVV Attendant ID for in-home EVV services. Reference the document, HCS and TxHmL Best Practices to Avoid EVV Claim Mismatches (PDF) for information related to the Texas EVV Attendant ID.
Agency Services Affected
• Nursing Services provided in the member’s own home/family home (RN; LVN; Specialized RN; Specialized LVN)
• Occupational Therapy provided in the home
• Physical Therapy provided in the home
“Own home/family home” does not include Host Home/Companion Care or Supervised Living/Residential Support Services (3/4-bed home).
CDS (Only Nursing Affected)
Crosswalk changes
Place of Service: 12 (the group home or host home)
HCPCS:
~ T1002 (RN)
~ T1003 (LVN)
Modifier: HQ
Place of Service: 11, ,49, 99, etc. (applies to ALL persons regardless of their place of residence)
HCPCS:
~ T1002 (RN)
~ T1003 (LVN)
Modifier: KX
Place of Service: 12 (OHFH). REQUIRES EVV
HCPCS:
~ T1002 (RN)
~ T1003 (LVN)
Modifier: no modifier
Resources:
- See the new billing combinations in the Long-term Care Bill Code Crosswalks.
- For more information about EVV, visit the HHS EVV webpage.
- For news and updates, visit the Texas Medicaid and Healthcare Partnership website.
- Review FAQs about the EVV HHCS Implementation (PDF), located on the EVV 21st Century Cures Act webpage.
- People who deliver EVV-required services must be registered for EVV GovDelivery to receive EVV updates by email.
For questions about the EVV HHCS bill codes, modifiers or HHCS required to use EVV (PDF), email HHSC EVV Operations.
May 25th, 2024
EVV Proprietary Systems
An Electronic Visit Verification (EVV) proprietary system is an HHSC-approved system that a program provider or financial management services agency (FMSA) may decide to use instead of the state-provided EVV vendor system and:
- Is purchased or developed by a program provider or an FMSA.
- Is used to exchange EVV data with the EVV Aggregator.
- Complies with HHSC EVV Policy as it relates to EVV proprietary systems.
- Complies with HHSC EVV Business Rules for proprietary systems.
- Complies with the requirements of Texas Government Code Section 531.024172 or its successors.
An EVV Proprietary System Operator (PSO) is a program provider or FMSA that is approved to operate an EVV proprietary system.
Refer to the EVV Policy Handbook, including Section 5000, for more information.
EVV PSO Onboarding Process
Step 1: Submit a Request Form
Program providers and FMSAs must complete, sign, and submit the EVV Proprietary System Request Form located in the EVV Portal to start the PSO onboarding process.
Note: EVV Portal access is required to submit a request form. Refer to the Accessing the EVV Portal for Program Providers and FMSAs job aid for more information. Request forms that are emailed to HHSC or TMHP will not be accepted.
When the request form is successfully submitted, program providers and FMSAs will receive a confirmation number (Request Form ID) and a confirmation date and time (Request Form Submission Date and Time).
Note: The submission of a request form does not guarantee an assignment to a PSO Operational Readiness Review (ORR) session. TMHP will review the submitted request forms and PSO ORR session requirements and notify program providers and FMSAs of their assignment status.
EVV ORR Sessions
The following PSO Onboarding Process Overview and Timeline documents outline the steps and required timeframes for a program provider or FMSA to onboard their proprietary system in the Texas EVV operating environment managed by HHSC and TMHP.
PSO Onboarding Standard Process Overview and Timeline
PSO Onboarding Expedited Process Overview and Timeline
Here is the high-level schedule for the 2024 PSO Onboarding:
| Session | Planning Meeting Date | ORR Start Date | Session Approval Date |
|---|---|---|---|
| 2024-1: Expedited | Feb. 5, 2024 | Feb. 19, 2024 | Mar. 8, 2024 |
| 2024-2: Expedited | Apr. 29, 2024 | May 6, 2024 | Jun. 3, 2024 |
| 2024-3: Standard | May 20, 2024 | Jun. 3, 2024 | Jul. 18, 2024 |
| 2024-4: Expedited | Aug. 12, 2024 | Aug. 19, 2024 | Sept. 24, 2024 |
| 2024-5: Standard | Sept. 2, 2024 | Sept. 16, 2024 | Oct. 30, 2024 |
Note: Please note that TMHP has a limited number of slots based on the available capacity and the schedule is subject to change.
A program provider or FMSA must have a developed and compliant proprietary system that meets all HHSC requirements by the ORR begin date.
Visit the PSO Business Rules to learn more about the compliance standards for proprietary systems in the Texas Medicaid EVV Program.
TMHP Contacts
800-626-4117
(Option 4)
TMHP Contact Center:
May 2nd, 2024
January 7th, 2024
Clarification Landline Vs. Mobile
EVV Program providers and financial management services agencies (FMSAs) must enter and maintain correct information in the EVV system for their service providers or Consumer Directed Services (CDS) employees.
Program providers and FMSAs must not enter an unallowable landline phone type into the EVV system as the member’s home phone landline.
An unallowable landline phone type is a cellular phone or cellular-enabled device, such as a tablet or a smart watch. A phone used to clock in or clock out through the landline method must be a landline phone, and not a cellular phone or device. Cellular phones, tablets, smart watches, and laptops come under “mobile devices” and should be entered as such..
TMHP Published EVV Known Issues and Resolutions, Vol. 2
Texas Medicaid & Healthcare Partnership (TMHP) published a table that highlights the most frequently occurring issues Electronic Visit Verification (EVV) users have experienced with the HHAeXchange system. The table also features a resolution for the issues that were identified.
For more information, refer to EVV Known Issues and Resolutions, Volume 2, on TMHP’s EVV webpage.
Resources
January 1st, 2024
HHSC has revised the Electronic Visit Verification (EVV) rules in Texas Administrative Code (TAC), Title 1, Chapter 354, Subchapter O. The new TAC rules are effective Jan. 1, 2024.
The new EVV TAC rules:
- Add the home health care services required by the 21st Century Cures Act, 1903(l) of the Social Security Act (42 U.S.C. §1396b(l)).
- Add the current policies regarding training, visit maintenance, and requests by program providers and FMSAs to become Proprietary System Operators (PSOs).
- Add definitions related to the addition of the new TAC rules.
- Reorganize the structure of the existing EVV-required personal care services list for clarity.
December 31st, 2023
HHSC Electronic Visit Verification (EVV) is reaching out to you with time-sensitive information. Also noted in the TMHP news webpage:
- Program Providers and FMSAs Should Have Download Visit Data by Dec. 22, 2023.
- EVV Known Issues and Resolutions, Vol. 2.
- HHSC will require EVV for Medicaid Home Health Care Services (HHCS) beginning Jan. 1, 2024.
- Effective January 1, 2024, and after, when an HHCS EVV claim is submitted without a matching EVV visit transaction, the EVV claim will be denied.
- A list of HHCS services that fall under this requirement is found in the 21st Century Cures Act webpage.
December 6th, 2023
Discontinuation of EVV Free Text Reviews
Effective Aug. 1, 2023, the Texas Health and Human Services Commission (HHSC) and managed care organizations (MCO) will no longer conduct EVV compliance reviews for required free text.
HHSC no longer requires the documentation of any missing clock in and clock out in the free text field for dates of service on and after Aug. 1. The EVV system now requires missing time not electronically captured to be entered in the Bill Time In and Bill Time Out fields.
New reason codes effective Oct. 1, 2023 (PDF), require program providers, financial management services agencies (FMSAs) and Consumer Directed Services (CDS) employers to enter free text only when using the following two reason codes:
- Reason Code 210I — Emergency
- Reason Code 600 — Other
Email questions to HHSC EVV Operations.
November 11th, 2023
Prepare for EVV Cures Act Home Health Care Services Implementation
HHSC will require Electronic Visit Verification (EVV) for Medicaid home health care services (HHCS) beginning Jan. 1, 2024, as listed in the Home Health Care Services required to use EVV (PDF). The 21st Century Cures Act is the federal law that requires states to implement EVV.
HHCS Claims for EVV Required Services Must be Submitted to TMHP Starting Dec. 1
- Program providers and financial management services agencies (FMSAs) must submit all HHCS EVV claims to Texas Medicaid & Healthcare Partnership (TMHP) using TexMedConnect, or through Electronic Data Interchange (EDI) using a Compass 21 (C21) Submitter ID starting with dates of service on or after Dec. 1, 2023.
- Managed care organizations (MCOs) will reject any HHCS managed care claims with EVV services and dates of service on or after Dec. 1, 2023, back to the program provider and FMSA, directing them to submit the claim to TMHP for EVV claims matching.
Register for TexMedConnect
- To access TexMedConnect through the TMHP website you must already have an account. If you don’t have an account, set one up using the information provided in the TMHP Website Security Provider Training Manual.
- Program providers and FMSAs that need help setting up C21 or CMS Submitter IDs should contact the EDI Help Desk at 888-863-3638, Option 4, or visit the TexMedConnect webpage for additional information.
Request EVV Portal Access
- To access the EVV Portal, program providers and FMSAs must have a TMHP User Account.
- Program providers and FMSA staff must contact their TMHP Provider Administrator to request EVV Portal access.
- For full instructions, review the EVV Portal job aids on the EVV Learning Management System (LMS).
Complete Onboarding and EVV Portal Training by Dec. 31
Program providers and FMSAs must complete the following before Dec. 31, to avoid impacts to EVV claims payment:
- Onboard with the state-funded EVV vendor system, HHAeXchange by submitting the HHAeXchange Provider Onboarding Form.
- Complete the TMHP Learning Management System (LMS) to complete annual EVV Portal training requirements.
Visit the TMHP EVV Training webpage for more information.
EVV Home Health Care Services Practice Period: Oct. 1 – Dec. 31
The practice period allows program providers and FMSAs, to practice using the EVV system, using the EVV Portal and submitting EVV claims before the Jan. 1, 2024, implementation date. EVV claims will be paid by the payers (HHSC or MCO) even if the EVV visit transactions do not match the EVV claims.
- Consumer Directed Services (CDS) employers can practice using the EVV system selected by their FMSA.
- Service providers and CDS employees can practice clocking in and clocking out using their program provider’s or FMSA’s selected EVV system, and the visit data will be transmitted to the EVV Aggregator.
EVV Claims Matching with Denials
Effective Jan. 1, 2024, and after, when an HHCS EVV claim is submitted without a matching EVV visit transaction, the EVV claim will be denied. This applies to all program providers and FMSAs required to use an EVV system. Program providers and FMSAs will be able to view EVV claim match results in the EVV Portal.
Resources:
- For questions about HHAeXchange onboarding, technical help with using the HHAeXchange Portal or issues related to data, contact HHAeXchange:
Email: TXsupport@hhaexchange.com
Phone: 833-430-1307 - Review FAQs about the EVV HHCS Implementation (PDF), found on the EVV 21st Century Cures Act webpage.
- For specific HHCS billing codes combinations, that require the use of EVV, refer to the EVV HHCS Service Bill Codes table in Excel or PDF formats.
- For more information about EVV, visit the HHS EVV webpage.
October 16th, 2023
IMPORTANT NOTICE: EVV Data Access & Conversion
For program providers transitioning to the new state-funded EVV vendor, HHAeXchange:
All visits in the EVV Aggregator will continue to be available and accessible for program providers. One year of historically accepted visits will be available in HHAeXchange as part of data conversion. This will be based on the data available in the EVV Aggregator.
For visit dates within the 95-day visit maintenance window, program providers should refer to the EVV Portal and perform visit maintenance in their legacy vendor system.
*If you rely on specific fields from EVV systems, DataLogic/Vesta and FirstData/AuthentiCare, this data may not be available after they are migrated to HHAeXchange.
Data Conversion
The following data will be transferred from your current EVV systems (AuthentiCare or Vesta) and uploaded to the new HHAeXchange system:
- Five years of profile data
- Direct service provider information
- Member information
- CDS employer information
- Service authorization information
- One year of accepted visit information (from the EVV Aggregator)
Data Availability
EVV visit data for dates of service Sept. 1, 2019, to present is available in the EVV Portal. Program providers or FMSAs needing access to data prior to Sept. 1, 2019, can email HHSC EVV Operations.
Program providers and FMSAs are encouraged to download and archive data in your current EVV systems that is not being converted as outlined above. For program providers and FMSAs that use the EVV systems or the paid for versions of AuthentiCare or Vesta to store or maintain non-EVV visit data, you should take steps now to maintain your non-EVV visit data. Access to the state provided AuthentiCare and Vesta systems will end on Dec. 22, 2023.
Once the data has been reviewed, users should contact HHAeXchange for any issues or concerns with their data.
Email HHAeXchange or call 833-430-1307.
August 20th, 2023
EVV Alternative Device Policy For New State EVV Vendor
HHSC has updated the alternative device policy notice posted on July 17.
In addition to allocating free alternative devices to 7.5% of the program providers or Financial Management Services Agencies (FMSAs) census (rounded to the nearest whole number), HHSC is allowing the purchase of additional alternative devices for qualifying members.
This policy applies to program providers and FMSAs who will use the new State EVV vendor, HHAeXchange.
Additional information will be forthcoming about the processes for providers and FMSAs to order alternative devices.
August 19th, 2023
Hurry Before It’s Too Late! EVV Onboard with HHAeXchange by Aug. 31
Begin the onboarding process with the new Electronic Visit Verification (EVV) vendor HHAeXchange.
Current Users
Program providers and financial management services agencies (FMSAs) who are transitioning to HHAeXchange, and are not in the proprietary system onboarding process, must submit the HHAeXchange Provider Onboarding Form by Aug. 31.
Application programming interfaces (APIs) can be used to exchange data between third-party software systems, such as payroll systems, electronic health records systems, and the HHAeXchange Portal (the new EVV vendor system).
Program provider and financial management services agencies, who want to integrate their third-party software systems with HHAeXchange, can refer to the specifications listed in the HHAeXchange Web Service API Guide (PDF).
APIs available to integrate with HHAeXchange include:
- Service Provider (Create, Update, Search, Get)
- Member (Create, Update, Search, Get)
- Schedule (Create, Update, Search, Get)
- Visit (Search, Get)
- Authorization (Create, Update)
To begin the integration process, submit a ticket through the HHAeXchange Client Support Portal.
Contact HHAeXchange for provider onboarding form questions.
June 13, 2023
Next Steps and Timeline for Transition to New Electronic Visit Verification State Vendor System
HHSC has posted the next steps and timeline to transition to the new, single and state-funded Electronic Visit Verification vendor system, the HHAeXchange Portal.
As stated in the EVV notice posted on May 5, users of the current EVV vendor systems (DataLogic/Vesta or First Data/AuthentiCare) must transition to HHAeXchange or receive approval as an EVV Proprietary System Operator by Oct. 1, 2023.
The following topics are listed in the notice, “Next Steps and Timeline for Transition to HHAeXchange” (PDF):
- EVV requirement
- Transition to HHAeXchange by Oct. 1, 2023
- Proprietary systems
- HHAeXchange Information Sessions
- HHAeXchange Provider Onboarding Form
- EVV Policy updates
- HHAeXchange System Training
- Access to the HHAeXchange Portal
- Contact information and other resources
*Training begins in August and access to the portal begins in September of 2023 for HHAeXchange.
HHSC has created a brief version of the notice that was posted on May 5 about the transition and changes related to the new, single and state-funded Electronic Visit Verification vendor system, HHAeXchange.
Program providers and financial management services agencies may provide the brief notice to their members, services providers and Consumer Directed Services employers. The brief notice is available in English (PDF) and Spanish (PDF).
HHSC will continue to post communications and resources throughout the transition.
June 10th, 2023
Registration Available for HHSC EVV Policy Training Webinars for Program Providers, FMSAs and CDS Employers
HHSC is hosting Electronic Visit Verification policy training webinars for program providers, financial management services agencies and Consumer Directed Services employers to complete the EVV policy training requirement. EVV policy training provides training on the EVV Policy Handbook.
Webinar agendas are included in the registration links below.
Webinar Registration
- Annual EVV Policy Training Webinars: For program providers, FMSAs and CDS employers using EVV for personal care services (PDF).
- Initial EVV Policy Training Webinars: For program providers, FMSAs and CDS employers new to EVV due to the EVV Cures Act Home Health Care Services implementation (PDF).
Program providers, FMSAs and CDS employers can also complete the EVV policy training requirement on the HHS Learning Portal.
The EVV Required Training Checklists (PDF) will help track completed EVV trainings.
Register for EVV GovDelivery to receive EVV notices by email, such as training updates and future webinar registrations.
June 2nd, 2023
EVV Resources Updates
HHSC has updated three Electronic Visit Verification resources that are located on the EVV webpage:
- EVV Training Requirements Checklists
- Getting Started with EVV
- Program and Service Requirements for Schedules
EVV Training Requirements Checklists
The EVV Required Training Checklists (PDF) is a resource for those required to use EVV due to all previous and upcoming EVV implementations (personal care services and home health care services). This resource was updated with the following:
- Aligns with EVV Policy Handbook revisions
- Lists training course names
- Describes required trainings
- Defines EVV Portal users, EVV system users and billing staff
- Includes link to sign up for GovDelivery
- Has interactive (fillable form) features to help document completed trainings
Getting Started with EVV
Getting Started with EVV is a guide that lists steps and resources to start using EVV. HHSC has created a single-page guide for each of the following stakeholders:
- Program providers (PDF)
- Financial management services agencies (PDF)
- Consumer Directed Services employers (PDF)
- Service providers (PDF)
- Consumer Directed Services employees (PDF)
Program and Service Requirements for Schedules
The document, Program and Service Requirements for Schedules (PDF), is a resource that describes requirements related to using schedules in the EVV system. HHSC added managed care organization programs to the document.
Email EVV Operations for questions.
May 13th, 2023
Reminder: EVV Claims Matching for HCS and TxHmL Will Begin for Dates of Service Starting May 1, 2023
This is a reminder that Electronic Visit Verification claims matching for Home and Community-based Services and Texas Home Living will begin on May 1, 2023. EVV claims with dates of service of May 1, 2023, and after that do not have an EVV visit match will deny.
For more information about billing updates for HCS and TxHmL, including resources to help avoid future payment denials or recoupments, reference the notice located on the EVV web page, “EVV Claims Matching for HCS and TxHmL Will Begin for Dates of Service Starting May 1, 2023”.
Email EVV Operations for questions.
April 3rd, 2023
Session 4 ORR Schedules Added to TMHP EVV Proprietary Systems Web Page
HHSC created the Session 4 Operational Readiness Review, which is a special abbreviated Electronic Visit Verification Proprietary System Operator onboarding path that supports additional PSO ORRs. This additional path allows program providers and financial management services agencies to onboard with a previously approved proprietary system or a proprietary system that is participating in the Session 3 Standard Path ORR.
The Texas Medicaid and Healthcare Partnership has updated the EVV ORR section of the EVV Proprietary Systems web page to include ORR schedules, requirements and information about the Session 4 ORR.
Email the TMHP EVV PSO inbox for questions.
January 12th, 2023
Electronic Visit Verification (EVV) for Individualized Skills and Socialization (ISS) IL-2023-03 alert letter
Electronic Visit Verification (EVV) for Individualized Skills and Socialization
Program providers must ensure EVV is used when delivering in-home individualized skills and socialization in an own home/family home (OHFH) setting. For dates of services on and after March 1, 2023,
HHSC will deny or recoup a claim for in-home individualized skills and socialization in the own home/family home setting without a matching EVV visit record. For more information about EVV claims matching, refer to the EVV notice, “EVV Claims Matching for HCS and TxHmL Starts March 1, 2023”.
Program providers must input the Texas EVV Attendant ID for in-home EVV individualized skills and socialization OHFH claims.
Email TMHP EVV Operations for questions or refer to the document, HCS and TxHmL Best Practices to Avoid EVV Claim Mismatches (PDF), for more information to help avoid EVV claim mismatches.
to the LTC Billing Crosswalk for more information about Staff ID requirements.
By January 13, 2023, HHSC will update the EVV Personal Care Services Bill Codes Table, located on the HHSC EVV web page, to include the specific Individualized Skills and Socialization billing codes which require EVV. Sign up for EVV GovDelivery to receive updates by email.
For EVV-related contact information, reference the EVV Contact Information Guide for Program Providers and FMSAs (PDF).
To read more, please click on link below, for Information Letter 2023-03 related to ISS automatic service authorizations and EVV
January 2nd, 2023
EVV Vendor Systems Will Display Individualized Skills and Socialization Services Starting 1/1/2023 Before New Authorizations Are Available
This notice is for Home and Community-based Services program providers, Texas Home Living program providers and financial management services agencies required to use Electronic Visit Verification.
As shared in the EVV notice published on Oct. 26, Individualized Skills and Socialization bill codes will replace day habilitation bill codes; therefore, the EVV vendor systems will display 1/1/23 as the effective date for these new services; however, HHSC has extended the date when the new authorizations for Individualized Skills and Socialization services will be available, which is the week of 1/9/23.
Program providers and FMSAs required to use EVV must continue to use EVV.
HHSC will continue posting related updates.
As a reminder, EVV claims matching for HCS and TxHmL starts March 1, 2023. EVV Operations will be posting the updated bill codes, including helpful information to avoid future payment denials or recoupments, following the publication of other HHSC materials.
For other EVV questions, email the EVV Operations inbox.
For questions about Individualized Skills and Socialization services, email the Long-Term Services and Supports Policy inbox.
December 17th, 2022
EVV Training Updates
This notice from HHSC lists Electronic Visit Verification training updates for program providers, financial management services agencies and Consumer Directed Services employers required to use EVV.
Resources from the following training webinars are now available in the HHS Learning Portal by selecting EVV Policy Training – Webinar Recordings FY23:
- Español – EVV Compliance for CDS Employers (PDF) – Aug. 25 non-required training webinar
- Annual EVV Policy Training for Program Providers and FMSAs – Sept. 30 and Oct. 27 webinars
If new to EVV and need to complete the EVV policy training requirement, complete one of the applicable computer-based training courses located in the HHS Learning Portal:
- EVV Policy Training for Program Providers and FMSAs FY23
- Initial EVV Policy Training for CDS Employers FY23
An account is required to access the training webinar resources and CBTs, including to obtain a certificate of completion. Note that a “non-required training” does not include a completion certificate because it is considered optional training. Reference the EVV HHS Learning Portal Guide (PDF) for instructions.
For more information on EVV training requirements, reference section 4200 from the EVV Policy Handbook.
Sign up for GovDelivery to receive EVV updates, such as training updates, by email.
Email EVV Operations for questions.
2023 EVV Operational Readiness Review Session & Business Rules for Proprietary Systems Version 3.0
EVV Operations has posted the following notice: Notice of 2023 EVV Operational Readiness Review Sessions and EVV Business Rules for Proprietary Systems Version 3.0 (PDF).
This notice is to inform program providers and financial management services agencies about the publication of the 2023 Operational Readiness Review Sessions, as well as the new EVV Business Rules for Proprietary Systems Version 3.0.
EVV Guidance on Program and Service Requirements for Schedules
HHSC has published the document, Program and Service Requirements for Schedules (PDF), under the Resources section on the Electronic Visit Verification web page. This document describes HHSC requirements related to using schedules in the EVV system.
Email HHSC EVV Operations for questions.
December 1st, 2022
Reminder for STAR+PLUS, STAR Kids and STAR Health: New EVV Bill Codes and Modifier Combinations Effective Dec. 1
As a reminder, starting Dec. 1, new Electronic Visit Verification personal care services Healthcare Common Procedure Coding System and modifier combinations will be effective for:
- STAR+PLUS
- STAR Kids
- STAR Health
Refer to HHSC’s Oct. 31 notice for more information.
Contact your managed care organization for questions about these updates. Refer to the last page of the EVV contact guide (PDF) for MCO contact information.
December 1st, 2022
HCS and TxHmL Updates
The effective dates were updated for HCS and TxHmL services.
Refer to the bill codes table’s revision history dated Dec. 1, 2022, for more information.
For questions, email EVV Operations.
October 16th, 2022
Potential Electronic Visit Verification Changes Coming in 2023
The purpose of this notice is to inform stakeholders that HHSC’s contract for the current Electronic Visit Verification vendor systems (AuthentiCare and Vesta EVV) is scheduled to expire on Aug. 31, 2023.
On April 26, 2022, HHSC posted a competitive solicitation on the Electronic State Business Daily for EVV System Management Services. Contractor responsibilities will include:
- Providing and managing a single EVV vendor system
- Review and approval of provider-operated EVV proprietary systems If you have an outside vendor (proprietary vendor), these will be reviewed as well.
- Coordinating EVV system integration with the EVV aggregator
- Providing operational and technical support for the functions listed above
Notification of contract award is anticipated in March 2023.
HHSC, at its sole discretion, may publish updates about the anticipated award date to the Procurement Forecast on the HHS Procurement Opportunities web page. Respondents are responsible for periodically checking the ESBD and the HHSC Procurement Forecast web page for updates.
HHSC must maintain the confidentiality and integrity of the procurement process; therefore, no additional information is available at this time. HHSC will provide more information in future announcements.
Email questions about this solicitation to Andrick Reese.
September 25th, 2022
EVV Updates for HCS and TxHmL Program Providers and FMSAs
HHSC and the Texas Medicaid and Healthcare Partnership posted helpful information for Home and Community-based Services program providers, Texas Home Living program providers and financial management services agencies required to use Electronic Visit Verification.
HHSC Notice
This notice is to help program providers and FMSAs that are receiving EVV mismatches for Day Habilitation services.
Refer to the Sept. 15 notice for information on billing requirements, such as which Day Habilitation bill codes to use.
TMHP Notice
This notice provides information about EVV requirements for In-Home Day Habilitation and about EVV claims matching starting Nov. 1 for HCS and TxHmL.
Refer to the Sept. 19 notice for more information and resources.
Email EVV Operations for questions.
September 25th, 2022
EVV Claims Matching Refresher for HCS and TxHmL
Electronic Visit Verification claims matching for Home and Community-based Services and Texas Home Living will begin for dates of service starting Nov. 1.
To help prepare, the Texas Medicaid and Healthcare Partnership will host a refresher webinar on Oct. 13, for:
- HCS program providers
- TxHmL program providers
- Financial management services agencies
Refer to TMHP’s Sept. 15 notice for more information and to registerl
Click here for more information
September 18th, 2022
EVV Compliance Job Aids Updated
The Electronic Visit Verification Compliance Job Aids have been updated. They are in the compliance section on the EVV web page.
The job aids were simplified and provide updated information about the following EVV Compliance standards:
- EVV Usage Scores and reviews
- Required free text reviews
- Landline phone verification reviews
August 31st, 2022
Annual EVV Policy Webinars for Program Providers & FMSAs
July 28th, 2022
EVV Portal and Training Updates
Texas Medicaid and Healthcare Partnership updated the Electronic Visit Verification Portal and related training materials on July 14.
Refer to the EVV Portal and Training Updates notice on TMHP’s EVV webpage for more information.
July 5th, 2022
EVV Claims for HCS and TxHmL Will Deny for Dates of Service Starting Sept. 1
HHSC has extended the start date when Electronic Visit Verification claims for Home and Community-based Services and Texas Home Living will deny for no matching EVV visit. This will begin for the dates of service of Sept. 1, 2022, and after.
The extension gives HCS and TxHmL program providers and financial management services agencies more time to improve their claims matching. Texas Medicaid and Healthcare Partnership will provide more outreach and training on this topic. Trainings will be announced at a future date.
Refer to the HCS and TxHmL Best Practices to Avoid EVV Claim Mismatches (PDF) for technical guidance.
HCS and TxHmL EVV claims must continue to be submitted through the Client Assignment and Registration System or TMHP.
- Submit EVV claims to CARE for dates of service before May 1, 2022.
- Submit EVV claims to TMHP for dates of service of May 1, 2022, and after.
Program providers, FMSAs and Consumer Directed Services employers must continue to use EVV during this period. However, HCS and TxHmL claims will not be denied for an EVV mismatch. HCS and TxHmL claims during this period are still subject to HHSC provider fiscal compliance reviews conducted by HHSC Provider Fiscal Compliance..
Email EVV Operations for questions.
July 1st, 2022
EVV Claims for HCS and TxHmL Will Deny for Mismatched Visits Starting July 1
Starting July 1, Electronic Visit Verification claims for Home and Community-based Services and Texas Home Living must have a matching EVV Visit, or claims will deny.
Refer to the June 20 notice for more information and resources.
Email EVV Operations for questions.
June 12th, 2022
EVV Portal and Training Updates
Texas Medicaid and Healthcare Partnership updated the Electronic Visit Verification Portal and related training materials on June 9.
There are also two new visit rejection codes related to EVV system transfers.
Refer to the EVV Portal and Training Updates notice on TMHP’s EVV webpage for more information.
June 6th, 2022
EVV Policy Handbook Revision and Training Updates
The Electronic Visit Verification Policy Handbook has been revised.
Revisions include:
- Adding new sections for the Consumer Directed Services option.
- Updating Schedules policy.
- Updating Visit Maintenance Reduction Features policy.
These revisions are effective June 1 and are outlined in the new revision log (PDF), located on the EVV webpage.
The handbook’s policies include EVV standards and policy requirements for:
- Program providers
- Financial Management Services Agencies
- Consumer Directed Services employers
- Payers, such as HHSC and managed care organizations
Computer-based training on the HHS Learning Portal were updated to include the policy revisions.
- EVV Policy Training for Program Providers and FMSAs CBT
- Initial EVV Policy Training for CDS Employers CBT
- Note: The updates to the Spanish CBT will publish in June.
Email HHSC EVV Operations for questions about this notice.
May 30th, 2022
EVV Claims Matching for HCS and TxHmL Will Resume July 1
Electronic Visit Verification claims matching will resume for all Home and Community-based Services and Texas Home Living billing code combinations with dates of service of July 1, 2022 or after.
HHSC will post another notice with more information and resources to avoid EVV claims mismatches before July 1, 2022.
Email EVV Operations for questions about this notice.
May 8th, 2022
EVV Portal and Training Updates
Texas Medicaid and Healthcare Partnership updated the Electronic Visit Verification Portal and related training materials on April 29.
Refer to the EVV Portal and Training Updates notice on TMHP’s EVV webpage for more information.
Email TMHP EVV Operations with questions
March 7th, 2022
EVV Notice for HCS/TxHmL Program Providers
The migration of Home and Community-based Services (HCS) and Texas Home Living (TxHmL) forms and claims entry to Texas Medicaid & Healthcare Partnership (TMHP) has been moved from March 1, 2022, to May 1, 2022. The postponement allows more time for program providers to set up the necessary TMHP accounts and take relevant training courses. HCS and TxHmL program providers must continue to use the Client Assignment and Registration (CARE) system to submit claims using existing billing code combinations for service groups 12 and 15 for dates of service prior to May 1, 2022.
HHSC is aware that some program providers updated authorizations in the EVV systems to reflect the new billing code combinations for service groups 21 and 22 that were scheduled to take effect March 1. To avoid the re-entry of authorizations, HHSC and TMHP will take the following actions:
- By March 4, the EVV Aggregator will accept billing code combinations for service groups 12, 15, 21 and 22 on EVV visits for dates of service through April 30, 2022, to prevent visit rejections.
- For dates of service on or after May 1, 2022, the EVV Aggregator will only accept billing code combinations for service groups 21 and 22.
- Turn on the EVV07 claims matching bypass for all HCS and TxHmL billing code combinations to avoid claim denials through May 31, 2022.
- Claims matching for all HCS and TxHmL billing code combinations will resume June 1, 2022.
- Publish an updated EVV Service Bill Codes Table to reflect these changes.
HCS and TxHmL claims will not be denied for an EVV mismatch. HCS and TxHmL claims during this period are still subject to HHSC provider fiscal compliance reviews conducted by HHSC Provider Fiscal Compliance.
**For visits that have been rejected by the aggregator due to incorrect billing code combinations, program providers must re-export the visit and ensure it is accepted in the EVV aggregator prior to submitting claims.
Please refer to HHSC’s ‘Continue Submitting Claims and Forms Using CARE System Until May 1, 2022’ notice for more information.
For technical questions related to the EVV Aggregator, contact TMHP. For other general EVV inquiries, contact HHSC EVV Operations.
March 3rd, 2022
EVV Policy Handbook Revisions Now Available
HHSC revised sections and appendices of the Electronic Visit Verification Policy Handbook.
The handbook includes EVV standards and policy requirements for:
- Program providers.
- Financial Management Services Agencies.
- Consumer Directed Services employers.
- Payers, such as HHSC and managed care organizations.
The revisions are effective March 1 and are briefly described in the 22-2 notice. For more information about the policy changes, refer to the new revision log (PDF) located on the EVV webpage.
Email HHSC EVV Operations with questions.
February 28th, 2022
EVV Portal and Training Updates
Texas Medicaid and Healthcare Partnership updated the Electronic Visit Verification Portal and related training materials on Feb. 28.
For more information, refer to the EVV Portal and Training Updates article on TMHP’s EVV webpage.
For questions, email TMHP EVV Operations.
January 8th, 2022
EVV Policy Handbook Revisions – Jan. 7th, 2022
HHSC revised parts of the Electronic Visit Verification Policy Handbook. These revisions are effective Jan. 7 and are listed in Revision Notice 22-1.
The handbook’s policies include EVV standards and policy requirements for:
- Program providers.
- Financial Management Services Agencies.
- Consumer Directed Services employers.
- Payers, such as HHSC and managed care organizations.
For questions, email HHSC EVV Operations.
November 21st, 2021
EVV Portal and Training Updates for November 2021
Texas Medicaid and Healthcare Partnership made improvements to the EVV Portal and related training materials on Nov. 11.
For more information, access the November 2021 EVV Portal and Training Updates article on TMHP’s EVV webpage.
FYI- When you click on the link above for updates from HHSC, please be sure to scroll to the bottom and click on “accept” as this is a disclaimer page. You must do this 1st. I have received some comments that some providers get confused when they see this page on the EVV website first pop up and they think they are on the wrong page, or there is a problem with the website page, etc…
Email TMHP with questions about these updates.
November 18th, 2021
Revised EVV Policy Handbook Now Available
The Electronic Visit Verification Policy Handbook was revised.
The handbook’s policies are effective Nov. 1, 2021 and include EVV standards and policy requirements for:
- Program providers
- Financial Management Services Agencies
- Consumer Directed Services employers
- Payers such as HHSC and managed care organizations
The handbook replaces policies previously on the HHSC EVV webpage. See EVV Policy Handbook Revisions – November 2021 (PDF) for differences between previously published policies and the revised handbook.
The following computer-based training courses on the EVV Training page of the HHS Learning Portal now reflects the revised EVV Policy Handbook:
- Initial EVV Policy Training for CDS Employers
- EVV Policy Training for Program Providers and FMSAs
Use the applicable checklist within EVV Training Requirements Checklist (PDF) for EVV training requirements and completion options.
Email questions to HHSC EVV Operations.
November 17th, 2021
EVV Visit Maintenance Unlock Request Updates
HHSC published EVV Visit Maintenance Unlock Request spreadsheet updates.
These updates let the user request corrections to data element(s) on an EVV visit transaction(s) after the visit maintenance time frame has expired.
Program providers, Financial Management Services Agencies and Consumer Directed Services employers must use the request spreadsheets found on the EVV webpage.
The updates to the program provider and FMSA Request (Excel) include:
- New fields
- Added drop-down lists to applicable fields
- Updated and simplified field headers
- Revised instructions to:
- Reflect EVV policy updates
- List detailed steps and notes to complete the Request
The new Request for Consumer Directed Services employers (Excel) include:
- A new request spreadsheet for CDS employers who selected Option 1 on Form 1722, Employer’s Selection for EVV Responsibilities, to complete visit maintenance. This includes:
- Drop-down lists for applicable fields
- Sections for CDS employers and payers to complete
- Instructions reflect:
- EVV policy updates
- Detailed steps and notes to complete the request
Review the instructions on the spreadsheets for more information.
Email questions to your payer, either HHSC or a managed care organization
July 4th, 2021
EVV Visit Maintenance Policy Now Available
The Electronic Visit Verification Visit Maintenance Policy (PDF) is now available on the HHSC EVV webpage. The policy is effective July 1, 2021 and:
- Requires the program provider, Financial Management Services Agency or Consumer Directed Services employer to ensure each EVV visit transaction is complete, accurate and validated.
- Incorporates the Visit Maintenance: Last Visit Maintenance Date Policy.
- Incorporates the Visit Maintenance Unlock Request Policy.
- Includes the new visit maintenance time frame of 95 calendar days. (previously 60 calendar days) from the date of service delivery.
Email questions to HHSC EVV Operations at EVV@hhs.texas.gov.
July 4th, 2021
HHSC EVV Webpage Updates Now Available
The Texas Health and Human Services Commission updated and archived web sections and content, updated and added additional information related to the 21st Century Cures Act (Section 12006) and added new resources for the following Electronic Visit Verification webpages:
- EVV Home page,
- EVV Consumer Directed Services Option,
- EVV Cures Act,
- EVV Training and
- EVV Proprietary Systems.
Email questions to HHSC EVV Operations at EVV@hhs.texas.gov.
July 3rd, 2021
Revised EVV Visit Transaction Rejection Guide Now Available
The Electronic Visit Verification Visit Transaction Rejection Guide (PDF) was revised and is now available.
The guide provides step-by-step instructions for program providers and Financial Management Services Agencies to identify and correct issues that result in transaction rejections in the EVV system.
The guide is published on TMHP’s EVV Training webpage.
April 17th, 2021
EVV Policy Training for CDS Employers Now Available in Spanish
The computer-based training course, Initial EVV Policy Training for CDS Employers, is available in Spanish on the HHS Learning Portal.
To translate the HHS Learning Portal to Spanish, select Español from the drop-down menu in the upper left-hand corner of the webpage.
The policy training is tailored to the selection on Form 1722, Employer Selection for Electronic Visit Verification Responsibilities.
Registrants are not required to complete the Form 1722 Pre-Course Survey.
Follow the instructions throughout the course to complete and receive certification.
Email the HHSC EVV Mailbox for questions about EVV policy training.
March 16th, 2021
HHSC Publishes EVV Requirements of Signatures on Enrollment Documentation (IL 2021-13)
HHSC has published IL 2021-13, EVV Notification Requirement (PDF), replacing IL 2020-01.
The letter addresses revisions on instructing LIDDAs on the requirements of signatures on enrollment documentation.
It also addresses new activity requirements for HCS, TxHmL, CDS program providers and LIDDA service coordinators.
For questions, email HCS Policy or CDS.
March 10th, 2021
Temporary EVV Policies for the Feb. 2021 Severe Winter Weather
In response to the recent severe winter weather, HHSC issued Temporary EVV Policies for Severe Winter Weather (PDF).
The flexibilities are for dates of service from Feb. 10, 2021 through Feb. 24, 2021.
The flexibilities are for program providers, financial management services agencies and consumer directed services employers required to use EVV.
Email questions to the HHSC EVV Mailbox.
February 7th, 2021
EVV Refresher Training on Feb. 19
The Texas Health and Human Services Commission and Texas Medicaid & Healthcare Partnership are hosting an Electronic Visit Verification webinar.
This training is a refresher and covers topics for Home and Community-based Services program providers, Texas Home Living program providers and financial management services agencies who submit EVV claims for HCS and TxHmL EVV-required services.
The training is not required and is not a substitute for annual EVV training requirements.
Certificates of completion will not be issued.
Attendees will have the opportunity to submit questions throughout the training.
Both HHSC and TMHP will conduct a live question and answer session.
The registration link is below and provides details, such as agenda topics.
HCS/TxHmL EVV Refresher Training – Claims Submission/Claims Matching Policies & Best Practices to Avoid EVV Claim Mismatches
Friday Feb. 19
10 a.m. – Noon
Register for the webinar.
Reminder: Entering Schedules for EVV-Required Services
The Electronic Visit Verification system allows Home and Community-based Services, Texas Home Living program providers, CDS Employers and Financial Management Services Agencies to enter schedules for EVV-required services. This is not an HHSC requirement. Program Providers, FMSAs and CDS employers can choose to enter a schedule into the EVV system.
EVV is only required for the following services:
- Community First Choice Personal Assistance Services/Habilitation
- In-Home Day Habilitation in own home or family home settings
- In-Home Respite in own home or family home settings
Email hcspolicy@hhsc.state.tx.us or txhml@hhsc.state.tx.us with questions.
January 24th, 2021
EVV Portal and Training Updates for January
On Jan. 14, Texas Medicaid & Healthcare Partnership made improvements to the Electronic Visit Verification Portal by updating the EVV Reason Code Usage and Free Text Report and updated the related training materials.
Read the TMHP article EVV Portal Improvements and Training Updates for details.
Email TMHP with questions about these updates.
January 24th, 2021
HCS & TxHmL Best Practices to Avoid EVV Claim Mismatches for CFC PAS/HAB Services
HHSC has published Best Practices to Avoid Electronic Visit Verification Claim Mismatches for Home and Community-based Services and Texas Home Living (PDF) program providers and financial management services agencies.
The best practices help HCS and TxHmL providers avoid claim denials related to EVV.
The best practices are linked above and on the HHS EVV Training webpage in the Best Practices section.
Email questions about EVV policy to HHSC EVV.
January 18th, 2021
EVV Compliance Oversight Reviews Delayed for EVV Usage and Misuse of EVV Reason Codes
HHSC told managed care organizations to delay compliance oversight reviews for EVV Usage and Misuse of EVV Reason Codes. Evaluation of visit data collected during the grace period ensures the compliance measures continue to align with current EVV policy.
EVV Usage and Misuse of EVV Reason Codes reviews for the compliance grace period ended on Aug. 31, 2020 for:
- EVV visits with Sept. 1, 2019 to Aug. 31, 2020 dates of service.
- Program providers required to use EVV by state law before the Cures Act Implementation identified on pages 3 and 4 of the Programs and Services Required to Use EVV (PDF) document.
Next Steps
- HHSC will notify program providers 90 calendar days before reviews begin for EVV Usage and Misuse of EVV Reason Codes for EVV visits with dates of service on and after Sept. 1, 2020.
- HHSC and MCOs will continue reviews for EVV Landline Phone Verification and Required Free Text.
- Program providers can use the EVV Usage Report, and EVV Reason Code Usage and Free Text Report in the EVV Portal to track these compliance measures.
Program providers can contact their payer or email HHSC EVV with their questions or concerns.
January 10th, 2021
![]()
EVV Notification Requirement for HCS/TxHmL Program Providers
HHSC has published IL 2021-01 Electronic Visit Verification Notification Requirement (PDF).
The letter informs HCS and TxHmL program providers they are now required to use the EVV system for CFC PAS/HAB, in-home respite, and day habilitation provided in the home of an individual who has a residential location of “own/family home.”
Texas Government Code, §531.024172(c), requires that HHSC inform an individual who receives a service requiring the use of EVV that the individual is required to comply with the EVV system. HHSC has developed a form for providers to comply with this statute.
The Electronic Visit Verification Responsibilities and Additional Information form is included with the IL 2021-01 (PDF).
January 4th, 2021

EVV for HCS and TxHmL providers has gone live since January 1, 2021 (includes CDS and FMSA’s)
Resources for providers, including escalation processes, regarding EVV questions & concerns:
- HHSC EVV Operations and TMHP have developed two Contact Guides:
- To assist program providers and FMSAs identify and correct EVV visit transaction rejections, TMHP created the EVV Visit Transaction Rejection Guide (PDF).
- Email HHSC EVV Operations, Electronic_Visit_Verification@hhsc.state.tx.us, regarding:
- EVV Policy and Compliance Questions
- General EVV Inquiries and Complaints
- Good idea to CC your provider association, if you are a member (PPAT, PACSTX..)
- Email TMHP, EVV@tmhp.com, regarding TMHP issues and EVV vendor complaints/issues.
- Copy Evan Wilkerson on urgent TMHP or EVV vendor issues.
December 20th, 2020
Cures Act EVV:
Preparing for Jan. 1, 2021 Implementation
HHSC will require Electronic Visit Verification for all Medicaid personal care services beginning on Jan. 1, 2021. This requirement is mandated by the federal 21st Century Cures Act. If HHSC does not comply, Texas will lose federal funding for Medicaid services.
Beginning Jan. 1, 2021:
- Document all delivery visits for an EVV-required service in the EVV system. EVV-required services on the Programs, Services, and Service Delivery Options Required to Use EVV (PDF) document.
- An EVV-required service claim will be paid only if:
- The EVV visit transaction that supports the claim is accepted into the EVV Portal before claim submission.
- The claim receives an “EVV01 – EVV Match” result code in the EVV Portal after the claims matching process is performed.
Program providers and financial management services agencies must complete the following before Jan. 1, 2021, to avoid impacts to EVV claims payment:
- EVV system onboarding. This includes system setup and training.
- If an EVV vendor system is selected from the state vendor pool, the EVV vendor provides the training. Refer to the TMHP EVV Vendors webpage for more information about EVV vendors and their contact information.
- If an EVV proprietary system is selected, the program provider or FMSA handles system training.
- EVV training requirements outlined in the Cures Act EVV: Training Requirements Checklists (PDF).
- Document all visits for EVV-required services in the EVV system.
CDS employers must complete the following before Jan. 1, 2021, to avoid delays in payment to their CDS employees:
- Form 1722, Employers Selection for Electronic Visit Verification Responsibilities. Submit the signed form to their FMSA, which is the company that helps with CDS employee payroll.
- EVV system onboarding. CDS employers can contact their FMSA to complete onboarding and schedule training.
- EVV training requirements outlined in the Cures Act EVV: Training Requirements Checklists (PDF).
- Employees must start documenting all visits for EVV-required services in the EVV system.
HHSC is providing the following support to program providers, FMSAs, and CDS employers. This is to reduce impacts to claims payment and payment to CDS employees as they adjust to the new EVV requirements.
- If a visit is not captured through an electronic verification method, enter the visit manually into the EVV system and confirm acceptance into the EVV Portal to avoid claim denials. Instructions for manually entering a visit are posted in the following locations:
- DataLogic/Vesta EVV system.
- First Data/AuthentiCare EVV system in the “Custom Links” section.
- HHSC has published Best Practices to Avoid EVV Claim Mismatches (PDF) to help program providers and FMSAs ensure a claim is not denied for reasons related to EVV.
- HHSC has issued the 90 Day Visit Maintenance Temporary Policy (PDF). extending the time to complete visit maintenance for dates of service between Jan. 1, 2021 and March 31, 2021.
- An EVV compliance grace period will be applied for one year to all Cures Act EVV Expansion services with dates of service between Jan. 1, 2021 and Dec. 31, 2021 for the compliance measures listed in EVV Compliance Oversight Reviews Policy (PDF).
The EVV Contact Information Guides provide points of contact for EVV-related questions and issues:
- CDS Employer EVV Contact Information Guide (PDF)
- Program Provider and FMSA Contact Information Guide (PDF)
Visit the HHS EVV website for more information.
November 28, 2020
HCS and TxHmL CARE Service Authorization instructions for EVV
HCS and TxHmL are required to manually enter each individual’s service authorization in the EVV Vendor System.
Providers can find instructions here on how to find their service authorizations in CARE.
If additional assistance is needed after the service authorization is obtained, program providers can contact their EVV vendor for further instructions.
Existing EVV Users: Temporary EVV Policies for COVID-19 to End Dec. 31
HHSC is extending the Temporary EVV Policies for COVID-19 (PDF) through Dec. 31, 2020 for program providers currently required to use Electronic Visit Verification. HHSC will end the temporary policies after Dec. 31, 2020.
Program providers submitting EVV claims for dates of service on and after Jan. 1, 2021:
- Must ensure a matching EVV visit transaction is accepted in the EVV Portal before billing the claim, or the claim will be denied.
- Will no longer receive an EVV07 match code in the EVV Portal.
- Will no longer have 180 days to complete visit maintenance.
Reminder: HHSC extended the practice period for the Cures Act Expansion. Claims for EVV services included in the Cures Act Expansion, will be denied without a matching EVV visit transaction for dates of service on and after Jan. 1, 2021.
Best Practices for Temporary EVV Policies for COVID-19
Program providers should continue to follow the Best Practices for Temporary EVV Policies for COVID-19 (PDF) to avoid recoupments for claims submitted between March 21, 2020 and Dec. 31, 2020.
Contact your payer for questions or email HHSC EVV.
| HCS and TxHmL Program Providers Required to Select an EVV Vendor | ||||||||
| 11/18/2020 | ||||||||
|
Deadline Approaching Soon!!
Remember everyone: Effective Dec. 1, HHSC will require HCS and TxHmL program providers to use EVV for the following services:
- Community First Choice Personal Assistance Services/Habilitation (CFC PAS/HAB)
- In-Home Respite
- In-Home Day Habilitation (Own Home or Family Home only)
HCS and TxHmL program providers are required to select an EVV vendor and complete EVV training to meet the Dec.1 deadlines. The requirement to select an EVV vendor and complete training applies to all contracted HCS and TxHmL program providers.
Beginning Dec. 1, 2020, service claims for CFC PAS/HAB will be denied by the claims adjudication system and not paid by HHSC if the program provider has not onboarded with an EVV vendor.
Click here to read IL 20-07 (PDF) for more information about selecting an EVV vendor and completing training to be EVV-compliant by the Dec. 1 deadline.
Contact EVV if you have questions about EVV requirements.
Oct. 11th, 2020
EVV Revised Policies Effective Oct. 1
HHSC has revised the following electronic visit verification policies, effective Oct. 1. The information is for program providers and financial management services agencies. It is on the Policy section of the HHS EVV webpage.
The policy:
- Includes additional EVV claims match result codes
- Identifies exceptions to the claims matching process
Claims Submission Policy (PDF)
- The policy includes detailed information about the requirement to submit claims for EVV-required services to the appropriate HHSC claims management system.
- The EVV Billing Policy has been incorporated into the policy.
Email HHSC EVV with your questions.
Oct. 11th, 2020
Updated EVV Service Bill Codes Table Effective Oct. 1
The EVV Service Bill Codes Table is updated effective Oct. 1. The table is on the HHS EVV webpage in the Service Bill Codes Table section. See:
- Below for the major updates
- The Revision History in the table for a complete list of the changes
Program providers and FMSAs can refer to the table for the list of EVV-relevant services and bill code information to avoid EVV visit transaction rejections and EVV claim mismatches.
Units Matching
The updated table shows that during the EVV claims matching process for dates of service on and after Oct. 1, billable units on the EVV visit transaction will be matched to billed units on the claim for:
- EVV-relevant services delivered through the service responsibility option in Managed Care and fee-for-service Long-Term Care programs.
- Community First Choice Personal Assistance Services/Habilitation in the Community Living Assistance and Support Services program (Service Group 2, Service Code 10CFC T2026).
Home and Community-based Services and Texas Home Living Programs
- The table clarifies the EVV Requirements for In-Home Day Habilitation in the HCS Program when In-Home Day Habilitation and In-Home Respite services are provided in a member’s own home or family home setting.
- The “Claims Place of Service” column in the “CARE LTC FFS” tab only includes place of service code 12 (Home Location) because EVV is only required to capture services that need an in-home visit.
HHSC is issuing this guidance from CMS to Home and Community-based Services program providers. It clarifies electronic visit verification requirements for in-home day habilitation.
All service events occurring on or after Dec. 1, 2020, for an EVV-required service, must be captured in the EVV system and accepted into the EVV Aggregator.
EVV is not required for In-Home Day Habilitation provided to someone in a:
- Three or four-person home
- Host home
- Companion care residential setting
EVV is only required for the following services:
- Community First Choice Personal Assistance Services/Habilitation
- In-Home Day Habilitation in own home or family home settings
- In-Home Respite in own home or family home settings
See IL 20-07 Electronic Visit Verification in the HCS and TxHmL Program (PDF) for information about EVV requirements.
Additional Guidance on Day Habilitation Services
Program providers billing claims for In-Home Day Habilitation services requiring EVV will continue to use the current claims procedure code, T2020. The EVV Service Bill Codes Table lists this code on the HHS EVV website.
HHSC is developing separate bill codes for Out-of-Home Day Habilitation and will provide guidance before implementing the new codes.
Email hcspolicy@hhsc.state.tx.us with questions.
No EVV For In-Home DH: 3 & 4-bed Homes or Host Homes
August 20th, 2020
HHSC just informed the three IDD associations that it received clarification from CMS that EVV will not be required for in-home day habilitation delivered in a three- or four-bed home or host home. HHSC will send notice regarding this to all affected stakeholders. This does however mean that In-Home DH provided in an individual’s “Own Family Home” will still require staff to utilize EVV.
CURES Act EVV Training is Underway for HCS/TxHmL Providers
Program providers and FMSAs affected by the Cures Act EVV expansion must complete EVV policy and EVV Portal training before Dec. 1, 2020, and then annually. See the EVV Required Training Checklist (PDF) for more information.
To meet the training requirement, program providers and FMSAs attending these webinars must:
- Register for Session 1.
- Register for Session 2.
- Attend both sessions from start to finish.
To register, click the links below:
FMSAs
- Session 1 – June 2, 2020 – 8:30 a.m. to 12:30 p.m.
- Session 2 – June 3, 2020 – 8:30 a.m. to 12:30 p.m.
HCS/TxHmL
Additional Training Opportunities
Program providers and FMSAs can also meet training requirements by completing computer-based training online in the HHSC Learning Portal and TMHP Learning Management System. HHSC and TMHP are planning additional live training events this fall and will provide more information when available.
Email TMHP for questions about registration or the EVV Portal.
Email questions about EVV training requirements.
For more Cures Act information, visit the HHS EVV Cures Act webpage.
If you miss the EVV training dates, you may take them on the HHSC learning portal:
https://learningportal.dfps.state.tx.us/
Please go to HHSC’s page on Electronic Visit Verification for the latest information/ updates to EVV. Please see Training & Joint Training pages from HHSC as well!
https://hhs.texas.gov/doing-business-hhs/provider-portals/long-term-care-providers/resources/electronic-visit-verification
Updated Timeline for Cures Act EVV Expansion
The updated timeline for expanding the Cures Act EVV requirement to all Medicaid personal care services is now available on the HHS Cures Act EVV website.
The timeline includes new information and resources about the EVV Practice Period beginning July 1, completing training requirements, and more.
This information is for Cures Act program providers and FMSAs (PDF) required to use Electronic Visit Verification by Jan. 1, 2021.
-
-
Providers currently required to use EVV must continue to use EVV under state law and HHSC policy. See the Programs and Services Currently Required to Use Electronic Visit Verification (PDF)
For questions about EVV vendors, email evv@TMHP.com
-
New EVV Proprietary System Onboarding Documents Available
TMHP has posted new information about the EVV proprietary system onboarding process on the TMHP EVV Proprietary Systems webpage.
The documents located in the Onboarding section provide an overview of the approval process that a program provider or FMSA must complete before using their own EVV proprietary system. For more information, refer to the article on the TMHP EVV website (PDF).
Resources
- Contact: Electronic_Visit_Verification@hhsc.state.tx.us
- Website: HHSC EVV Cures Act
Trainings Available:
EVV Policy Training (Provided by your payer)
- The HHSC EVV Policy computer-based training (CBT).
- The MCO Policy training. Contact your MCO for EVV Policy training opportunities.
EVV Aggregator and EVV Portal Training (Provided by TMHP)
There will also be instructor-led trainings (EVV Roadshow) in October. Find the schedule and register on the HHS Learning Portal.
Additional training resources are available on the HHSC EVV website and the TMHP EVV Provider Training webpage.
For questions about this alert, email Electronic_Visit_Verification@hhsc.state.tx.us.
Online, interactive EVV training courses are available
in the HHS Learning Portal and TMHP Learning Management System. Completing these courses help program providers meet EVV training requirements.
The HHS Learning Portal includes training about HHSC EVV Policy.
The TMHP Learning Management System includes training about:
- EVV Vendor Selection
- EVV Portal
- EVV Portal Standard Reports and Search Tools
- EVV Claims Submission and Billing
CLASS and DBMD Quarterly Webinar on March 19
February 28th, 2025
HHSC will be providing ongoing opportunities for CLASS and DBMD providers and FMSAs to hear about recent program updates.
CLASS and DBMD Quarterly Webinar
March 19, 2025 10–11:30 a.m.
Topics to be discussed will include:
- CLASS/DBMD — Upcoming form updates, June webinar.
- UR/PES — UR/PES responsibility changes.
- EVV — EVV updates.
- Fair Hearing — Fair hearings information.
Email CLASSPolicy@hhs.texas.gov and DBMDPolicy@hhs.texas.gov with any questions.
Documentary “Into the Spotlight” Released To The General Public
February 27th, 2025

Utilization Review Department News!
February 20th, 2025
HHSC Publishes Information on Waiver and Community Services Utilization Review Process
HHSC has published Information Letter 2025-02 Waiver and Community Services Utilization Review Process.
This letter provides a summary of the authority for conducting field utilization reviews in the Community Living Assistance and Support Services (CLASS), Deaf Blind with Multiple Disabilities (DBMD), Home and Community-based Services (HCS) and Texas Home Living (TxHmL) Programs.
There is also a link included in the letter, to the document that describes the Waiver and Community Services Utilization Review Process.
You can also click on the link to the summary of this field UR Review process here: https://www.hhs.texas.gov/sites/default/files/documents/field-ur.pdf
Employment Readiness Rates
February 18th, 2025
HHSC Publishes Payment Rates for Employment Readiness Services in DBMD, HCS, and TxHML Waiver Programs.
HHSC approved payment rates for for Employment Readiness Services in the Deaf-Blind with Multiple Disabilities (DBMD), Home and Community-Based Services
(HCS), and Texas Home Living (TxHmL) Waiver Programs effective Jan. 1, 2025.
More information about the approved payment rates is available on the HHSC Provider Finance Department webpage.
The Employment Readiness Services payment rates, effective Jan. 1, 2025, can be accessed on the HHSC Provider Finance Department webpage.
See Jan 2025 HCS & TxHmL rates here including Employment Readiness rates for HCS: HCS Rates-Jan-2025
For TxHmL: TxHmL Rates-Jan-2025
Letter To The Providers From Twogether Consulting: February 15th, 2025
February 15th, 2025

From Twogether Consulting!
Hello Everyone!
Hope everyone had a wonderful Valentine’s weekend. I feel like this month is flying by. Don’t forget we have a “Pop-Up”webinar on Feb. 21st,2025 from 1pm-3:30pm. This is especially great session for any new providers, as well as new program managers and case managers:“Care Coordination Basics: Admission, Post- Admission & Other Follow-Up Required” (HCS)
Twogether Consulting will be adding additional ICF and HCS webinars for March on the website later this week. Don’t forget we have a live 2-day training in Austin at the PPAT Office (Private Provider’s Association of Texas) for HCS Care Coordination (Case Management) on February 27th & 28th, 2025. Seating is limited, so please contact Megan Jones as soon as possible if you want to sign up. We will also be adding some live training sessions for Nurses in HCS/TxHmL programs in March in the Austin area. Look for the sessions to be posted in the near future on our home page calendars-www.twogetherconsulting.com.
If you missed the webinar for ICAP’s/IDRC’s/LON’s (ICF Program), please let us know. We do have the recorded session. We do have a variety of other pre-recorded trainings for program managers, case managers and nurses, so feel free to email us at info@twogetherconsulting.com to inquire. Let us know what areas of training you would like, to help us plan future sessions.
Please see our “Updates” section of the website for the latest news for IDD providers.

Medical Care Advisory Committee (MCAC) met Thursday, February 13, 2025
February 15th, 2025
Spotlight Musical Theater Presentation in Dallas February 22nd, 2025
February 14th, 2025
Belong Disability Ministry celebrates 15 years of Spotlight Musical Theater with a new production, “I’m on My Way” on Saturday, February 22 from 5:00 – 7:00pm at Highland Park United Methodist Church. This comedic, yet touching musical shares captivating stories of what it’s like to live with a disability through a series of DART rides. Join us in a theatrical display that features real-world scenarios, upbeat original music, and a journey in finding courage during the tough times of life. Purchase tickets HERE. For more about Spotlight Theater, please click on this Youtube link, for a newscast story about their documentary: https://www.youtube.com/watch?v=tf4lAoBuhNY
5-Year Children’s Behavioral Health Strategic Plan
February 8th, 2025
The Texas Health and Human Services Commission (HHSC) has published the 2024 Children’s Behavioral Health Strategic Plan (PDF).
The five-year plan is intended to foster an environment in which Texas children and their caregivers, based on identified need, have access to compassionate, comprehensive, and innovative behavioral health care, that will help develop their resilience and enable them to thrive emotionally, mentally, and socially.
The plan was developed by the Texas Statewide Behavioral Health Coordinating Council’s Children’s Behavioral Health Strategic Plan Subcommittee and is specific to the behavioral health of children and youth.
If you have any questions or comments, please email mentalhealth_sbhcc@hhs.texas.gov.
HHSC Publishes PL 2025-01: New Emergency Communication Tool For Long-Term Care Providers
January 19th, 2025
![]()
New Emergency Communication Tool – AlertMedia.
HHSC Publishes PL 2025-01 New Emergency Communication Tool – AlertMedia. This provider letter informs providers of the emergency communication system called AlertMedia, how it will be used, and their responsibility in signing up for the system.
HHSC will use this system to send emergency and outreach notifications through email, text, voice calls, and app push if available.
AlertMedia Joint Provider Trainings in January and February 2025
AlertMedia: Be Prepared. Stay Informed.
Friday, Jan. 24
1:30–2:30 p.m.
Register here for the webinar.
AlertMedia: Be Prepared. Stay Informed.
Wednesday, Feb. 5
10–11 a.m.
Register here for the webinar.
November 10th, 2024
REMINDER TO ALL LONG-TERM CARE PROVIDERS, BLACKBOARD CONNECT ENDED OCT. 31ST, 2024!
The current emergency communication system (Connect) for long-term care providers ended on Oct. 31 and will be replaced by the new system (AlertMedia), which is anticipated to go live no later than Dec. 1.
During this gap, no emergency communication system will be in place, so HHSC will communicate with providers through alerts, email and phone calls. Providers must respond to any request for information related to emergency preparedness and follow any instructions from HHSC.
Once AlertMedia is in place, HHSC will issue a separate communication on how to use the new system. Providers will be required to register in AlertMedia as defined by their Texas Administrative Code rule.
Free Web-Based Long-Term Care Educational Opportunities: Continuing Education Credit Available
January 19th, 2025
The Texas Health and Human Services Commission and the University of Texas at Austin School of Nursing are pleased to announce a collaborative effort to improve long-term care in Texas. This partnership includes updating eight web-based modules delivering best practices education to providers of long-term care in Texas nursing homes.
The Long-Term Care modules are:
-Infection Prevention and Control.
-Reducing Antipsychotic Use in Long-Term Care Facilities.
-Culture Change for Person-Centered Care.
-Quality Improvement.
-Advanced Geriatric Practice.
-Transition to Practice.
-Intellectual and Developmental Disabilities.
-Mental Health with Aging and Severe Mental Illness.
Each module provides education and resources for physicians, nurses, pharmacists, direct care staff, residents, and their family members and will help guide the decision-making process and improve care using evidence-based best practices.

Continuing education credit is available for: registered nurses, certified nurse aides and licensed nursing facility administrators.
Registration is free.
For more information, visit the Johnson-Turpin Center: Continuing Nursing Education | School of Nursing.
Letter To The Providers From Twogether Consulting: January 16th, 2025

January 16th, 2025
From Twogether Consulting!
Howdy!
Hope everyone is well! Back to the grind for so many of us now that the holidays are over. Please be sure to check the HCS and ICF home pages on the HHSC website for any new changes in rules, regulations, news, provider letters, training opportunities and more. Remember that Employment Readiness Services kick in as of January 1st, 2025 on the IPC for HCS & TxHmL. See IL-2025-01.
Twogether Consulting will be offering HCS webinars again this February and some are posted in this newsletter and our website. We are happy to announce that we will also start offering ICF webinars again in February as well. Our newest edition, Jo Beth Collier will be our main presenter for the ICF sessions. She brings some incredible knowledge and years of expertise in the field and I am excited for her to be one of our webinar presenters. We plan to provide webinars for Administrators, QA staff, QIDP’s, Nurses and Direct Support Staff in the homes, so please click on our survey further down in the newsletter and give us your feedback on trainings you would like to see.
FYI- Remember that HCS/TxHmL Billing Guidelines were updated in January of 2025.
I will be setting up webinars for February for some possible live sessions in Houston and/or Austin. We do have a variety of pre-recorded trainings for program managers, case managers and nurses, so feel free to email us at info@twogetherconsulting.com to inquire. Let us know what areas of training you would like, to help us plan future sessions.
We do have our free provider resource webinar for January with Dr. Amanda Frias, OT posted on the website for January 30th, 2025 from noon-1pm. Please check out our home page at www.twogetherconsulting.com and click on our training calendars for more information on next year’s live webinars and live training.
Please see our “Updates” section of the website for the latest news for IDD providers.

Fair and Fraud Hearings Handbook Revised
January 15th, 2025
The Fair and Fraud Hearings Handbook updates Section 1240.
This revision is effective Jan. 17, 2024. Click this link to see the updates.
Letter To Providers From Twogether Consulting-January 7th, 2025

January 7th, 2025
From Twogether Consulting!
Happy Holidays!
Bon Jour and Happy New Year to all of you. I spent some of my final holiday time in Paris. It was wonderful and I was so glad I got to see some incredible places including the newly renovated Notre Dame Cathedral and eat some amazing food! I am feeling refreshed and am looking forward to coming home soon so I can assist providers with their needs.
Twogether Consulting will be officially open to provide services again as of January 13th, 2025. Thank you everyone for your patience during the holidays and we would be happy to assist you, so please feel free to email me at info@twogetherconsulting.com or my general email address, if you already have it. You can also contact meghanjones.tx@gmail.com to schedule an appointment or make an inquiry if you can’t reach me for some reason.
FYI- Remember that HCS/TxHmL Billing Guidelines were updated in January of 2025.
I will be setting up webinars for January and February shortly, as well as some possible live sessions in Houston and/or Austin. We do have a variety of pre-recorded trainings for program managers, case managers and nurses, so feel free to email us at info@twogetherconsulting.com to inquire. Let us know what areas of training you would like, to help us plan future sessions.
We do have our free provider resource webinar for January with Dr. Amanda Frias, OT posted on the website for January 30th, 2025 from noon-1pm. Please check out our home page at www.twogetherconsulting.com and click on our training calendars for more information on next year’s live webinars and live training.
Please see our “Updates” section of the website for the latest news for IDD providers.

Promoting Independence Plan: 2024 Report
January 6th, 2024
From HHSC:
The Promoting Independence Plan report has been publicly posted in accordance with Executive Order RP-13 and is now available for viewing
This plan outlines accomplishments in the last two years as well as key strategies and goals that support people with disabilities to live independently within their communities. Highlights of the 2024 plan include activities to expand and improve services and an overarching theme of collaboration between multiple state agency partners.
Please review the Promoting Independence Plan and explore how it aims to improve the quality of life for people with disabilities by promoting independent living across Texas.
View the report here: Click here to view the Promoting Independence Plan 2024.
The report can also be found on the HHSC Reports and Presentations website located here: Reports and Presentations | Texas Health and Human Services
If you have comments or questions, please email HHSCOfficeofDisabilityServicesCoordination@hhs.texas.gov
Extreme Winter Weather Emergency Resources & Considerations
December 30th, 2024

HHSC reminds long-term care facilities and agencies to review and update emergency plans for freezing temperatures and snow. Emergency plans for extreme weather should include the provider’s plan to address:
- Power loss.
- Water and food needs.
- Medical and pharmaceutical supplies.
- Communication to families and staff.
- Staffing shortages.
- Sheltering in place and evacuation, as applicable.
Providers must follow emergency preparedness rules and their own internal emergency preparedness policies and procedures.
Facilities with generators should perform any maintenance or needed testing while the weather is mild. This will ensure the equipment functions in case of extreme cold or power loss.
It’s important to review building integrity and identify any areas that may need repair, reinforcement, or weatherproofing. Multi-story buildings should review any other needed measures should evacuation be required and have a plan in place for how to move residents around or out of the building if there’s a loss of power.
Preparing for disaster is the most important step in protecting the Texans we serve and reducing the risk for loss of life.
Email questions to LTCRpolicy@hhs.texas.gov.
December 22nd, 2023
LTC Provider Resources During an Emergency
Long-term care providers impacted by the current severe weather event should be implementing emergency management plans. LTC providers in need of resources or assistance during an emergency, such as the current severe weather, are reminded that you can:
- Contact your LTCR regional office regarding events that are affecting residents (such as no heat, evacuation, frozen fire sprinkler systems, etc.). They can initiate an emergency request.
- Contact your local emergency management or Regional Advisory Council, who can initiate a STAR request.
- Contact your local power company if you are having power issues. Nursing facilities, assisted living facilities, and inpatient hospices should inform the power company that you are an LTC provider, as those providers are prioritized for service restoration per the Public Utility Commission rules.
- Contact your Texas Department of Emergency Management District Contacts if you are having challenges getting generator fuel.
If you need guidance or assistance in relocating residents, work with your LTCR Regional Director. All requests to exceed licensed capacity must be approved by the Director of Survey Operations. If your facility is projected to exceed its licensed capacity because it is accepting residents who have been evacuated from another facility, email Renee Blanch-Haley and include State Capacity Increase Request in the subject line.
Please refer to Provider Letter 2018-19 (PDF) as applicable and to your program’s rules for additional important information regarding emergency preparedness. If you have any questions, contact your LTCR regional office, email LTCR Policy Rules and Training or call 512-438-3161.
ISS (Individual Socialized Services) FAQ’s

December 26th, 2024
Individualized Skills and Socialization FAQ’s: Updated Dec 2024
HHSC Long-term Care Regulation updated the Individualized Skills and Socialization frequently asked questions document on December 4, 2024.
Read the FAQ here.
June 5th, 2023
HHSC’s Response to Three Recent ISS-Related Questions From Providers
Question 1: May an Individualized Skills and Socialization (ISS) provider charge families for after-hour care? Many times families cannot get off work at the time the program closes/services stop. Some providers will keep their doors open until 5 or 6 (with staff present of course), until families get off work. In these cases, the ISS providers charge families for that service.
HHSC’s Response: If the individualized skills and socialization provider is also the program provider, the program provider would not be allowed to charge additional fees outside of the established HCS Waiver Program Payment rates, located here. According to 40 TAC §9.178(o):
(o) The program provider must not assess charges against the individual’s personal funds for costs for items or services reimbursed through the HCS Program or through CFC.
Additionally, according to 26 TAC §263.2015:
The service limit for the combined total of on-site, off-site, and in-home individualized skills and socialization is:
(1) 1560 hours during an IPC year;
(2) six hours per calendar day; and
(3) five days per calendar week.
If the individualized skills and socialization provider is a contractor of the program provider, the provider’s costs must be considered reasonable and necessary in regard to the Medicaid cost/accountability reports. Unless the program provider agrees to pay a higher amount, the individualized skills and socialization provider must provide the service at or below the direct services portion of the applicable HCS Program rate.
According to 40 TAC §9.177(b):
(b) The program provider must employ or contract with a person or entity of the individual’s or LAR’s choice in accordance with this subsection.
(1) Except as provided by paragraph (2) of this subsection, the program provider must employ or contract with a person or entity of the individual’s or LAR’s choice to provide an HCS Program service or CFC service to the individual if that person or entity:
(A) is qualified to provide the service;
(B) unless the program provider agrees to pay a higher amount, provides the service at or below:
(i) for any service except CFC ERS, the direct services portion of the applicable HCS Program rate; and
(ii) for CFC ERS, the reimbursement rate; and
(C) is willing to contract with or be employed by the program provider to provide the service in accordance with this subchapter.
As part of agreeing to provide the HCS Program service at the direct services portion of the applicable HCS Program rate, the individualized skills and socialization provider would not be allowed to charge an individual or family additional charges outside what is reimbursed through the HCS Program. (This means, the provider can pay all of the direct and indirect portions of the rate to the ISS provider if they want to or more, but they don’t have to pay more than the direct portion of the rate if they don’t want to. Many HCS/TxHmL providers choose to pay all of the rate amount, the direct and indirect side both, but most likely are not paying more than the total rate as this would not be feasible or affordable for many HCS providers.)
Question 2: According to the rules, a person may receive in-home ISS assuming certain criteria are met/justifications secured. Provision of the service does not require a license. If the person wants to also engage in off-site activities, such must be provided by a licensed ISS. In these cases,
~Can (as an example) the HH provider obtain a license for off-site only and provide the service as long as the HH provider was not the person delivering the service?
HHSC’s Response: In accordance with the HCS Billing Requirements, Section 43102.7 a host home/companion care provider is prohibited from being the service provider of in-home individualized skills and socialization. There is no prohibition on the host home/companion care provider being a service provider of on-site or off-site individualized skills and socialization but those services cannot be provided in the individual’s residence. The host home/companion care provider would need to either be employed by an individualized skills and socialization provider or obtain an individualized skills and socialization license.
~ Can the individual (again one who has a justification for in-home ISS) attend an ISS just to participate in off-site ISS only, or must that service be provided in an off-site only licensed ISS ?
HHSC’s Response: Yes, an individual who has a justification to receive in-home individualized skills and socialization may choose to also receive off-site individualized skills and socialization at a facility that provides both on-site and off-site individualized skills and socialization. It is not required that they receive off-site through an off-site only licensed individualized skills and socialization facility.
~ Can the program provider for an individual obtain an off-site only ISS license so the individual can participate in off-site ISS activities as long as the service provider of such is not the HH provider? And if so, could the person providing the in-home ISS work for or contract with the provider to provide off-site ISS to the individual?
HHSC’s Response: Yes, a program provider may become a licensed off-site only individualized skills and socialization provider so that an individual can participate in off-site individualized skills and socialization activities. The service provider providing in-home individualized skills and socialization would be allowed to become an employee or contractor of the program provider owned off-site only individualized skills and socialization provider, as long as they met all other service provider requirements outlined in program rule and in the HCS Program Billing Requirements.
Question 3: Concerning ISS notes, it’s been reported by some providers that some HHSC or TMHP reviewers have told them that the ISS notes cannot be handwritten rather must be electronic. Is that true? And if so, where is that stated?
HHSC’s Response: There is no requirement that service delivery logs for on-site, off-site, or in-home individualized skills and socialization must be electronic over handwritten. HCS Policy does not specify the modality of service delivery log notes, only that the written documentation must be legible. According to Section 3810 of the HCS Billing Requirements:
3810 General Requirements
Revision 23-2; Effective April 1, 2023
(a) Legible A program provider must have written, legible documentation to support a service claim.
January 13th, 2023
ISS FAQs: Updated January 13th, 2023
August 23rd, 2022
Frequently Asked Questions HHSC shared during the ISS draft rules webinar on August 23rd, 2022.
These are questions received during the ISS webinar on July 19th, 2022
Q1: Will current day hab providers be grandfathered into the new
program? Or do they have to be program provider to have a day hab
contract with HHSC?
A1: No, Day Hab Providers are not grandfathered into the Individualized Skills and
Socialization program. Any provider who is interested in delivering Individualized
Skills and Socialization services must obtain a Day Activity Health Services or DAHS
– Individualized Skills and Socialization service category license, even those who
are currently providing day habilitation services.
Q2: Are the off-site activities generated from the individual PDPs or does the
ISS facility plan the activities?
A2: Off-site activities are generated from the individual’s Individual Plan of Care
and Individual Program Plan in the DBMD waiver program. In TxHmL and HCS, an
Individualized Skills and Socialization provider must provide off-site Individualized
Skills and Socialization in accordance with an individual’s PDP, IPC, and
implementation plan.
Q3: If the in-home service provider does not need to be an ISS
provider, does that mean that they can be a parent?
A3: A person who meets the Service Provider Qualifications for In-Home
Individualized Skills and Socialization, including a parent of an adult child
can provide Individualized Skills and Socialization.
Q4: What is the enhanced staffing rate? How does that work?
A4: An enhanced staffing rate is available in the HCS and TxHmL Programs
for an individual who requires more service provider support than the
individual would receive with the individual’s assigned LON. The requirement
for additional support may be because of the individual’s mobility, medical,
or behavioral needs. The program provider may request the enhanced
staffing rate for an individual with an LON 1 or LON 5 in the HCS Program, or
any LON in the TxHmL Program.
Q5: If the PDP do not specify how often a client needs to go out, will that be up
to the discretion of the individualized skills organization to decide how often
they go out?
A5: It is the individual’s choice for how they choose to receive off-site Individualized
Skills and Socialization and off-site Individualized Skills and Socialization must align with
the individual’s PDP, IPC, IP, and in DBMD the individual’s IPP.
Q6: Do we need to provide meals and snacks? Have a paid nurse on site? Can it
be an LVN?
A6: An Individualized Skills and Socialization provider does not need to provide meals
and snacks to the individuals, but they must provide personal assistance for an
individual who cannot manage personal care needs including eating during an
Individualized Skills and Socialization activity. An Individualized Skills and Socialization
provider must also be able to provide assistance with medications and the performance
of tasks delegated by a registered nurse.
Q7: Is there going to be an open enrollment period for ISS with times of the year
that are closed, or is it an open enrollment?
A7• An individual in the HCS, TxHmL, and DBMD Program can add Individualized Skills
and Socialization to their IPC at any point during the plan year. It is the individual’s or
their LAR’s choice if they would like to receive individualized skills and socialization.
• Any provider who is interested in delivering Individualized Skills and Socialization
services must obtain a Day Activity Health Services or DAHS – Individualized Skills
and Socialization service category license. The provider may apply at any time once
the online licensure portal (TULIP) is operational. HHSC anticipates that the license
application process will be available late November or December.
Q8: Are staffing ratios minimum or maximum? Will providers be reimbursed if
they go over the ratio?
A8: The staffing ratios described in the rule indicate that they are “no higher than” i.e.,
they describe the maximum ratio of individuals to service providers of Individualized
Skills and Socialization. To receive reimbursement and avoid recoupment of funds,
Individualized Skills and Socialization services (on-site, off-site, or in-home) must be
provided in accordance with the HCS, TxHmL, or DBMD Program rules.
Q9: Will ISS providers be required to have RNs as part of staff now that
medication management is part of the program? Additionally, our day hab does
not currently enroll individuals that need help with toileting or feeding needs,
will the program require that we do enroll these LONs individuals?
A9: If an individual receiving Individualized Skills and Socialization needs assistance
with medication or other nursing tasks, the HCS program provider’s nurse must ensure
the Individualized Skills and Socialization service providers are delegated/trained to
deliver the service. Individualized Skills and Socialization providers like day habilitation
providers can refuse to accept a person for services.
Q10: Is there any guidance regarding scheduling? For example, is the service
only Monday-Friday, etc.
A10: There is not a requirement for how many hours per day an Individualized Skills
and Socialization provider needs to provide services. There is a service limit for the
combined total of on-site, off-site, and in-home Individualized Skills and Socialization for
HCS and TxHmL of 1560 hours during an IPC year, six hours per calendar day, and five
days per calendar week.
Q11: Does an HCS, TxHmL or DBMD provider have to apply to be licensed as ISS
provider?
A11: An active day habilitation site could choose not to participate in Individualized Skills and
Socialization and not apply for a license. They would no longer be able to provide day
habilitation to individuals in HCS, TxHmL, and DBMD after March 1, 2023, since day hab will
no longer be a service at that point. Any provider who wishes to deliver Individualized Skills
and Socialization services will be required to have a Day Activity and Health Services –
Individualized Skills and Socialization license. A provider must obtain a temporary license
prior to delivering Individualized Skills and Socialization services and may choose to do so at
any time once the licensing system is available. HHSC Long-term Care Regulatory will issue a
provider a final license after conducting an on-site visit that results in final approval of the
license.
Q12: In the examples of ratios given, there was not an example that included an ICF
client. What are the expectations when mixing ICF clients with waiver clients?
A12: If a person is not in the TxHmL, HCS, or DBMD Program and is receiving services by a
staff member who is also providing on-site Individualized Skills and Socialization to an
individual in the DBMD Program or off-site to an individual in the HCS, TxHmL, and DBMD
Program, the appropriate HCS, TxHmL, and DBMD staffing ratio must be applied, and that
individual must be included in the staffing ratio.
Q13: If someone’s PDP says they need XX hours in the community, but we do
not have the manpower, are we still able to work with the client?
A13: Waiver providers can engage the Individualized Skills and Socialization
providers in the development of the implementation plan by identifying free or low-
cost activities (affordable by the individual) the Individualized Skills and Socialization
providers can offer within their community and match well with the individual’s
interests. Off-site Individualized Skills and Socialization is provided in a community
setting chosen by the individual from among available community setting options.
Community settings are settings accessible to the general public within an
individual’s community.
Q14: Day hab allowed for 5-hour minimum days, so now under ISS is it going
to be required to be 6 direct services timer?
A14: The service limit for the combined total of on-site, off-site, and in-home
Individualized Skills and Socialization for HCS and TxHmL is:
(1) 1560 hours during an IPC year;
(2) six hours per calendar day; and
(3) five days per calendar week.
Individuals can receive less than six hours per calendar day.
Q15: If the individual/LAR choses not to utilize the ISS program, will
they still be able to receive funding from TxHmL/HCS?
A15: The individual or LAR can choose to receive in-home Individualized
Skills and Socialization if the individual meets the policy for in-home
delivery. Individuals living in three and four person residences would need
to participate in employment or day activity with natural supports if the
LAR or individual does not choose to receive individualized skills and
socialization and does not meet the policy guidance for in-home
individualized skills and socialization. Access to HCS and TxHmL waiver
services is not dependent upon receiving individualized skills and
socialization.
Q16: Can we have a combination of HCS waivers and private pay? Does private
pay also need to be in the community?
A16: Individualized Skills and Socialization providers will have a choice about how to
conduct business. They will be allowed to accept all payor sources, or they may choose
to accept only waiver (HCBS) or non-waiver. The HCBS settings regulations do not apply
to ICF/IID, private pay or general revenue and therefore, day habilitation can continue
to be provided without changing the service to individualized skills and socialization;
however, if a provider wants to serve individuals in the waiver programs, the provider
must do so as a licensed individualized skills and socialization provider after March 1,
2023. Individualized skills and socialization has both on-site and off-site services that
must be offered to individuals in the waivers.
Q17: Will ISS provided in the client’s home require EVV verification for HCS and
TxHmL funded clients? If the client lives in a group home or a Host
Home/Companion Care home, will the EVV verification be required?
A17: In-home Individualized Skills and Socialization provided in the individual’s own
home or family home will require the use of EVV verification, similar to in-home day
habilitation today. If the individual lives in a 3-person or 4-person residence, or a host
home/companion care residence, EVV verification will not be required.
Q18: Will we need a separate license for each day hab our individuals
attend including any families that provided in-home day hab due to
their LON and medical need?
A18: Each physical location that provides on and off-site Individualized Skills
and Socialization services will require its own license and application process.
In-home services will not require a license.
Q19: Can you give a few examples of offsite locations?
A19:Visits to the museums, libraries and parks are examples of off-site
Individualized Skills and Socialization activities if they are chosen by the
individual, integrate the individual into the community, and promote the
development of skills and behavior that support independence and personal
choice.
For further questions, contact:
HCSPolicy@hhs.texas.gov
TxHmLPolicy@hhs.texas.gov
LTCRPolicy@hhs.texas.gov
HHSC will conduct a public hearing on the proposed HCS, TxHmL and DBMD ISS program rules on September 7, 2022 from 8:00 am. until Noon. To register for the virtual hearing, go to: https://attendee.gotowebinar.com/register/927810115195515152
Reminder: Revalidation Period Extension Through May 31st, 2025
December 20th, 2024

TMHP Email: TMHP sent this email to keep providers up to date regarding a recently published article, which details the recent Provider Revalidation Extension that was granted by the Health and Human Services Commission (HHSC).
The fully published article can be found here: https://www.tmhp.com/news/2024-12-13-revalidation-due-dates-extended-and-retroactive-enrollment-period-be-implemented. It covers the recently granted revalidation extension, how it will affect currently applied enrollment gaps and enrollment effective dates and enrollment periods for providers, as well as general timeframes for implementation, and future claims filing and enrollment instructions. Additional publications and notifications are also in the works, and we will share these, as well, once they are publicly available.
If you have questions about the article mentioned above, and wish to contact TMHP directly for assistance, please call the TMHP Contact Center at 800-925-9126, or email provider.relations@tmhp.com.
12/02/24
Revalidation Due Date Extension and Grace Period
The Texas Health & Human Services Commission (HHSC) and the Texas Medicaid & Healthcare Partnership (TMHP) are taking actions to assist providers experiencing difficulty completing the provider enrollment revalidation process in the Provider Enrollment Management System (PEMS). The actions described in this notification are designed to provide near-term relief for providers while HHSC and TMHP pursue longer-term system and process improvements. HHSC and TMHP continue to analyze the scenarios that must be addressed with these actions and will provide additional clarification and information as needed. These flexibilities are currently planned to last through May 31, 2025.
Please read the full notice Revalidation Due Date Extension and Retroactive Enrollment Period Effective Dates | TMHP.
New Review Process regarding Critical Incident Reports
December 18th, 2024
Guidance Related to the Regional Offsite Review Process for Critical Incidents Reported into CIMS
HHSC Long-term Care Regulation published Provider Letter 2024-22, Regional Offsite Review (ROR) Process for Critical Incidents Reported into the Critical Incident Management System (CIMS), for Home and Community-based Services (HCS) and Texas Home Living (TxHmL) providers and a frequently asked questions document. Both documents are available on the HCS and TxHmL provider portals.
December 16th, 2024
Changes are coming to CIMS!
Long-Term Care Regulation staff and program providers are invited to attend the Regional Offsite Review Process for Critical Incidents Reported into the Critical Incident Management System for HCS/TxHmL training webinar.
Regional Offsite Review Process for Critical Incidents Reported into the Critical Incident Management System for HCS/TxHmL
Monday, Dec. 23
10–11 a.m.
Register for the webinar.
Deadline For Stakeholder Comments For Proposed HCS and TxHmL Billing Requirements-Dec. 16th, 2024
December 14th, 2024
Home and Community-based Services and Texas Home Living stakeholders can now comment on the proposed revisions to the HCS and TxHmL Billing Requirements by 5 p.m. on December 16.
The proposed billing requirement revisions and a summary of changes are located on the Long-term Care Providers webpage and are outlined below:
HCS
- HCS Billing Requirements Draft Revision 25-1
- HCS Billing Requirements Draft Revision 25-1 Summary of Changes (PDF)
TxHmL
HHSC Retraction To Be Posted Concerning: TMHP LMS Knowledge Management Bulletin on Surety Bond
December 13th, 2024
Subject: TMHP LMS Knowledge Management Bulletin
Here is what the message sent out stated:
“You have been enrolled and must complete KMB OCM 8383761 Surety Bond PDC60 Batch Process Removal 12/13/2024.”
Course Instructions:
1. Open a Microsoft Edge browser and log into the Learning Management System at https://learn.tmhp.com/.
2. Click the Plan icon in the navigation bar to view the training.
3. Select KMB OCM 8383761 Surety Bond PDC60 Batch Process Removal 12/13/2024 and complete the training.
Employment Assistance & Supported Employment Training Options From HHSC
Employment Assistance & Supported Employment Training Options From HHSC
December 10th, 2024
The Texas Health and Human Services Commission (HHSC) is pleased to host a free in-person Employment First / Employment Services training on January 28, 2025, at the Starlight Event Center – Trans Mountain Room, 6650 Continental Drive, El Paso, Texas 79925.
Training will be one day in duration and is scheduled for 9 a.m. to 4 p.m, MST.
Training topics will cover:
- Overview of Employment First and the National movement with Employment First.
- Providing Employment Services
- Family Concerns and Disability Inclusive Communities
- Employment Readiness Skills
- Apprenticeship Programs
- Employer Relationships
This training is valuable to anyone who has a role either indirectly or directly in promoting employment services and helping individuals achieve their goal of competitive and integrated employment.
November 11th, 2024
The Texas Health and Human Services Commission (HHSC) is pleased to host a free in-person Employment First / Employment Services training on December 2, 2024 at the HHSC North Austin Complex (NAC), 4601 W. Guadalupe Street, Austin, Texas 78751, Rooms 1.401–1.404.
Training will be one day in duration and is scheduled for 9 a.m. to 4 p.m, CST.
Training topics will cover:
- Overview of Employment First and the National movement with Employment First.
- Providing Employment Services
- Family Concerns and Disability Inclusive Communities
- Employment Readiness Skills
- Apprenticeship Programs
- Employer Relationships
This training is valuable to anyone who has a role either indirectly or directly in promoting employment services and helping individuals achieve their goal of competitive and integrated employment.
June 28th, 2021
There were 2 Home and Community-based Services and Texas Home Living trainings in this series:
The web-based trainings cover employment services provided through HCS and TxHmL, information about the payer of first resort for employment assistance, and the basics of providing these services. They are designed to enhance staff knowledge about providing quality employment services to people enrolled in the waivers.
Each training has a corresponding quiz.
The Direct Service Workers web-based training provides information about employment services and how direct service workers can support people achieve their employment goals. The training covers federal and state initiatives related to employment for people with disabilities and touches on issues related to people who work and receive SSI or SSDI benefits. The training has a corresponding quiz.
Star Plus Handbook Update
December 5th, 2024
The STAR+PLUS Handbook updates Appendix XXII. This revision is effective Dec. 1, 2024.
Provider Investigations Handbook (PIH) Revised
December 3rd, 2024
The Provider Investigations Handbook (PIH) revision 24-2 updates sections throughout the handbook. This revision is effective Dec. 2, 2024. Does apply to HCS/TxHmL/ICF programs.
“Embracing Change To Enhance Value”-2024 Conference for ICF Surveyors and Providers- Dec. 5th, 2025
December 1st, 2024
Register for the 2024 ICF Conference Webinar
The Intermediate Care Facility Conference webinar for Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) program staff and providers will be held on Tuesday, Dec. 5. There is one track, so register for each session for the complete educational activity.
Welcome to the 2024 ICF Conference: Embracing Change to Enhance Value
8:30–8:45 a.m.
Register for Webinar
Keynote: Scott Abel, “The Strive to Thrive”
9–9:45 a.m.
Register for Webinar
ICF Deficiency Trends
10:15–11:45 a.m.
Register for Webinar
Understanding Survey Rules: What Surveyors Look for During an ICF/IID Survey
1–2:30 p.m.
Register for Webinar
Surrogate Decision Making
3–4:15 p.m.
Register for Webinar
Comments on Proposed Rule Changes for HCS & TxHmL Have Ended
November 28th, 2024
The informal comment period for new proposed changes to the rule for HCS & TxHmL (TAC 565 and 566) ended on November 27, 2024: Comment on Proposed & Draft Rules | Texas Health and Human Services.
These proposed new and amended rules implement House Bill (HB) 1009 by Turner the 88th Legislature, Regular Session, 2023. HB 1009 imposes a new requirement on a Medicaid provider providing services under a 1915(c) waiver to conduct criminal history record information and employee misconduct registry reviews and to suspend the employment or contracts of individuals who engage in reportable conduct. New rule language in §565.12 requires HCS providers to notify HHSC of opening a new location or the voluntary closure of an HCS residence. Added language under §565.15 prohibits minor children from sharing a bedroom with an adult in HCS residences, including host/home and companion care settings. Added language under §565.23 clarifies the authority of LTCR.
The TxHmL Handbook Revision 24-1
November 26th, 2024
The TxHmL Handbook Has Been Revised
Texas Home Living (TxHmL) Program handbook revision 24-1 updates Appendix X.
This revision became effective Oct. 1, 2024. Click this link to see the updates.
Adverse Childhood Experiences (ACES) and Trauma Informed Care (TIC) Conference Online-12/05/24
November 16th, 2024
From HHSC Weekly Digest Bulletin:
Adverse Childhood Experiences (ACES) and Trauma Informed Care (TIC) Conference Online, December 5, 2024
|
|
|
|
Six (6) hours of FREE continuing education units (CEUs) will be provided by HHSC. See registration for details.
ASL and CART will be provided.
Presentations will include:
- “Recognizing and Responding to Adversity: Embracing Trauma-Informed Care in Intellectual and Developmental Disability Services” by John Keesler, Ph.D., MSW, LMSW Associate professor, School of Social Work, Indiana University Bloomington
- “The Road to Recovery: Supporting Children with Intellectual and Developmental Disabilities Who Have Experienced Trauma” by Laura Buckner, Community Education, Texas Center for Disability Studies, UT Austin; Mentor trainer, The Learning Community for Person-Centered Practices
- “Trauma and Healing in the Lives of People with Intellectual and Developmental Disabilities” by Karyn Harvey, Ph.D., Psychologist, author, and director of programs for the Park Avenue Group; and
- “Addressing the Impact of Adverse Childhood Experiences in Children with Intellectual and Developmental Disabilities” by Kynthia Brooks, Child Health Specialist, Family Health Strategy division, Texas Health and Human Services Commission
 |
TMHP: Important Reminder Concerning Client Movement Forms
November 15th, 2024
Submitting HCS and TxHmL Individual Movement Forms
Home and Community-Based Services Waiver (HCS) and Texas Home Living Waiver (TxHmL) providers should refrain from submitting the following Individual Movement Forms (IMTs) via the Long-Term Care (LTC) Online Portal:
• IMT-Local Authority Reassignment
• IMT-Service Coordinator Update
These specific purpose codes are designated for LIDDA-use only and should not be submitted by HCS and TxHmL providers for any reason!
HCS and TxHmL providers can only submit the IMT for purpose codes “IMT-Suspension” and “IMT-Individual Update.” See page 193 in the LTC HCS and TxHmL Waiver Programs Provider User Guide for details.
**Questions For issues encountered while submitting the IMT on the TMHP LTC Online Portal, call TMHP at 800-626-4117, select option 1, then option 1.
Webinars & CBT’s Available For LTC Providers (HCS/TxHmL) on TMHP Learning Management System
November 15th, 2024
Computer-Based Training in the TMHP Learning Management System
The following long-term care (LTC)-specific computer-based training (CBT) course is currently available on the Texas Medicaid & Healthcare Partnership (TMHP) Learning Management System (LMS):
• LTC Online Portal Basics—This interactive CBT provides a basic overview of the LTC Online Portal, including information about creating an administrator account and an overview of the features of 5 November 2024 LTC Provider Bulletin, No. 100 Training and Events the blue navigational bar and the yellow Form Actions bar. Demonstrations and simulations appear throughout the CBT to provide opportunities for an interactive experience.
• TexMedConnect for Long-Term Care (LTC) Providers—This CBT demonstrates effective navigation and use of the LTC TexMedConnect web application.
Providers will learn how to:
‒ Log in to TexMedConnect
.‒ Verify a client’s eligibility
.‒ Enter, save, and adjust different types of claims
.‒ Export Claim Data.
‒ Find the status of a claim
.‒ View Remittance and Status (R&S) Reports.
LTC Online Portal Training for HCS and TxHmL Waiver Programs Webinar – Provides information on the features and navigation of the LTC Online Portal, management of waiver program assessments and forms in the LTC Online Portal, and the purpose and workflow of the forms. For a list of webinar or CBT descriptions, upcoming broadcast dates, registration links, recordings of past webinars, and Q&A documents, visit the TMHP Learning Management System (LMS) at learn. tmhp.com.
The TMHP LMS can be accessed through the TMHP website or directly at learn.tmhp.com.
Providers must create an account to access the training materials on the LMS. To create an account, click Don’t have an account? Sign up here on the LMS home page. For questions about the LTC training CBTs and webinars, call the TMHP Contact Center at 800-626-4117 or 800-727-5436. For LMS login or access issues, email TMHP LMS support at TMHPTrainingSupport@ tmhp.com.
IPC Revisions to Add ISS/Renewal & IPC Revisions/Enrollment & Transfer IPC’s
November 12th, 2024
Reminder for HCS and TxHmL Providers Entering IPC Revisions to Add Individual Skills and Socialization
This is a reminder for Home and Community-based Services (HCS), Texas Home Living (TxHmL) program providers, and local intellectual and developmental disability authorities (LIDDAs) that are submitting an Individual Plan of Care (IPC) revision to add Individualized Skills and Socialization (ISS) on the IPC plan year.
When entering IPC revisions, if you update the effective date in field 12a, you must click the search icon located next to the date field. This will allow the individual’s data to refresh and prepopulate from the web service based on the new effective date.
If you don’t perform this step, the form processing will be delayed. Contact the Texas Medicaid & Healthcare Partnership (TMHP) Long-Term Care (LTC) Help Desk at 800-626-4117 or 800-727-5436 for assistance with submitting forms.
Renewal and Revision IPCs
If they are in either Pending DADS Review or Pending Coach Review status require action from the submitter, usually the submission of supporting documentation. The IPC will not be reviewed until action is taken. This is the same process that is in place for Exceeds flags in ID-CARE.
A packet submitted to Utilization Review (UR) must include the following:
• IPC Cover Sheet (Form 8599, which can be found at hhs.texas.gov/regulations/forms/8000-8999/ form-8599-individual-plan-care-ipc-cover-sheet)
• Copy of signed IPC (all pages)
• Person-directed Plan
• Implementation Plans for all services on the IPC, including a breakdown of nursing and behavior hours if they are part of the request A packet may include the following, depending on the services that are requested: • Comprehensive Nursing Assessment (Form 8584 or a form with all the same elements) for nursing hours
• Occupational therapy (OT) evaluation, treatment plan, or assessment (including orders) for OT hours
• Physical therapy (PT) evaluation, treatment plan, or assessment (including orders) for PT hours
• Speech and language therapy evaluation, plan, or assessment (including orders) for speech hours
• Dietary evaluation for dietary hours (including orders)
• Dental treatment plan, if applicable
• Behavior support plan for behavioral support hours that meets HHSC criteria
• PAS/HAB Assessment (Form 8510) for personal assistance services and habilitation (PAS/HAB) hours
• Transportation Plan (Form 3598) for transportation hours
• Audiology treatment plan (including orders), if applicable
• Cognitive rehabilitation therapy plan, if applicable (in HCS)
• Support consultation plan, if applicable (in HCS) • Social work plan, if applicable (in HCS)
• All documentation for adaptive aids, if they are included in the request, including:
‒ A list of items to be purchased, the number of each item needed, and the cost (based on the lowest bid) for each item.
‒ Three bids for each item. Bids from online vendors are acceptable. If an annual vendor is used, three bids are needed only if an item costs $500 per month or more; otherwise, an annual vendor bid can be submitted.
‒ Proof of Medicaid denial and professional recommendations, as required in Appendix VII of the HCS Program Billing Requirements.
See Section 6100 of the HCS Billing Requirements at hhs.texas.gov/sites/default/files/documents/ doing-business-with-hhs/provider-portal/long-term-care/hcs-billing-requirements.pdf for more information.
• All documentation for minor home modifications (three bids based on specs from licensed professional recommendations) if they are part of the request.
See Section 6200 of the HCS Billing Requirements.
Enrollment and Transfer IPCs
Enrollment and transfer IPCs remain in Pending DADS Review status while the enrollment or transfer is being processed.
Enrollment IPCs may require additional documentation to be submitted to Program Eligibility and Support (PES).
*If an enrollment requires additional documentation, PES will contact the LIDDA that submitted the enrollment IPC.
Transfer IPCs always require a transfer packet to be submitted to PES. If a transfer packet requires additional documentation, PES will contact the LIDDA that submitted the transfer IPC.
A transfer packet submitted to PES must include the following
: • Request for Transfer of Waiver Program Services (Form 3617)
• HCS only: Individual Plan of Care – HCS/CFC (Form 3608)
• TxHmL only: Individual Plan of Care – TxHmL/CFC (Form 8582)
If an enrollment or transfer requires utilization review, UR will contact the LIDDA that submitted the enrollment or transfer packet.
Packet and Documentation Submission Details
The most efficient way to submit HCS and TxHmL documentation is through the Attachment function in the Long-term Care Online Portal (LTCOP). For more details on attachments, refer to the “LTC Online Portal to Allow Electronic Attachments on HCS and TxHmL Waiver Program Forms” notification posted on tmhp.com on June 28, 2023.
For questions about renewal, revision, or requested call back of IPC review packets, call HHSC UR at 512-438-5055, or email deskURLONIPC@hhs.texas.gov. For questions about enrollments or transfers, call PES at 512-438-2484, or email enrollmenttransferdischargeinfo@hhs.texas.gov.
Assistance With Eligibility Issues Due To The End of Continuous Medicaid Coverage
November 5th, 2024

From the October 28 Ambassador Program call. Presentation slides are also included below and resource links are below.
Actions You Can Take Now
- Visit the Ambassador Toolkit page on the HHS website.
- Visit the End of Continuous Medicaid Coverage page on the HHS website.
- If you know someone who could benefit from joining the Ambassador Program, invite them to sign up using this link: Ambassador Program Signup.
We Value Your Feedback
To help us improve the Ambassador Program and ensure it meets your needs, please take a moment to complete our brief survey: Ambassador Program Feedback Survey. Your insights are invaluable to us!
Next Ambassador Program Call
Ambassador Program calls are held once a month. The next call will be on November 18th at 3:00 Central Time. If you have any questions or concerns, please feel free to reach out to this mailbox: update@hhs.texas.gov.
October 1st, 2024

Resources:
Actions You Can Take Now
1. Download Ambassador Toolkit
2. Visit End of Continuous Medicaid Coverage
3. Email Stakeholder Engagement with questions at:
update@hhs.texas.gov
4. Join the Ambassador Program –Ambassador
Program Contact List
5. Explore the Interview Toolkit: Questions About Your
Benefits | Texas Health and Human Services
6. Explore the Extended Postpartum Coverage Toolkit
https://www.hhs.texas.gov/services/health/women-
children
June 15th, 2024
HHSC stated that If people are not able to obtain assistance from the community partners or 211, they can contact the Office of the Ombudsman 877-787-8999 or complete our online form . More information on the initiative can be found at: https://www.hhs.texas.gov/providers/medicaid-business-resources/end-continuous-medicaid-coverage-ambassador-toolkit
Save the Date: Annual Intermediate Care Facility Conference Webinar Dec. 5
October 30th, 2024
The HHSC Joint Training unit will host its annual Intermediate Care Facility Conference webinar, “Embracing Change to Enhance Value,” on Dec. 5.
This daylong virtual conference is for providers and survey staff of intermediate care facilities for people with intellectual disabilities or related conditions.
Registration for sessions begins Nov. 1. Links will be provided when registration opens.
Don’t Forget Annual Vendor Submission Due (Nov.1st-Jan31st) HCS/TxHmL!
October 25th, 2024
HCS and TxHmL Annual Vendor Submission Timeframe
The timeframe to submit for annual vendor approval is Nov.1, 2024 through Jan. 31, 2025. Required documentation for annual vendor requests are in the HCS and TxHmL Billing Guidelines, Section 6160(b)(2), Approval of Annual Vendor. Email packet submissions to Billing and Payment with the subject line: Annual Vendor Approval. Submissions sent to any other email addresses may not be received.
Required documentation for annual vendor requests are in the HCS (PDF) and TxHmL (PDF) Billing Requirements, Section 6160(b)(2), Approval of Annual Vendor.
Email packet submissions to providerfiscalcompliance@hhs.texas.gov with the subject line: Annual Vendor Approval. Submissions sent to any other email addresses may not be received.
If you are unable to meet the deadline to submit, you may request an extension prior to Jan. 31, 2025. Email Provider Fiscal Compliance with any questions. Call 512-438-5359 with your questions.
Submissions sent to any other email addresses may not be received.
Don’t Forget To Get Ready For Flu Season!
October 20th, 2024

From HHSC:
LTC Providers Encouraged to Get Ready for Flu Season
CDC recommends everyone (six months and older) be vaccinated against the flu by the end of October to avoid peak flu season. Long-term care providers should review their program requirements for guidance related to vaccinations and infection control.
Some of the CDC’s recommendations for vaccinating residents in congregate health care settings are:
- The CDC recommends that LTC facilities offer the flu vaccine to all residents and health care staff throughout the flu season.
- People 65 years and older are at higher risk of developing serious flu complications compared with young, healthy adults.
- CDC and ACIP preferentially recommend the use of higher-dose flu vaccines for people 65 years and older.
Adhere to standard precautions. They’re the foundation for preventing the transmission of infectious agents in all health care settings.
Implement droplet precautions for those with suspected or confirmed flu. Do this for seven days after illness onset or until 24 hours after the fever and respiratory symptoms resolve, whichever is longer, while the person is in a long-term care facility.
In compliance with TAC Title 25, Part 1, Chapter 97, report all outbreaks to the local health department, regardless of the provider type. Contact information for your local health department is on the DSHS website.
As a reminder, flu vaccines may be safely coadministered with other vaccines. In addition to getting a flu shot, people 65 years and older should take the same everyday preventive actions CDC recommends for everyone, including avoiding people who are sick, covering coughs, washing hands often, and staying up-to-date with all recommended vaccines.
For more information, visit the following links:
Time To Vote: Ensure Your Individuals Are Educated and Have The Opportunity To Vote
October 17th, 2024
Please be sure to provide education about voting, if needed as well as opportunities for your individuals to vote. Twogether Consulting recommends checking out the “My Voter Portal” at the Secretary of State’s website before voting to look for your voting location and to ensure an individual is still registered, as the individual may not be registered anymore if they have moved for example. FYI, the voter registration deadline ended on Oct. 7th, 2024. Information on services for voting available to persons with disabilities can be found at: https://www.votetexas.gov/mobile/voter-with-special-needs.htm
Here is the information on dates for absentee and general voting deadlines
Absentee ballot deadlines
- Request ballot (received by) : Oct 25
- Return ballot by mail (postmarked by) : Nov 5 by 7:00 p.m. CST
- Return ballot in person : Nov 5 by 7:00 p.m. CST
Important Action You Can Take With Your Individuals
- Make a voting plan with this guide for voters with disabilities from Disability Rights Texas.
- Watch this video for voters with disabilities and poll workers from Texas Council for Developmental Disabilities.
- Vote early Oct. 21-Nov. 1!
- If voting by mail, the deadline to apply for a mail-in ballot is Oct. 25.
If you need assistance in registering to vote, have questions regarding voting or feel that any of your voting rights have been violated, please contact:
Disability Rights Texas
2222 West Braker Lane
Austin, Texas 78758
1-888-796-VOTE (8683)
vote@drtx.org
Texas Secretary of State
P.O. Box 12060
Austin, Texas 78711-2060
512-463-5650 or 1-800-252-VOTE (8683)
Fax: 512-475-2811; TTY: 7-1-1
Texas Secretary of State website
HHSC Moves News and Information and Provider Letter Content
October 16, 2024
Effective Oct. 16, HHSC moved the News and Information and the Provider Letter content to new locations on the Long-Term Care Regulation (LTCR) Provider webpages.
This change to the LTCR Provider webpages was made to improve the visibility of the content and to fix a technical issue that wouldn’t let people use the search feature of the Provider Letter content more than once.
News and Information and Provider Letters now have separate links accessible from the main webpage for each provider type. These links are found on the left-hand menu of each provide page along with the links for how to become a provider.
All providers listed here are affected by the updated web links.
Annual EVV Policy Training Webinars for CDS Employers
October 13th, 2024
This is a reminder that HHSC will host Electronic Visit Verification training webinars for Consumer Directed Services (CDS) employers required to use EVV. Attending the webinar will complete the annual EVV policy training requirement.
Webinar Registration
Agendas are included in the registration link.
Alternatively, CDS employers can also complete the annual EVV policy training requirement on the HHS Learning Portal.
The EVV Required Training Checklists (PDF) will help track completed EVV trainings.
Advocacy Resources For Individuals with Intellectual and Developmental Disabilities
Resources for IDD Providers: Organizations & Associations
October 13th, 2024
National Organizations:
American Association on Intellectual and Developmental Disabilities (AAIDD)
American Network of Community Options & Resources (ANCOR)
National Association of Qualified Developmental Disability Professionals
National Parent Network on Disabilities (NPND)
The Accreditation Council
State Associations:
Private Providers Association of Texas (PPAT)
Providers Alliance for Community Services of Texas (PACSTX)
Office of Inspector General (OIG) Recommends Updating ER/Evac Plans
October 12th, 2024
From OIG: Update emergency plans
Providers should take stock of emergency preparations, acknowledging that a disaster is best prepared for well ahead of time. In Texas, long-term care facilities, including assisted living, nursing and intermediate care facilities, hospices and group homes, are responsible for maintaining emergency response plans for the residents in their care.
To verify that providers comply with federal and state requirements, OIG inspectors can review these facilities’ response plans, equipment and staff training. Most facilities were prepared during the most recent inspections, but inspectors found a few common errors. Specifically:
- Not documenting initial employee training on emergency preparedness.
- Not ensuring the emergency preparedness plan identifies how alternate energy sources should be used to maintain the power needs of key systems.
- Failing to maintain a printed copy of the current emergency preparedness plan at each workstation assigned to a personnel supervisor who had responsibilities under the plan.
- Failing to document the required contact information for the state licensing and certification agency in its communication plan.
- Not sharing the emergency preparedness and response plan with residents and residents’ legally authorized representatives.
- Failing to request an annual fire marshal inspection.
Emergency preparedness is vital for care facility residents’ ongoing health and safety during local incidents, like power outages or widespread natural disasters. Providers can find helpful preparedness resources at the DSHS Texas Ready website, including sample plans, disaster supply checklists and more information on preparing for hurricanes and other emergencies.
Preparing for a disaster includes planning for evacuation, transportation, communication, staff responsibilities and continuing resident care and treatment. In an emergency, providers can visit Texas HHS Disaster Services for up-to-date regulatory support for health care facilities, long-term care facilities and special waivers for Medicaid providers and clients as needed.
Tarrytown Expo Pharmacy Zoom Webinar October 10th, 2024
October 9th, 2024
Tarrytown Expo Pharmacy Zoom Webinar (Complimentary CE Credits)

Click here for the printable PDF version
EVV Policy Training Webinars For Program Providers, FMSA’s & CDS Employers: Sept.-Oct. 2024
September 14th, 2024
** This is especially important for all of you new HCS/TxHmL Providers.
Registration Available for HHSC EVV Policy Training Webinars for Program Providers, FMSAs and CDS Employers
HHSC is hosting Electronic Visit Verification (EVV) policy training webinars for program providers and financial management services agencies (FMSAs), and Consumer Directed Services (CDS) employers. You will complete the annual EVV policy training requirement by attending one of the webinars.
Webinar Registration
Agendas are included in the registration links. Select from the dates below to register for one webinar.
- Annual EVV Policy Training in September for Program Providers and FMSAs:
- Annual EVV Policy Training in October for CDS Employers:
Alternatively, program providers, FMSAs and CDS employers can also complete the annual EVV policy training requirement on the HHS Learning Portal.
The EVV Required Training Checklists (PDF) will help track completed EVV trainings.
Register for EVV GovDelivery to receive EVV notices by email, such as training updates and future webinar registrations.
Email questions to HHSC EVV Operations.
FREE Positive Behavior Management and Support 2024 (PBMS) Virtual Workshop
September 13th, 2024
The Texas Health and Human Services Commission (HHSC) is offering virtual Positive Behavior Management and Support (PBMS) and Advanced PBMS workshops at no cost for attendees on the following and times:
- September 23 (PBMS)
- October 9 (PBMS)
- October 25 (Advanced PBMS)
- November 8 (Advanced PBMS)
**Please click on a date above to register for that workshop.
The workshops are available to the public, including family members, caregivers, providers (educational, foster care, geriatric, long-term services and supports in the intellectual and developmental disabilities and aging population, and mental health), Adult Protective Services, and case managers.
Upon completion of the training, HHSC will issue continuing education units (CEUs) for social workers, certified nurse aides, licensed nursing facility administrators, nursing facility activity directors, assisted living facility managers, day activity and health services managers, qualified developmental disabilities professionals, and qualified intellectual disabilities professionals. Behavior analyst certification board CEU will be issued by the University of North Texas.
For training resources, visit the Training Initiatives webpage.
STAR+PLUS Transition Member Information: Change In MCO Providers
September 11th, 2024
Effective September 1, HHSC began transitioning contracts for the STAR+PLUS program.
This document below provides STAR+PLUS members and providers with resources for assistance with go-live concerns.
STAR+PLUS Providers by service area (MCO’s leaving, staying and new)
|
I am a… |
I need help with… |
How to get help |
|
Member |
Learning general information about the transition |
See the HHSC STAR+PLUS webpage |
|
Member |
A complaint about my MCO |
Contact your MCO plan first. If the issue isn’t resolved, contact the HHSC Ombudsman |
|
Member |
STAR/CHIP, STAR Health, STAR Kids, MMP, or CHIP |
Please see the HHSC Medicaid and CHIP webpage |
|
Member |
Understanding how my coverage may be impacted by the transition |
Please see the Continuity of Care webpage |
|
Provider |
Contracting with an MCO |
To contract with an MCO, please see the MCO provider contacts list. If you have already connected with an MCO and have a complaint, reach out to the Health Plan Management Complaints inbox. |
|
Provider |
Understanding how the transition pay impact my billing |
Please reach out to the MCO you have contracted with to understand their billing processes |
|
Provider |
Understanding how to help my clients through the transition |
Please see the HHSC STAR+PLUS webpage for transition resources |
For any STAR+PLUS transition related issues, please contact the STAR+PLUS Go Live inbox.
May 12th, 2024
- Nine (9) of the 13 service areas were affected by the procurement and award processes:
- Letters from HHSC have been sent to current members in the nine (9) areas in which a change in MCOs is occurring. The letters were sent In March.
- Members in the 9 affected service areas have until July 20, 2024 to pick a new health plan (MCO) and will be sent a reminder before the deadline. Note: Persons satisfied with their current MCO are not required to respond to the letter, but, if they want, may switch to the new MCO or any other MCO in their area. Of course, persons currently enrolled in a MCO which was not awarded a ‘new’ contract will need to select a health plan from the MCOs in their service area.
- Example: If a person resides in the Jefferson STAR+PLUS Service Area, and is currently enrolled with United Healthcare, the person will need to choose either Wellpoint or Molina since , effective September 1, 2024, United Healthcare will no longer serve that area. On the other hand, if a person residing in Jefferson STAR+PLUS service area is currently enrolled with Molina, the person can either stay with Molina, or change to the other MCO (Wellpoint) in that area.
- HHSC is planning to conduct information sessions about the changes, but no dates were provided.
TxHmL New Rates: September 1st, 2024
September 10th, 2024
TxHmL New Rates
Click on link below:
TxHmL Rates: Sept. 1st, 2024- PDF Download
The Texas Health and Human Services Commission (HHSC) approved payment rates for Support Consultation under Community Attendant Services (CAS), the Community Living Assistance and Support Services (CLASS) waiver program, the Deaf Blind with Multiple Disabilities (DBMD) waiver program, Family Care (FC), the Home and Community-based Services (HCS) waiver program, Primary Home Care (PHC), and Texas Home Living (TxHmL) to be effective Sept. 1, 2024.
HHSC reviewed Support Consultation payment rates and methodology as part of the fiscal year 2024 biennial fee review.
The approved Support Consultation payment rates, effective Sept. 1, 2024, can be accessed at: https://pfd.hhs.texas.gov/long-term-services-supports
Contact PFD-LTSS@hhs.texas.gov or (737) 867-7817 if you have questions
STATUS OF HCS RATES!
Payment Rates as of September 1st, 2024
HCS Rates Sept. 1, 2024 including ISS
Status of HCS Rates as of Jan. 1st, 2023 (includes new ISS rates)
HCS Rates Jan. 1st, 2023 including ISS services
Status of HCS Rates as of June 3rd 2022
Provider Rate Updates for HCS and TxHmL Providers
In early May, HHSC identified missing or incorrect rate keys for some Home and Community-based Services and Texas Home Living providers.
On May 11–12, HHSC completed updates to rate keys for these HCS and TxHmL providers based on rates published on the Provider Finance website.
After confirming rates with Provider Finance and paid claims on the R&S Report, contact the TMHP LTC Help Desk at 800-626-4117, Option 1, then Option 7, if you have additional questions.
https://pfd.hhs.texas.gov/sites/rad/files/documents/long-term-svcs/2022/2022-hcs-awards.pdf
Status of HCS Rates as of January 17th, 2022
HCS and TxHmL Day Habilitation Rates, Respite Rates and Other Concerns
- The Public Health Emergency (PHE) was renewed until April 16, 2022, and
- Clarification: The HCS & TxHmL rates posted on HHSC’s webpage listed as Effective March 1, 2022 to Current. are a bit confusing
Please contact the Rate Analysis Department’s Customer Information Center at (512) 424-6637 or by email at RAD-LTSS@hhsc.state.tx.us should you have any questions regarding the information in this document.
Free Webinar Session “Addressing the Recovery Support Needs of Persons with IDD”
September 3rd, 2024
Upcoming Free Webinar Session
“Addressing the Recovery Support Needs of Persons with IDD”
Hosted By Austin Integral Care and presented by Jordan Smelley, MHPS
Presenter: Jordan Smelley, MHPS

I wanted to share this wonderful resource for providers. I just received some awesome information that Austin Integral Care is hosting this webinar for providers and others working with persons with IDD. Jordan Smelley is an amazing young man and I recently had the pleasure of speaking with him and also meeting him at last year’s Texas Chapter AAIDD conference (where we were both recipients of awards).
recovery from Intellectual and Developmental Differences including Sensory Processing Disorders with Co-occurring Mental Health challenges. Jordan defines his own recovery in relation to the opportunities available to present and educate the community on topics around supporting individuals with IDD.
Jordan is also the 2023 recipient of the American Association of Intellectual and Developmental Disabilities (AAIDD) Texas Chapter Empowerment Award for Excellence in Promotion of Self-Advocacy.
Duration: 90 minutes For Presentation plus Q&A
2. Identify different potential support needs of people with Intellectual and Developmental
Disabilities including vital support needs around Sensory Processing Disorders like Tactile Dysfunction
and Proprioceptive Dysfunction
3. Execute a more trauma informed and person-centered approach to interacting with persons
with Proprioceptive Dysfunction and/or Tactile Dysfunction
Identify the intended audience of this session.
a. Behavioral health providers (MSW, PhD, LPC, other)
d. Medical Providers (MD, RN, NP, PA)
c. People with Intellectual and Developmental Disabilities
d. Caregivers/Family members of people with Intellectual and Developmental Disabilities