Twogether Updates
Letter To Providers From Twogether Consulting: December 31st, 2025
December 31st, 2025

From Twogether Consulting
Happy New Year!
I hope everyone enjoyed a wonderful holiday season. Twogether Consulting will be closed January 6th- January 15th, 2025, as I will not be in the office. Feel free to contact Meghan Jones to make an appointment with us after January 15th, 2026, by emailing her at: meghanjones.tx@gmail.com
We are not accepting any new clients for HCS, TxHml, until January 16th. We do still have our other contractors available during this time for those of you who are current customers and have an emergency or are currently working with us on a project. Sheila Hanson (HCS/TxHmL), Marcus Denman(HCS/TxHmL), and Jo Beth Collier (ICF only) will all still be available during this time for things like 1-1 webinars, mentoring or consultation, assistance with POC’s (Plans of Correction), and other emergencies, of course.
We will be checking email, and you can contact us at our general email at: info@twogetherconsulting.com or my regular email address for those of you who already have it.

January 2026 Training:
If any of you need QIDP training in the ICF program, we do have some sessions scheduled for Jan 13th, 16th, 20th, and 23rd. You may contact Meghan Jones at meghanjones.tx@gmail.com to register or info@twogetherconsulting.com for information.
Jan 13th, 2026: Roles & Responsibilities of The QIDP in ICF-Part I (Active Treatment, Admission, 30-day staffing, Annual Staffing, Interim Staffings, Discharges, and Other Important Documentation) 3 PM-5 PM
Jan 16th, 2026: Roles & Responsibilities of the QIDP in ICF-Part II (Important W-Tags) 2 PM-4 PM
Jan 20th, 2026– Rights, Rights Restrictions, and Human Rights Committee (3 PM-5 PM)
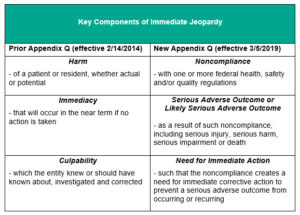
Jan 23rd, 2026– Surrogate Decision Maker/Making Committee and Immediate Jeopardy/IJ’s (2 PM-4 PM)
Please contact Meghan Jones at: meghanjones.tx@gmail.com. The cost is $65/person. We can provide the handouts as well as a link to the recording, once you have paid. Please notify Meghan Jones, for payment and to receive the link to registration for the training on “Gotowebinar” and all handouts will be provided prior to the session.
We are still available for facility and 1 on 1 requests for webinars and live training in January, but we will be taking a break from the live on-site trainings, through January 20th, 2025. We will, however, be having webinars in January. Remember, for all scheduled webinars and our general live sessions open to the public, you can view all calendar postings on our Twogether Consulting website.
Here are the webinars for January. Others may be posted in the near future
ISS: TAC Changes: Updates, Clarifications, & Survey Expectations – moved to January 28th (10am-12:00pm)
Host Home/Companion Care Service Provider: Job Description– moved to January 19th, 2026 (10am-noon)
Please continue to check our website for these sessions. We will post them on the website “calendar” page
We have a variety of pre-recorded webinar trainings for program managers, case managers and nurses, and direct care, so feel free to email us at info@twogetherconsulting.com to inquire. Let us know what areas of training you would like, to help us plan future sessions.
Here are just a few of the recent pre-recorded webinar trainings available for purchase: “Admission, Post-Admission & Other Follow-Up Requirements-HCS Program”, ICAPs/LON’s/IDRC’s-ICF Program” (Also have for HCS program), “Development of The Comprehensive Nursing Assessment & Nursing Service Plan-HCS or ICF”, “Best Practices For HCS Providers: How To Remain In Compliance With TAC Ch 565”, “Role & Responsbilities of The Q”, “Surrogate Decision Making Process, Rights Restrictions & Immediate Jeopardy-ICF Program”, “Licensed ISS Providers: What You Really Need To Know.”, We also have a ore-recorded 5 part Care Coordination/Case Management series as well for the HCS program. All of these sessions and many more come with handouts as well as the link to the pre-recorded session
Please see our “Updates” section of the website for the latest news for IDD providers.

IPC Renewals Submissions, Transfers, How To Submit IPC into LTCOP
December 31st, 2025
Now Effective: LTCOP HCS and TxHmL Transfer Form Submission Sequencing Enhancements
On December 18, 2025, the Texas Medicaid & Healthcare Partnership (TMHP) released enhancements to the Long-Term Care Online Portal (LTCOP) that are designed to streamline the transfer process for the Home and Community-based Services (HCS) and Texas Home Living (TxHmL) waiver programs. These updates are now in effect for use by providers and local intellectual and developmental disability authorities (LIDDAs).
- A TMHP enhancement for HCS and TxHmL is scheduled to deploy 12/18:
- When a transfer includes a change in residence address or county, the receiving provider will no longer need to submit a separate IMT individual update – the system will auto-generate the required update.
- LIDDA users will only see counties in their catchment area, reducing data entry errors.
- If a location code is inactive, the system will flag it.
A future enhancement will apply the same logic to revision IPCs when only the residential type changes (same contract number), so a separate individual update form will not be required in those
For more information, see the full posting at TMHP.com Now Effective: LTCOP HCS and TxHmL Transfer Form Submission Sequencing Enhancements | TMHP
December 14th, 2025
LTCOP HCS and TxHmL Transfer Form Submission Sequencing Enhancements
On Dec. 18, 2025, the Texas Medicaid & Healthcare Partnership (TMHP) will update the Long-Term Care Online Portal (LTCOP) to improve form sequencing requirements and transfer processing for the HCS & TxHmL programs. These updates will help HCS and TxHmL waiver program providers and local intellectual and developmental disability authorities (LIDDAs) to submit forms accurately and reduce manual processing needs.
Hopefully, this should make transfers occur in a much more timely fashion with fewer errors in the transfer process and accountability for transfer steps by appropriate parties.
For more information, see the full posting at TMHP.com
Coming Soon: LTCOP HCS and TxHmL Transfer Form Submission Sequencing Enhancements | TMHP
Timely Submission of IPC Renewals
HHSC reminds HCS and TxHmL providers and local intellectual and developmental disability authorities (LIDDAs) to submit individual plan of care (IPC) renewals for individuals enrolled in the HCS and TxHmL waiver programs as early as program rules allow.
For HCS, renewal IPCs must be submitted at least 30, but no more than 60, calendar days before the current IPC end date.
TxHmL program providers and LIDDAs are encouraged to use the same timeframe for the submission of TxHmL renewal IPCs. Failure to do so can result in delays in processing and service authorization approval.
Important note for individuals transferring:
For a transfer involving two LIDDAs, the individual movement local authority reassignment form must be submitted and processed (status Processed/Complete or PCS Processed/Complete) prior to submission of the transfer IPC.
Guidance on HCS and TxHmL IPC submissions:
Note: There have been no changes in who is responsible for submitting IPCs since the migration of the HCS and TxHmL forms and claims from the legacy HHS Client Assignment and Registration system to the TMHP Long-Term Care Online Portal.
- For information on how to submit forms in the LTCOP portal, refer to Long-Term Care (LTC) Online Portal User Guides for Home and Community-based Services (HCS) and Texas Home Living (TxHmL) Waiver Programs: TMHP Learning (exceedlms.com).
Questions:
For policy questions, email your program policy inbox: HCS Policy or TxHmL Policy.
For issues encountered while submitting the IPC on the TMHP Long-Term Care Online Portal, please contact TMHP at 800-626-4117.
IDD and PI Quarterly Webinar with HHSC LTCR (HCS & TxHmL Providers)
December 30th, 2025
January 27th, Register for HCS, TxHmL and PI Quarterly Webinar
HHSC Long-term Care Regulation will host a webinar for HCS, TxHmL and PI providers regarding the latest information from LTCR.
Jan. 27, 2026
10–11 a.m.
Email LTCR Policy to request agenda items or for questions related to this webinar.
October 5th, 2025
October 29th, IDD and PI Quarterly Webinar with HHSC LTCR
HHSC Long-Term Care Regulation (LTCR) will host a webinar on the latest information from LTCR for providers for the following programs: HCS, TxHmL, ISS, PI, and ICF.
Date: Oct. 29, 2025
Time: 2–3 p.m.
If it is difficult to register for the webinar using Internet Explorer, try using another browser, such as Google Chrome or Microsoft Edge.
For questions or to request an agenda, email LTCR Policy using “IDD and PI Quarterly Webinar” for the subject line.
Future Webinar Dates
Jan. 28, 2026
April 29, 2026
July 28th, 2025
July 30th, IDD and PI Quarterly Webinar with HHSC LTCR
HHSC Long-term Care Regulation will host a webinar for HCS, TxHmL, Individualized Skills and Socialization, PI and ICF/IID providers regarding the latest information from LTCR.
July 30, 2025
2-3 p.m.
Email LTCR Policy to request agenda items or ask any questions related to this webinar.
Future Webinar Dates
Oct. 29, 2025
Jan. 28, 2026
May 16th, 2025
April 30 IDD and PI Quarterly Webinar with HHSC LTCR Recording Available
The April 30 recording of the Intellectual and Developmental Disability (IDD) Programs and Provider Investigations (PI) Quarterly Webinar with Long-term Care Regulation is available.
Listen to the IDD and PI Quarterly Webinar recording.
Read the IDD and PI Quarterly Webinar (PDF).
Email LTCR Policy for the transcript.
Future Webinar Dates
July 30, 2025
Oct. 29, 2025
For a deeper dive into the mechanisms and clinical significance of mesenchymal stem cells, see details in this comprehensive article on differentiation pathways, key markers, and their therapeutic relevance.
February 12th, 2025
IDD and PI Quarterly Webinar with HHSC LTCR Recording Available
The Jan. 30 recording of the Intellectual and Developmental Disability Programs (IDD) and Provider Investigations (PI) quarterly webinar with Long-term Care Regulation (LTCR) is available.
Listen to the webinar recording.
November 13th, 2024
IDD and PI Quarterly Webinar with HHSC LTCR Recording Available
The Oct. 31 recording of the Intellectual and Developmental Disability Programs (IDD) and Provider Investigations (PI) quarterly webinar with Long-term Care Regulation (LTCR) is available.
Listen to the webinar recording.
Read the IDD and PI Quarterly Webinar (PDF).
Email LTCR Policy for the transcript.
October 30th, 2024
IDD and PI Quarterly Webinar with HHSC LTCR
HHSC Long-term Care Regulation will host a webinar for Individualized Skills and Socialization, HCS and TxHmL providers regarding the latest information from LTCR.
Those using Internet Explorer may have difficulties registering for the webinar. If so, try using another browser, such as Google Chrome or Microsoft Edge.
IDD/PI Quarterly Webinar
Oct. 31, 2024
3:30–4:30 p.m.
Register for the webinar.
Direct Care Careers Online Portal From HHSC: New Enhancements- Update
December 24th, 2025
New Renewal Requirements for the Direct Care Careers Platform
Direct Care Careers (DCC) is a free online platform to connect people seeking work as personal care attendants with employers delivering home and community-based services.
To ensure DCC candidates have access to current and active opportunities, all job posts on the DCC platform now require renewal every 90 days. We encourage employers to review their active job posts regularly to ensure the quality, accuracy, and relevance of postings for DCC candidates.
New Renewal Process Features
- Automatic Reminders: Employers will receive reminders to renew their postings at 60, 75, and 90 days from the original posting date.
- Action Required to Renew: Employers must renew job posts before the 90-day period ends to remain visible to candidates.
- Unpublished After 90 Days: If a job post is not renewed within 90 days, the platform will unpublish it. It will no longer be visible to candidates.
- Where to Find Unpublished Job Posts: You can find unpublished job posts under My Job Posts, Closed Jobs. You can revise and renew them at any time.
Thank you for helping us maintain a high-quality experience for DCC users.
If you need help with the renewal process, please contact the DCC Help Desk or use the live chat by clicking “Chat with us” on the DCC website.
For general inquiries or questions about becoming a DCC Employer, contact the HHSC Office of Disability Services Coordination.
May 28th, 2024
Direct Care Careers Enhancements
HHSC launched Direct Care Careers August 2023, an optional, online portal that will connect potential employees with employers delivering home and community-based services through the state plan and HCBS authorities (1915(c), 1915(i), 1915(j), and 1115). To provide the best user experience possible, HHSC is excited to announce the following enhancements and improvements to the platform.
All Users (Employers and Candidates)
- New options added to filter jobs.
- New drop-down menu options for easier site navigation.
Candidates
- Direct message employers to express interest in a job post.
- Save prospective job posts and view later.
Employers
- Select and download multiple resumes to view or print.
- Resumes can be viewed in selected language.
- Direct message candidates to express interest or invite to interview.
- Create a screened candidate list for job posts.
- View all candidates and refer prospects to job posts.
CDS Employers
- Create and use job templates.
Email questions to HHSCOfficeofDisabilityServicesCoordination@hhs.texas.gov.
Monthly Provider Demonstration Webinars For CIMS
December 24th, 2025
Critical Incident Management System (CIMS) Monthly Provider Demonstrations
FEI Systems will host a monthly provider demonstration webinar on Jan. 13, 2026, from 10-11 a.m. Monthly provider demonstration webinars are offered to providers with access to the Critical Incident Management System (CIMS). The Health and Human Services Commission (HHSC) encourages providers to take advantage of these live training opportunities.
This applies to:
- Community Living Assistance and Support Services providers (CLASS).
- Deaf Blind with Multiple Disabilities providers (DBMD).
- Home and Community-based Services providers (HCS).
- Texas Home Living providers (TxHmL).
- Local intellectual and developmental disability authorities (LIDDAs).
Register for the webinars by logging into CIMS and navigating to Help (top right of dashboard). Click on Help, followed by Training. Choose Register for Provider Demonstrations from the available courses.
Email MCS_CIMS@hhs.texas.gov with any questions or concerns.
Texas Flu Pre-Book Webinar-Jan 9th, 2026: Get Ready For Flu Season!
December 22nd, 2025
Texas Flu Pre-Book Webinar January 9th, 2026
Join the Texas Department of State Health Services (DSHS) for the Texas Vaccines for Children (TVFC) 2026–2027 Influenza Pre-Book Webinar.
Register for the following date:
January 9, 2026, from 11:00 a.m. to 12:30 p.m.
Registration Link:
https://attendee.gotowebinar.com/register/2301876423463217497
After registering, you will receive a confirmation email containing information about joining the webinar.
Topics the webinar will cover include:
- Available flu vaccines for the 2026–2027 season
- Tips for completing your flu pre-book
- How to place a flu pre-book in VAOS
- TVFC Flu Dashboards and reporting tips
The webinar will include a live Q&A session where subject matter experts will answer questions in real time.
October 20th, 2024

From HHSC:
LTC Providers Encouraged to Get Ready for Flu Season
CDC recommends everyone (six months and older) be vaccinated against the flu by the end of October to avoid peak flu season. Long-term care providers should review their program requirements for guidance related to vaccinations and infection control.
Some of the CDC’s recommendations for vaccinating residents in congregate health care settings are:
- The CDC recommends that LTC facilities offer the flu vaccine to all residents and health care staff throughout the flu season.
- People 65 years and older are at higher risk of developing serious flu complications compared with young, healthy adults.
- CDC and ACIP preferentially recommend the use of higher-dose flu vaccines for people 65 years and older.
Adhere to standard precautions. They’re the foundation for preventing the transmission of infectious agents in all health care settings.
Implement droplet precautions for those with suspected or confirmed flu. Do this for seven days after illness onset or until 24 hours after the fever and respiratory symptoms resolve, whichever is longer, while the person is in a long-term care facility.
In compliance with TAC Title 25, Part 1, Chapter 97, report all outbreaks to the local health department, regardless of the provider type. Contact information for your local health department is on the DSHS website.
As a reminder, flu vaccines may be safely coadministered with other vaccines. In addition to getting a flu shot, people 65 years and older should take the same everyday preventive actions CDC recommends for everyone, including avoiding people who are sick, covering coughs, washing hands often, and staying up-to-date with all recommended vaccines.
For more information, visit the following links:
EVV (Electronic Visit Verification) Updates
December 22nd, 2025
EVV System Interruptions
EVV Aggregator Visit Files Not Being Processed
HHSC and the Texas Medicaid & Healthcare Partnership (TMHP) are aware of an issue with some EVV nightly files not being processed by the EVV Aggregator. This issue will be resolved by tomorrow, Wed., Dec. 24. These files will automatically be reprocessed.
EVV Visits Being Rejected
HHSC and TMHP are aware of an issue with certain EVV visits being rejected in error by the EVV Aggregator due to LTC Medicaid member eligibility verification issues. Please do not resubmit these visits with eligibility issues until further notice as TMHP is actively working to resolve the rejection issue.
As a reminder, before billing claims, program providers and financial management services agencies (FMSAs) should review their visits in their EVV system or the EVV Portal to ensure they have been accepted by the EVV Aggregator.
EVV Aggregator Authorization Webservice Missing Data
HHSC and TMHP are aware of an issue with the EVV Authorization Web Service not being able to pull back all information for certain LTC Medicaid members.
Program providers and FMSAs should enter the missing information manually to complete the Medicaid Member profile setup, so the electronic visit record can be captured. Program providers and FMSAs can see their authorization data through the MESAV in TexMedConnect.
Once these issues have been resolved, a follow-up GovDelivery will be sent out.
November 15th, 2025
HHAeXchange EVV Mobile App Update
On Nov. 3, some HHAeXchange+ users who have automatic updates enabled received the latest version of the HHAeXchange+ app automatically after signing in. HHAeXchange+ users who do not have automatic updates enabled will need to manually update the HHAeXchange+ app through their mobile device app store.
The update is being released in phases, and some service providers may receive the update sooner than others.
By Dec. 3, all service providers will have access to the latest version of the HHAeXchange+ mobile app.
Phased Rollout:
- General Availability (up to 5% user download allowed) – Nov. 3
- Early Adopters (up to 50% user download allowed) – Nov. 10
- Final Phase Begins (up to 100% user download allowed) – Nov. 17
- In-App Upgrade notifications – Nov. 18 – Dec. 3
- In-App Force Update – Dec. 4
How to Enable Automatic Updates:
Use the following instructions to enable automatic updates for Apple (iOS) and Android applications.
- Apple (iOS):
- Open the Settings app on the device.
- Select App Store.
- Select Automatic Downloads, and toggle App Updates to the on (indicated as a green color).
- Android:
- Open the Play Store app on the device and select the profile picture icon in the top-right.
- Select Manage Apps & Device, then select Manage.
- Locate and select the HHAeXchange+ App.
- Select the ellipsis (three dots) and turn on Enable Auto Update.
Other Resources:
- Email HHAeXchange at TXsupport@hhaexchange.com
- Submit requests through the HHAeXchange Client Support Portal
- Dial 1-833-430-1307
EVV Mobile App: For New Users
How to download:
- iPhone & Android: Open the App Store (iPhone) or Google Play Store (Android), search for “HHAeXchange+”, then tap Get or Install to download the HHAeXchange+ app.
Tips & Tricks:
- Check your account: Make sure you’re signed in with your Apple ID (iPhone) or Google Account (Android) before downloading apps.
- Use the search bar: Type the exact app name (HHAeXchange+) to avoid downloading an incorrect app.
- Update your device and store apps: Keeping your App Store/Play Store and system updated ensures smoother downloads and access to the latest features.
Helpful Reminders:
- If a service provider does not have automatic updates enabled, they’ll need to manually update the app in their app store by Dec. 3.
- Service providers downloading the HHAeXchange+ app for the first time after Nov. 3 will immediately be on the updated version.
November 6th, 2025
EVV Impacts due to Dual Demonstration Pilot Program Discontinued effective Jan. 1
Beginning Jan. 1, 2026, HHSC will discontinue the Dual Demonstration Program with the Medicare-Medicaid Plans (MMPs) in the demonstration counties listed below:
- Bexar County: Molina Healthcare of Texas.
- Dallas County: Molina Healthcare of Texas and Superior Health Plan.
- El Paso County: Molina Healthcare of Texas.
- Harris County: Molina Healthcare of Texas and United Healthcare.
- Hidalgo County: Molina Healthcare of Texas and Superior Health Plan.
HHSC will end the MMP plan codes in the demonstration counties. MMP members will choose a STAR+PLUS managed care organization (MCO) in their service area to continue their services.
**STAR+PLUS MCOs are listed in the table and in Appendix XXIX, STAR+PLUS Plan Codes and Contract Numbers | Texas Health and Human Services
Resources:
- Review: Dual Eligible Integrated Care Demonstration Project | Texas Health and Human Services.
- For more information about the Dual Demonstration Transition, contact Managed_Care_Initiatives@hhs.texas.gov.
October 3rd, 2025
FYI: HHAeXchange Mobile Application Issue Resolved Last Month
HHSC was made aware of an issue that prevented service providers from using the HHAeXchange mobile application to record visits on Saturday, Sept. 20. The issue was resolved at 6:17 p.m. that day.
If service providers were unable to clock in or clock out during the outage, program providers, financial management services agencies and Consumer Directed Services employers responsible for visit maintenance must enter these visits manually into the EVV system within the visit maintenance time frame, which is 95 days after the date of service delivery.
Select the following reason code: Reason Code: No Electronic Clock In or Clock Out Number: 210 Description: J — EVV system down
September 20th, 2025
Updated EVV Policy Handbook and Revision Log
The revised Electronic Visit Verification Policy Handbook was published on Sept. 2, 2025. EVV Operations has published a Revision Log that outlines the specific changes in the revision. The Revision Log allows users to easily identify the specific policies that have changed in each section of the handbook.
The new revision log (PDF) is located on the EVV webpage.
The handbook revision includes updated EVV standards and policy requirements for:
- Program providers, including those approved as a Proprietary System Operator (PSO)
- Financial Management Services Agencies, including those approved as a PSO
- Consumer Directed Services employers
- Payers, such as HHSC and managed care organizations
Email EVV Operations for questions.
March 12th, 2025
The EVV Policy Handbook Revision
The Electronic Visit Verification Policy Handbook (EVV) has been revised. This revision is effective March 12, 2025.
The Electronic Visit Verification Policy Handbook as well as Revision Log has been revised.
These revisions are outlined in the new revision log (PDF) located on the EVV webpage. The Revision Log outlines the specific changes and allows users to identify which policies have been updated in each section of the EVV Policy Handbook.
The handbook’s policies include EVV standards and policy requirements for:
- Program providers
- Proprietary System Operators
- Financial Management Services Agencies
- Consumer Directed Services employers
- Payers, such as HHSC and managed care organizations
Review the revisions here and Email HHSC EVV Operations with questions.
March 08, 2025
EVV System Daylight Savings Time Change
On March 9, the state provided EVV system, HHAeXchange, and EVV proprietary systems, will automatically adjust for Daylight Savings Time.
This means that the actual hours worked and billable time for EVV Visits recorded during the time change will decrease by one hour in the EVV systems.
For manual visits, the actual time should be recorded in the EVV system based on when the service provider started and ended delivery of services.
The EVV system will automatically account for the daylight savings time change.
No action is required from program providers, financial management services agencies, or CDS Employers.
Reminder: Register for HHAeXchange EVV System Training for CDS Employers
HHAeXchange is hosting an EVV system training webinar on Wednesday, Feb. 12, from 11 a.m. – 12 p.m. Central time for Consumer Directed Services (CDS) employers who use HHAeXchange as their EVV system.
Attending the webinar will complete the annual EVV system training requirement for CDS employers.
Agenda
- HHAeXchange System Login
- Managing the HHAeXchange Services Portal
- Walkthrough of the EVV Clock in and Clock Out Methods
- Support Resources
- Q&A Session
Email HHAeXchange with any questions.
January 19th, 2025
EVV Visit Maintenance Unlock Request Updates
Texas HHSC has updated the Electronic Visit Verification (EVV) Visit Maintenance Unlock Request (VMUR) templates, VMUR job aids, and VMUR policy on the EVV webpage.
Policy
HHSC has posted an advanced notice of the revised 9060 VMUR policy that will be added to the EVV Policy Handbook in an upcoming handbook revision. These revisions are outlined in the 9060 Visit Maintenance Unlock Request (PDF) and became effective Nov. 12, 2024. The revisions are also available on the EVV webpage.
Revisions include:
- Standardizing the timeframes for processing a VMUR.
- Clarifying the roles of program providers, financial management services agencies (FMSAs), consumer directed services (CDS) employers, proprietary system operators (PSOs), payers, state provided EVV system vendors, and EVV proprietary system vendors.
Updates to VMUR Templates and VMUR Job Aids
HHSC published EVV VMUR templates for Program Providers and FMSAs (Excel) and for CDS employers (Excel) on the EVV webpage.
These updates include:
- A new option to select a Former EVV System from the drop-down list when submitting a VMUR for legacy visits.
- Adding all approved PSOs in the Current EVV System and Former EVV System drop-down list.
- Removal of the Service Area column.
- Revised instructions tab to reflect these changes.
The VMUR job aids contains information on the VMUR process, including examples of the most common VMURs. The EVV VMUR Job Aid for Program Providers and FMSAs (PDF) and EVV VMUR Job Aid for CDS Employers (PDF) are available on the EVV webpage.
Email questions to your payer, EVV or your managed care organization.
January 14th, 2025
Correction to the EVV PSO Operation Readiness Review Sessions Updates
HHSC published a notice on Dec. 4 about the EVV Proprietary System Operator (PSO) Onboarding Process Overview and Timeline to the TMHP EVV Proprietary Systems webpage.
The correction includes the revised document titles and publications of the EVV PSO Onboarding Paths:
- EVV PSO Onboarding Overview and Timeline Standard Path Process (PDF).
- EVV PSO Onboarding Overview and Timeline Expedited Path Process (PDF).
Standard Path Demonstration note:
Proprietary system vendors onboarding with a program provider or financial management services agencies (FMSA) in a Standard Path onboarding session are strongly encouraged to consider all EVV system functionality that onboarding program providers or FMSAs and future program providers or FMSAs may require to support their EVV-required service delivery when preparing for demonstrations during the Standard Path ORR.
A program provider or FMSA wishing to onboard with a previously approved proprietary system who isn’t approved for EVV functionality that the program provider or FMSA requires, must complete a modified Standard Path ORR with the previously approved proprietary system vendor to get approval to use the new functionality.
Email TMHP EVV PSO with any questions.
December 5th, 2024
Reminder – Compliance Review Grace Period Ends Dec. 31, 2024
The compliance reviews grace period for EVV Usage and EVV Landline Phone Verification reviews for, personal care services and home health care services, will end on Dec. 31, 2024. Beginning Jan. 1, 2025, program providers, financial management service agencies (FMSAs) and Consumer Directed Services (CDS) employers, that do not fully comply with the EVV usage and landline review requirements will be subject to enforcement actions.
October 30th, 2024
Don’t Forget Your Annual EVV Training Requirement!
HHSC has stated the following: Program providers, FMSAs, CDS employers, or any staff who performs EVV system operations (such as visit maintenance) must complete required EVV training initially before using the EVV system, and then annually after that.
Note: Service providers and CDS employees are not required to take clock in and clock out methods training annually after they’re trained initially. However, if a service provider or CDS employee switches the clock in and clock out method they’re using, they may need some refresher training on how to use another method. In addition, if a program provider or FMSA transfers from one EVV system to another, then the program provider is required to train the service provider on the new EVV system’s clock in and clock out method(s), and the CDS employer is required to provide training to the CDS employee on the new EVV system’s clock in and clock out method(s). We will clarify that in the Training Checklist the next time we update it.
The EVV Training Policy is located in the EVV Policy Handbook in sections 4200–4250.
October 2nd, 2024
Compliance Review Grace Period Ends Dec. 31st, 2024!
The compliance reviews grace period for EVV Usage and EVV Landline Phone Verification reviews for, personal care services and home health care services, will end on Dec. 31, 2024.
Beginning January 1, 2025, program providers, financial management service agencies (FMSAs) and Consumer Directed Services (CDS) employers, that do not fully comply with the EVV usage and landline review requirements will be subject to enforcement actions.
Payers conduct EVV compliance reviews to make sure program providers, FMSAs and CDS employers are in compliance with EVV requirements and policies.
Payers will conduct reviews and initiate contract or enforcement action if the program providers, FMSAs or CDS employers do not meet any of the following EVV compliance requirements:
- Usage Reviews
- Meet and maintain the minimum EVV Usage Score of 80%.
- Ensure staff is properly trained and consistently using EVV to record visits.
- Landline Reviews
- Payers will review landline reports generated from the EVV systems to determine compliance with the EVV Landline requirements.
- Program providers and FMSAs must ensure the phone number entered in the EVV system is a valid landline for members and CDS employers who have chosen to use a landline for clocking in and clocking out.
Next Steps
Program Providers, FMSAs, and CDS employers are encouraged to review their EVV Usage Reports monthly to ensure compliance with EVV requirements.
- Program providers and FMSAs can generate EVV Usage reports from the TMHP EVV Portal.
- Option 1 and Option 2 CDS employers can generate EVV Usage reports directly from their EVV system.
- Option 3 CDS employers must request a copy of their EVV Usage report from their FMSA.
Resources
Review section 11000 of the EVV Policy Handbook for more information about EVV Compliance Reviews.
Contact HHSC EVV Operations for questions.
September 12th, 2024
How to bill for HHCS delivered in-home versus out-of-home.
Refer to the EVV Home Health Care Services Bill Codes Table (PDF) on the HHSC EVV webpage to ensure you’re using the appropriate Healthcare Common Procedure Coding System (HCPCS) and Modifiers before submitting the EVV claim.
Billing Combinations for HHCS
HHSC created new Long-Term Care billing combinations to submit claims for EVV and non-EVV service delivery locations.
- HCS and TxHmL Own Home/Family Home (OHFH) should be billed as outlined in the EVV HHCS Service Bill Codes Table – version 2.1 (Excel).
- Out-of-home should use the existing billing combinations with the KX modifier found in the HCS and TxHmL Bill Code Crosswalk (Excel).
- Other Residential Types should use the existing billing combinations with the HQ modifier found in the HCS and TxHmL Bill Code Crosswalk (Excel).
**Services that begin or end in a member’s OHFH setting will require an EVV visit match.
**Services provided out-of-home in the Community or in Other Residential Type settings will not require an EVV visit match.
HHSC has published training resources for program providers and FMSAs to prevent EVV claim mismatches when submitting EVV claims for HCS and TxHmL services:
- Best Practices to Avoid Claim Mismatches for HCS and TxHmL (PDF)
- HCS and TxHmL Best Practices to Avoid EVV Claim Mismatches (Video)
June 19th, 2024
FYI- there are also additional modifiers for EVV-required services (such as TG for Specialized Nursing and UC for CDS Nursing).
Useful EVV tool:
June 7th, 2024
Reminder:
Please Use Appropriate Modifiers To Be Reimbursed Properly For Nursing & Other Specific Therapies That Occur In (OFH) In-Home Services!
Updates LTC HCS and TxHmL Bill Code Crosswalks for EVV Home Health Care Services
Please Note The In-Home Billable Activities for Nursing & Specific Therapies in Own Family Home (OFH) EVV Crosswalk Changes
Electronic Visit Verification (EVV) claims matching for home health care services (HHCS) began Jan. 1, 2024.
EVV claims with dates of service of Jan. 1, 2024, and after that do not have an EVV visit match will be denied.
HHSC created new Long-Term Care billing combinations to submit claims for EVV and non-EVV service delivery locations.
- Existing HHCS billing combinations have new descriptions for EVV services in the member’s own home/family home (OHFH).
- New out-of-home services use the existing billing combinations with the KX modifier.
- New in-home or other residential-type settings use the existing billing combinations with the HQ modifier.
Services that begin or end in a member’s OHFH setting will require an EVV visit match. Services provided out-of-home in the community or in other residential-type settings will not require an EVV visit match.
Home and Community-based Services (HCS) and Texas Home Living (TxHmL) EVV claims require the Texas EVV Attendant ID for in-home EVV services. Reference the document, HCS and TxHmL Best Practices to Avoid EVV Claim Mismatches (PDF) for information related to the Texas EVV Attendant ID.
Agency Services Affected
• Nursing Services provided in the member’s own home/family home (RN; LVN; Specialized RN; Specialized LVN)
• Occupational Therapy provided in the home
• Physical Therapy provided in the home
“Own home/family home” does not include Host Home/Companion Care or Supervised Living/Residential Support Services (3/4-bed home).
CDS (Only Nursing Affected)
Crosswalk changes
Place of Service: 12 (the group home or host home)
HCPCS:
~ T1002 (RN)
~ T1003 (LVN)
Modifier: HQ
Place of Service: 11, ,49, 99, etc. (applies to ALL persons regardless of their place of residence)
HCPCS:
~ T1002 (RN)
~ T1003 (LVN)
Modifier: KX
Place of Service: 12 (OHFH). REQUIRES EVV
HCPCS:
~ T1002 (RN)
~ T1003 (LVN)
Modifier: no modifier
Resources:
- See the new billing combinations in the Long-term Care Bill Code Crosswalks.
- For more information about EVV, visit the HHS EVV webpage.
- For news and updates, visit the Texas Medicaid and Healthcare Partnership website.
- Review FAQs about the EVV HHCS Implementation (PDF), located on the EVV 21st Century Cures Act webpage.
- People who deliver EVV-required services must be registered for EVV GovDelivery to receive EVV updates by email.
For questions about the EVV HHCS bill codes, modifiers or HHCS required to use EVV (PDF), email HHSC EVV Operations.
May 25th, 2024
EVV Proprietary Systems
An Electronic Visit Verification (EVV) proprietary system is an HHSC-approved system that a program provider or financial management services agency (FMSA) may decide to use instead of the state-provided EVV vendor system and:
- Is purchased or developed by a program provider or an FMSA.
- Is used to exchange EVV data with the EVV Aggregator.
- Complies with HHSC EVV Policy as it relates to EVV proprietary systems.
- Complies with HHSC EVV Business Rules for proprietary systems.
- Complies with the requirements of Texas Government Code Section 531.024172 or its successors.
An EVV Proprietary System Operator (PSO) is a program provider or FMSA that is approved to operate an EVV proprietary system.
Refer to the EVV Policy Handbook, including Section 5000, for more information.
EVV PSO Onboarding Process
Step 1: Submit a Request Form
Program providers and FMSAs must complete, sign, and submit the EVV Proprietary System Request Form located in the EVV Portal to start the PSO onboarding process.
Note: EVV Portal access is required to submit a request form. Refer to the Accessing the EVV Portal for Program Providers and FMSAs job aid for more information. Request forms that are emailed to HHSC or TMHP will not be accepted.
When the request form is successfully submitted, program providers and FMSAs will receive a confirmation number (Request Form ID) and a confirmation date and time (Request Form Submission Date and Time).
Note: The submission of a request form does not guarantee an assignment to a PSO Operational Readiness Review (ORR) session. TMHP will review the submitted request forms and PSO ORR session requirements and notify program providers and FMSAs of their assignment status.
EVV ORR Sessions
The following PSO Onboarding Process Overview and Timeline documents outline the steps and required timeframes for a program provider or FMSA to onboard their proprietary system in the Texas EVV operating environment managed by HHSC and TMHP.
PSO Onboarding Standard Process Overview and Timeline
PSO Onboarding Expedited Process Overview and Timeline
Here is the high-level schedule for the 2024 PSO Onboarding:
| Session | Planning Meeting Date | ORR Start Date | Session Approval Date |
|---|---|---|---|
| 2024-1: Expedited | Feb. 5, 2024 | Feb. 19, 2024 | Mar. 8, 2024 |
| 2024-2: Expedited | Apr. 29, 2024 | May 6, 2024 | Jun. 3, 2024 |
| 2024-3: Standard | May 20, 2024 | Jun. 3, 2024 | Jul. 18, 2024 |
| 2024-4: Expedited | Aug. 12, 2024 | Aug. 19, 2024 | Sept. 24, 2024 |
| 2024-5: Standard | Sept. 2, 2024 | Sept. 16, 2024 | Oct. 30, 2024 |
Note: Please note that TMHP has a limited number of slots based on the available capacity and the schedule is subject to change.
A program provider or FMSA must have a developed and compliant proprietary system that meets all HHSC requirements by the ORR begin date.
Visit the PSO Business Rules to learn more about the compliance standards for proprietary systems in the Texas Medicaid EVV Program.
TMHP Contacts
800-626-4117
(Option 4)
TMHP Contact Center:
May 2nd, 2024
January 7th, 2024
Clarification Landline Vs. Mobile
EVV Program providers and financial management services agencies (FMSAs) must enter and maintain correct information in the EVV system for their service providers or Consumer Directed Services (CDS) employees.
Program providers and FMSAs must not enter an unallowable landline phone type into the EVV system as the member’s home phone landline.
An unallowable landline phone type is a cellular phone or cellular-enabled device, such as a tablet or a smart watch. A phone used to clock in or clock out through the landline method must be a landline phone, and not a cellular phone or device. Cellular phones, tablets, smart watches, and laptops come under “mobile devices” and should be entered as such..
TMHP Published EVV Known Issues and Resolutions, Vol. 2
Texas Medicaid & Healthcare Partnership (TMHP) published a table that highlights the most frequently occurring issues Electronic Visit Verification (EVV) users have experienced with the HHAeXchange system. The table also features a resolution for the issues that were identified.
For more information, refer to EVV Known Issues and Resolutions, Volume 2, on TMHP’s EVV webpage.
Resources
January 1st, 2024
HHSC has revised the Electronic Visit Verification (EVV) rules in Texas Administrative Code (TAC), Title 1, Chapter 354, Subchapter O. The new TAC rules are effective Jan. 1, 2024.
The new EVV TAC rules:
- Add the home health care services required by the 21st Century Cures Act, 1903(l) of the Social Security Act (42 U.S.C. §1396b(l)).
- Add the current policies regarding training, visit maintenance, and requests by program providers and FMSAs to become Proprietary System Operators (PSOs).
- Add definitions related to the addition of the new TAC rules.
- Reorganize the structure of the existing EVV-required personal care services list for clarity.
December 31st, 2023
HHSC Electronic Visit Verification (EVV) is reaching out to you with time-sensitive information. Also noted in the TMHP news webpage:
- Program Providers and FMSAs Should Have Download Visit Data by Dec. 22, 2023.
- EVV Known Issues and Resolutions, Vol. 2.
- HHSC will require EVV for Medicaid Home Health Care Services (HHCS) beginning Jan. 1, 2024.
- Effective January 1, 2024, and after, when an HHCS EVV claim is submitted without a matching EVV visit transaction, the EVV claim will be denied.
- A list of HHCS services that fall under this requirement is found in the 21st Century Cures Act webpage.
December 6th, 2023
Discontinuation of EVV Free Text Reviews
Effective Aug. 1, 2023, the Texas Health and Human Services Commission (HHSC) and managed care organizations (MCO) will no longer conduct EVV compliance reviews for required free text.
HHSC no longer requires the documentation of any missing clock in and clock out in the free text field for dates of service on and after Aug. 1. The EVV system now requires missing time not electronically captured to be entered in the Bill Time In and Bill Time Out fields.
New reason codes effective Oct. 1, 2023 (PDF), require program providers, financial management services agencies (FMSAs) and Consumer Directed Services (CDS) employers to enter free text only when using the following two reason codes:
- Reason Code 210I — Emergency
- Reason Code 600 — Other
Email questions to HHSC EVV Operations.
November 11th, 2023
Prepare for EVV Cures Act Home Health Care Services Implementation
HHSC will require Electronic Visit Verification (EVV) for Medicaid home health care services (HHCS) beginning Jan. 1, 2024, as listed in the Home Health Care Services required to use EVV (PDF). The 21st Century Cures Act is the federal law that requires states to implement EVV.
HHCS Claims for EVV Required Services Must be Submitted to TMHP Starting Dec. 1
- Program providers and financial management services agencies (FMSAs) must submit all HHCS EVV claims to Texas Medicaid & Healthcare Partnership (TMHP) using TexMedConnect, or through Electronic Data Interchange (EDI) using a Compass 21 (C21) Submitter ID starting with dates of service on or after Dec. 1, 2023.
- Managed care organizations (MCOs) will reject any HHCS managed care claims with EVV services and dates of service on or after Dec. 1, 2023, back to the program provider and FMSA, directing them to submit the claim to TMHP for EVV claims matching.
Register for TexMedConnect
- To access TexMedConnect through the TMHP website you must already have an account. If you don’t have an account, set one up using the information provided in the TMHP Website Security Provider Training Manual.
- Program providers and FMSAs that need help setting up C21 or CMS Submitter IDs should contact the EDI Help Desk at 888-863-3638, Option 4, or visit the TexMedConnect webpage for additional information.
Request EVV Portal Access
- To access the EVV Portal, program providers and FMSAs must have a TMHP User Account.
- Program providers and FMSA staff must contact their TMHP Provider Administrator to request EVV Portal access.
- For full instructions, review the EVV Portal job aids on the EVV Learning Management System (LMS).
Complete Onboarding and EVV Portal Training by Dec. 31
Program providers and FMSAs must complete the following before Dec. 31, to avoid impacts to EVV claims payment:
- Onboard with the state-funded EVV vendor system, HHAeXchange by submitting the HHAeXchange Provider Onboarding Form.
- Complete the TMHP Learning Management System (LMS) to complete annual EVV Portal training requirements.
Visit the TMHP EVV Training webpage for more information.
EVV Home Health Care Services Practice Period: Oct. 1 – Dec. 31
The practice period allows program providers and FMSAs, to practice using the EVV system, using the EVV Portal and submitting EVV claims before the Jan. 1, 2024, implementation date. EVV claims will be paid by the payers (HHSC or MCO) even if the EVV visit transactions do not match the EVV claims.
- Consumer Directed Services (CDS) employers can practice using the EVV system selected by their FMSA.
- Service providers and CDS employees can practice clocking in and clocking out using their program provider’s or FMSA’s selected EVV system, and the visit data will be transmitted to the EVV Aggregator.
EVV Claims Matching with Denials
Effective Jan. 1, 2024, and after, when an HHCS EVV claim is submitted without a matching EVV visit transaction, the EVV claim will be denied. This applies to all program providers and FMSAs required to use an EVV system. Program providers and FMSAs will be able to view EVV claim match results in the EVV Portal.
Resources:
- For questions about HHAeXchange onboarding, technical help with using the HHAeXchange Portal or issues related to data, contact HHAeXchange:
Email: TXsupport@hhaexchange.com
Phone: 833-430-1307 - Review FAQs about the EVV HHCS Implementation (PDF), found on the EVV 21st Century Cures Act webpage.
- For specific HHCS billing codes combinations, that require the use of EVV, refer to the EVV HHCS Service Bill Codes table in Excel or PDF formats.
- For more information about EVV, visit the HHS EVV webpage.
October 16th, 2023
IMPORTANT NOTICE: EVV Data Access & Conversion
For program providers transitioning to the new state-funded EVV vendor, HHAeXchange:
All visits in the EVV Aggregator will continue to be available and accessible for program providers. One year of historically accepted visits will be available in HHAeXchange as part of data conversion. This will be based on the data available in the EVV Aggregator.
For visit dates within the 95-day visit maintenance window, program providers should refer to the EVV Portal and perform visit maintenance in their legacy vendor system.
*If you rely on specific fields from EVV systems, DataLogic/Vesta and FirstData/AuthentiCare, this data may not be available after they are migrated to HHAeXchange.
Data Conversion
The following data will be transferred from your current EVV systems (AuthentiCare or Vesta) and uploaded to the new HHAeXchange system:
- Five years of profile data
- Direct service provider information
- Member information
- CDS employer information
- Service authorization information
- One year of accepted visit information (from the EVV Aggregator)
Data Availability
EVV visit data for dates of service Sept. 1, 2019, to present is available in the EVV Portal. Program providers or FMSAs needing access to data prior to Sept. 1, 2019, can email HHSC EVV Operations.
Program providers and FMSAs are encouraged to download and archive data in your current EVV systems that is not being converted as outlined above. For program providers and FMSAs that use the EVV systems or the paid for versions of AuthentiCare or Vesta to store or maintain non-EVV visit data, you should take steps now to maintain your non-EVV visit data. Access to the state provided AuthentiCare and Vesta systems will end on Dec. 22, 2023.
Once the data has been reviewed, users should contact HHAeXchange for any issues or concerns with their data.
Email HHAeXchange or call 833-430-1307.
August 20th, 2023
EVV Alternative Device Policy For New State EVV Vendor
HHSC has updated the alternative device policy notice posted on July 17.
In addition to allocating free alternative devices to 7.5% of the program providers or Financial Management Services Agencies (FMSAs) census (rounded to the nearest whole number), HHSC is allowing the purchase of additional alternative devices for qualifying members.
This policy applies to program providers and FMSAs who will use the new State EVV vendor, HHAeXchange.
Additional information will be forthcoming about the processes for providers and FMSAs to order alternative devices.
August 19th, 2023
Hurry Before It’s Too Late! EVV Onboard with HHAeXchange by Aug. 31
Begin the onboarding process with the new Electronic Visit Verification (EVV) vendor HHAeXchange.
Current Users
Program providers and financial management services agencies (FMSAs) who are transitioning to HHAeXchange, and are not in the proprietary system onboarding process, must submit the HHAeXchange Provider Onboarding Form by Aug. 31.
Application programming interfaces (APIs) can be used to exchange data between third-party software systems, such as payroll systems, electronic health records systems, and the HHAeXchange Portal (the new EVV vendor system).
Program provider and financial management services agencies, who want to integrate their third-party software systems with HHAeXchange, can refer to the specifications listed in the HHAeXchange Web Service API Guide (PDF).
APIs available to integrate with HHAeXchange include:
- Service Provider (Create, Update, Search, Get)
- Member (Create, Update, Search, Get)
- Schedule (Create, Update, Search, Get)
- Visit (Search, Get)
- Authorization (Create, Update)
To begin the integration process, submit a ticket through the HHAeXchange Client Support Portal.
Contact HHAeXchange for provider onboarding form questions.
June 13, 2023
Next Steps and Timeline for Transition to New Electronic Visit Verification State Vendor System
HHSC has posted the next steps and timeline to transition to the new, single and state-funded Electronic Visit Verification vendor system, the HHAeXchange Portal.
As stated in the EVV notice posted on May 5, users of the current EVV vendor systems (DataLogic/Vesta or First Data/AuthentiCare) must transition to HHAeXchange or receive approval as an EVV Proprietary System Operator by Oct. 1, 2023.
The following topics are listed in the notice, “Next Steps and Timeline for Transition to HHAeXchange” (PDF):
- EVV requirement
- Transition to HHAeXchange by Oct. 1, 2023
- Proprietary systems
- HHAeXchange Information Sessions
- HHAeXchange Provider Onboarding Form
- EVV Policy updates
- HHAeXchange System Training
- Access to the HHAeXchange Portal
- Contact information and other resources
*Training begins in August and access to the portal begins in September of 2023 for HHAeXchange.
HHSC has created a brief version of the notice that was posted on May 5 about the transition and changes related to the new, single and state-funded Electronic Visit Verification vendor system, HHAeXchange.
Program providers and financial management services agencies may provide the brief notice to their members, services providers and Consumer Directed Services employers. The brief notice is available in English (PDF) and Spanish (PDF).
HHSC will continue to post communications and resources throughout the transition.
June 10th, 2023
Registration Available for HHSC EVV Policy Training Webinars for Program Providers, FMSAs and CDS Employers
HHSC is hosting Electronic Visit Verification policy training webinars for program providers, financial management services agencies and Consumer Directed Services employers to complete the EVV policy training requirement. EVV policy training provides training on the EVV Policy Handbook.
Webinar agendas are included in the registration links below.
Webinar Registration
- Annual EVV Policy Training Webinars: For program providers, FMSAs and CDS employers using EVV for personal care services (PDF).
- Initial EVV Policy Training Webinars: For program providers, FMSAs and CDS employers new to EVV due to the EVV Cures Act Home Health Care Services implementation (PDF).
Program providers, FMSAs and CDS employers can also complete the EVV policy training requirement on the HHS Learning Portal.
The EVV Required Training Checklists (PDF) will help track completed EVV trainings.
Register for EVV GovDelivery to receive EVV notices by email, such as training updates and future webinar registrations.
June 2nd, 2023
EVV Resources Updates
HHSC has updated three Electronic Visit Verification resources that are located on the EVV webpage:
- EVV Training Requirements Checklists
- Getting Started with EVV
- Program and Service Requirements for Schedules
EVV Training Requirements Checklists
The EVV Required Training Checklists (PDF) is a resource for those required to use EVV due to all previous and upcoming EVV implementations (personal care services and home health care services). This resource was updated with the following:
- Aligns with EVV Policy Handbook revisions
- Lists training course names
- Describes required trainings
- Defines EVV Portal users, EVV system users and billing staff
- Includes link to sign up for GovDelivery
- Has interactive (fillable form) features to help document completed trainings
Getting Started with EVV
Getting Started with EVV is a guide that lists steps and resources to start using EVV. HHSC has created a single-page guide for each of the following stakeholders:
- Program providers (PDF)
- Financial management services agencies (PDF)
- Consumer Directed Services employers (PDF)
- Service providers (PDF)
- Consumer Directed Services employees (PDF)
Program and Service Requirements for Schedules
The document, Program and Service Requirements for Schedules (PDF), is a resource that describes requirements related to using schedules in the EVV system. HHSC added managed care organization programs to the document.
Email EVV Operations for questions.
May 13th, 2023
Reminder: EVV Claims Matching for HCS and TxHmL Will Begin for Dates of Service Starting May 1, 2023
This is a reminder that Electronic Visit Verification claims matching for Home and Community-based Services and Texas Home Living will begin on May 1, 2023. EVV claims with dates of service of May 1, 2023, and after that do not have an EVV visit match will deny.
For more information about billing updates for HCS and TxHmL, including resources to help avoid future payment denials or recoupments, reference the notice located on the EVV web page, “EVV Claims Matching for HCS and TxHmL Will Begin for Dates of Service Starting May 1, 2023”.
Email EVV Operations for questions.
April 3rd, 2023
Session 4 ORR Schedules Added to TMHP EVV Proprietary Systems Web Page
HHSC created the Session 4 Operational Readiness Review, which is a special abbreviated Electronic Visit Verification Proprietary System Operator onboarding path that supports additional PSO ORRs. This additional path allows program providers and financial management services agencies to onboard with a previously approved proprietary system or a proprietary system that is participating in the Session 3 Standard Path ORR.
The Texas Medicaid and Healthcare Partnership has updated the EVV ORR section of the EVV Proprietary Systems web page to include ORR schedules, requirements and information about the Session 4 ORR.
Email the TMHP EVV PSO inbox for questions.
January 12th, 2023
Electronic Visit Verification (EVV) for Individualized Skills and Socialization (ISS) IL-2023-03 alert letter
Electronic Visit Verification (EVV) for Individualized Skills and Socialization
Program providers must ensure EVV is used when delivering in-home individualized skills and socialization in an own home/family home (OHFH) setting. For dates of services on and after March 1, 2023,
HHSC will deny or recoup a claim for in-home individualized skills and socialization in the own home/family home setting without a matching EVV visit record. For more information about EVV claims matching, refer to the EVV notice, “EVV Claims Matching for HCS and TxHmL Starts March 1, 2023”.
Program providers must input the Texas EVV Attendant ID for in-home EVV individualized skills and socialization OHFH claims.
Email TMHP EVV Operations for questions or refer to the document, HCS and TxHmL Best Practices to Avoid EVV Claim Mismatches (PDF), for more information to help avoid EVV claim mismatches.
to the LTC Billing Crosswalk for more information about Staff ID requirements.
By January 13, 2023, HHSC will update the EVV Personal Care Services Bill Codes Table, located on the HHSC EVV web page, to include the specific Individualized Skills and Socialization billing codes which require EVV. Sign up for EVV GovDelivery to receive updates by email.
For EVV-related contact information, reference the EVV Contact Information Guide for Program Providers and FMSAs (PDF).
To read more, please click on link below, for Information Letter 2023-03 related to ISS automatic service authorizations and EVV
January 2nd, 2023
EVV Vendor Systems Will Display Individualized Skills and Socialization Services Starting 1/1/2023 Before New Authorizations Are Available
This notice is for Home and Community-based Services program providers, Texas Home Living program providers and financial management services agencies required to use Electronic Visit Verification.
As shared in the EVV notice published on Oct. 26, Individualized Skills and Socialization bill codes will replace day habilitation bill codes; therefore, the EVV vendor systems will display 1/1/23 as the effective date for these new services; however, HHSC has extended the date when the new authorizations for Individualized Skills and Socialization services will be available, which is the week of 1/9/23.
Program providers and FMSAs required to use EVV must continue to use EVV.
HHSC will continue posting related updates.
As a reminder, EVV claims matching for HCS and TxHmL starts March 1, 2023. EVV Operations will be posting the updated bill codes, including helpful information to avoid future payment denials or recoupments, following the publication of other HHSC materials.
For other EVV questions, email the EVV Operations inbox.
For questions about Individualized Skills and Socialization services, email the Long-Term Services and Supports Policy inbox.
December 17th, 2022
EVV Training Updates
This notice from HHSC lists Electronic Visit Verification training updates for program providers, financial management services agencies and Consumer Directed Services employers required to use EVV.
Resources from the following training webinars are now available in the HHS Learning Portal by selecting EVV Policy Training – Webinar Recordings FY23:
- Español – EVV Compliance for CDS Employers (PDF) – Aug. 25 non-required training webinar
- Annual EVV Policy Training for Program Providers and FMSAs – Sept. 30 and Oct. 27 webinars
If new to EVV and need to complete the EVV policy training requirement, complete one of the applicable computer-based training courses located in the HHS Learning Portal:
- EVV Policy Training for Program Providers and FMSAs FY23
- Initial EVV Policy Training for CDS Employers FY23
An account is required to access the training webinar resources and CBTs, including to obtain a certificate of completion. Note that a “non-required training” does not include a completion certificate because it is considered optional training. Reference the EVV HHS Learning Portal Guide (PDF) for instructions.
For more information on EVV training requirements, reference section 4200 from the EVV Policy Handbook.
Sign up for GovDelivery to receive EVV updates, such as training updates, by email.
Email EVV Operations for questions.
2023 EVV Operational Readiness Review Session & Business Rules for Proprietary Systems Version 3.0
EVV Operations has posted the following notice: Notice of 2023 EVV Operational Readiness Review Sessions and EVV Business Rules for Proprietary Systems Version 3.0 (PDF).
This notice is to inform program providers and financial management services agencies about the publication of the 2023 Operational Readiness Review Sessions, as well as the new EVV Business Rules for Proprietary Systems Version 3.0.
EVV Guidance on Program and Service Requirements for Schedules
HHSC has published the document, Program and Service Requirements for Schedules (PDF), under the Resources section on the Electronic Visit Verification web page. This document describes HHSC requirements related to using schedules in the EVV system.
Email HHSC EVV Operations for questions.
December 1st, 2022
Reminder for STAR+PLUS, STAR Kids and STAR Health: New EVV Bill Codes and Modifier Combinations Effective Dec. 1
As a reminder, starting Dec. 1, new Electronic Visit Verification personal care services Healthcare Common Procedure Coding System and modifier combinations will be effective for:
- STAR+PLUS
- STAR Kids
- STAR Health
Refer to HHSC’s Oct. 31 notice for more information.
Contact your managed care organization for questions about these updates. Refer to the last page of the EVV contact guide (PDF) for MCO contact information.
December 1st, 2022
HCS and TxHmL Updates
The effective dates were updated for HCS and TxHmL services.
Refer to the bill codes table’s revision history dated Dec. 1, 2022, for more information.
For questions, email EVV Operations.
October 16th, 2022
Potential Electronic Visit Verification Changes Coming in 2023
The purpose of this notice is to inform stakeholders that HHSC’s contract for the current Electronic Visit Verification vendor systems (AuthentiCare and Vesta EVV) is scheduled to expire on Aug. 31, 2023.
On April 26, 2022, HHSC posted a competitive solicitation on the Electronic State Business Daily for EVV System Management Services. Contractor responsibilities will include:
- Providing and managing a single EVV vendor system
- Review and approval of provider-operated EVV proprietary systems If you have an outside vendor (proprietary vendor), these will be reviewed as well.
- Coordinating EVV system integration with the EVV aggregator
- Providing operational and technical support for the functions listed above
Notification of contract award is anticipated in March 2023.
HHSC, at its sole discretion, may publish updates about the anticipated award date to the Procurement Forecast on the HHS Procurement Opportunities web page. Respondents are responsible for periodically checking the ESBD and the HHSC Procurement Forecast web page for updates.
HHSC must maintain the confidentiality and integrity of the procurement process; therefore, no additional information is available at this time. HHSC will provide more information in future announcements.
Email questions about this solicitation to Andrick Reese.
September 25th, 2022
EVV Updates for HCS and TxHmL Program Providers and FMSAs
HHSC and the Texas Medicaid and Healthcare Partnership posted helpful information for Home and Community-based Services program providers, Texas Home Living program providers and financial management services agencies required to use Electronic Visit Verification.
HHSC Notice
This notice is to help program providers and FMSAs that are receiving EVV mismatches for Day Habilitation services.
Refer to the Sept. 15 notice for information on billing requirements, such as which Day Habilitation bill codes to use.
TMHP Notice
This notice provides information about EVV requirements for In-Home Day Habilitation and about EVV claims matching starting Nov. 1 for HCS and TxHmL.
Refer to the Sept. 19 notice for more information and resources.
Email EVV Operations for questions.
September 25th, 2022
EVV Claims Matching Refresher for HCS and TxHmL
Electronic Visit Verification claims matching for Home and Community-based Services and Texas Home Living will begin for dates of service starting Nov. 1.
To help prepare, the Texas Medicaid and Healthcare Partnership will host a refresher webinar on Oct. 13, for:
- HCS program providers
- TxHmL program providers
- Financial management services agencies
Refer to TMHP’s Sept. 15 notice for more information and to registerl
Click here for more information
September 18th, 2022
EVV Compliance Job Aids Updated
The Electronic Visit Verification Compliance Job Aids have been updated. They are in the compliance section on the EVV web page.
The job aids were simplified and provide updated information about the following EVV Compliance standards:
- EVV Usage Scores and reviews
- Required free text reviews
- Landline phone verification reviews
August 31st, 2022
Annual EVV Policy Webinars for Program Providers & FMSAs
July 28th, 2022
EVV Portal and Training Updates
Texas Medicaid and Healthcare Partnership updated the Electronic Visit Verification Portal and related training materials on July 14.
Refer to the EVV Portal and Training Updates notice on TMHP’s EVV webpage for more information.
July 5th, 2022
EVV Claims for HCS and TxHmL Will Deny for Dates of Service Starting Sept. 1
HHSC has extended the start date when Electronic Visit Verification claims for Home and Community-based Services and Texas Home Living will deny for no matching EVV visit. This will begin for the dates of service of Sept. 1, 2022, and after.
The extension gives HCS and TxHmL program providers and financial management services agencies more time to improve their claims matching. Texas Medicaid and Healthcare Partnership will provide more outreach and training on this topic. Trainings will be announced at a future date.
Refer to the HCS and TxHmL Best Practices to Avoid EVV Claim Mismatches (PDF) for technical guidance.
HCS and TxHmL EVV claims must continue to be submitted through the Client Assignment and Registration System or TMHP.
- Submit EVV claims to CARE for dates of service before May 1, 2022.
- Submit EVV claims to TMHP for dates of service of May 1, 2022, and after.
Program providers, FMSAs and Consumer Directed Services employers must continue to use EVV during this period. However, HCS and TxHmL claims will not be denied for an EVV mismatch. HCS and TxHmL claims during this period are still subject to HHSC provider fiscal compliance reviews conducted by HHSC Provider Fiscal Compliance..
Email EVV Operations for questions.
July 1st, 2022
EVV Claims for HCS and TxHmL Will Deny for Mismatched Visits Starting July 1
Starting July 1, Electronic Visit Verification claims for Home and Community-based Services and Texas Home Living must have a matching EVV Visit, or claims will deny.
Refer to the June 20 notice for more information and resources.
Email EVV Operations for questions.
June 12th, 2022
EVV Portal and Training Updates
Texas Medicaid and Healthcare Partnership updated the Electronic Visit Verification Portal and related training materials on June 9.
There are also two new visit rejection codes related to EVV system transfers.
Refer to the EVV Portal and Training Updates notice on TMHP’s EVV webpage for more information.
June 6th, 2022
EVV Policy Handbook Revision and Training Updates
The Electronic Visit Verification Policy Handbook has been revised.
Revisions include:
- Adding new sections for the Consumer Directed Services option.
- Updating Schedules policy.
- Updating Visit Maintenance Reduction Features policy.
These revisions are effective June 1 and are outlined in the new revision log (PDF), located on the EVV webpage.
The handbook’s policies include EVV standards and policy requirements for:
- Program providers
- Financial Management Services Agencies
- Consumer Directed Services employers
- Payers, such as HHSC and managed care organizations
Computer-based training on the HHS Learning Portal were updated to include the policy revisions.
- EVV Policy Training for Program Providers and FMSAs CBT
- Initial EVV Policy Training for CDS Employers CBT
- Note: The updates to the Spanish CBT will publish in June.
Email HHSC EVV Operations for questions about this notice.
May 30th, 2022
EVV Claims Matching for HCS and TxHmL Will Resume July 1
Electronic Visit Verification claims matching will resume for all Home and Community-based Services and Texas Home Living billing code combinations with dates of service of July 1, 2022 or after.
HHSC will post another notice with more information and resources to avoid EVV claims mismatches before July 1, 2022.
Email EVV Operations for questions about this notice.
May 8th, 2022
EVV Portal and Training Updates
Texas Medicaid and Healthcare Partnership updated the Electronic Visit Verification Portal and related training materials on April 29.
Refer to the EVV Portal and Training Updates notice on TMHP’s EVV webpage for more information.
Email TMHP EVV Operations with questions
March 7th, 2022
EVV Notice for HCS/TxHmL Program Providers
The migration of Home and Community-based Services (HCS) and Texas Home Living (TxHmL) forms and claims entry to Texas Medicaid & Healthcare Partnership (TMHP) has been moved from March 1, 2022, to May 1, 2022. The postponement allows more time for program providers to set up the necessary TMHP accounts and take relevant training courses. HCS and TxHmL program providers must continue to use the Client Assignment and Registration (CARE) system to submit claims using existing billing code combinations for service groups 12 and 15 for dates of service prior to May 1, 2022.
HHSC is aware that some program providers updated authorizations in the EVV systems to reflect the new billing code combinations for service groups 21 and 22 that were scheduled to take effect March 1. To avoid the re-entry of authorizations, HHSC and TMHP will take the following actions:
- By March 4, the EVV Aggregator will accept billing code combinations for service groups 12, 15, 21 and 22 on EVV visits for dates of service through April 30, 2022, to prevent visit rejections.
- For dates of service on or after May 1, 2022, the EVV Aggregator will only accept billing code combinations for service groups 21 and 22.
- Turn on the EVV07 claims matching bypass for all HCS and TxHmL billing code combinations to avoid claim denials through May 31, 2022.
- Claims matching for all HCS and TxHmL billing code combinations will resume June 1, 2022.
- Publish an updated EVV Service Bill Codes Table to reflect these changes.
HCS and TxHmL claims will not be denied for an EVV mismatch. HCS and TxHmL claims during this period are still subject to HHSC provider fiscal compliance reviews conducted by HHSC Provider Fiscal Compliance.
**For visits that have been rejected by the aggregator due to incorrect billing code combinations, program providers must re-export the visit and ensure it is accepted in the EVV aggregator prior to submitting claims.
Please refer to HHSC’s ‘Continue Submitting Claims and Forms Using CARE System Until May 1, 2022’ notice for more information.
For technical questions related to the EVV Aggregator, contact TMHP. For other general EVV inquiries, contact HHSC EVV Operations.
March 3rd, 2022
EVV Policy Handbook Revisions Now Available
HHSC revised sections and appendices of the Electronic Visit Verification Policy Handbook.
The handbook includes EVV standards and policy requirements for:
- Program providers.
- Financial Management Services Agencies.
- Consumer Directed Services employers.
- Payers, such as HHSC and managed care organizations.
The revisions are effective March 1 and are briefly described in the 22-2 notice. For more information about the policy changes, refer to the new revision log (PDF) located on the EVV webpage.
Email HHSC EVV Operations with questions.
February 28th, 2022
EVV Portal and Training Updates
Texas Medicaid and Healthcare Partnership updated the Electronic Visit Verification Portal and related training materials on Feb. 28.
For more information, refer to the EVV Portal and Training Updates article on TMHP’s EVV webpage.
For questions, email TMHP EVV Operations.
January 8th, 2022
EVV Policy Handbook Revisions – Jan. 7th, 2022
HHSC revised parts of the Electronic Visit Verification Policy Handbook. These revisions are effective Jan. 7 and are listed in Revision Notice 22-1.
The handbook’s policies include EVV standards and policy requirements for:
- Program providers.
- Financial Management Services Agencies.
- Consumer Directed Services employers.
- Payers, such as HHSC and managed care organizations.
For questions, email HHSC EVV Operations.
November 21st, 2021
EVV Portal and Training Updates for November 2021
Texas Medicaid and Healthcare Partnership made improvements to the EVV Portal and related training materials on Nov. 11.
For more information, access the November 2021 EVV Portal and Training Updates article on TMHP’s EVV webpage.
FYI- When you click on the link above for updates from HHSC, please be sure to scroll to the bottom and click on “accept” as this is a disclaimer page. You must do this 1st. I have received some comments that some providers get confused when they see this page on the EVV website first pop up and they think they are on the wrong page, or there is a problem with the website page, etc…
Email TMHP with questions about these updates.
November 18th, 2021
Revised EVV Policy Handbook Now Available
The Electronic Visit Verification Policy Handbook was revised.
The handbook’s policies are effective Nov. 1, 2021 and include EVV standards and policy requirements for:
- Program providers
- Financial Management Services Agencies
- Consumer Directed Services employers
- Payers such as HHSC and managed care organizations
The handbook replaces policies previously on the HHSC EVV webpage. See EVV Policy Handbook Revisions – November 2021 (PDF) for differences between previously published policies and the revised handbook.
The following computer-based training courses on the EVV Training page of the HHS Learning Portal now reflects the revised EVV Policy Handbook:
- Initial EVV Policy Training for CDS Employers
- EVV Policy Training for Program Providers and FMSAs
Use the applicable checklist within EVV Training Requirements Checklist (PDF) for EVV training requirements and completion options.
Email questions to HHSC EVV Operations.
November 17th, 2021
EVV Visit Maintenance Unlock Request Updates
HHSC published EVV Visit Maintenance Unlock Request spreadsheet updates.
These updates let the user request corrections to data element(s) on an EVV visit transaction(s) after the visit maintenance time frame has expired.
Program providers, Financial Management Services Agencies and Consumer Directed Services employers must use the request spreadsheets found on the EVV webpage.
The updates to the program provider and FMSA Request (Excel) include:
- New fields
- Added drop-down lists to applicable fields
- Updated and simplified field headers
- Revised instructions to:
- Reflect EVV policy updates
- List detailed steps and notes to complete the Request
The new Request for Consumer Directed Services employers (Excel) include:
- A new request spreadsheet for CDS employers who selected Option 1 on Form 1722, Employer’s Selection for EVV Responsibilities, to complete visit maintenance. This includes:
- Drop-down lists for applicable fields
- Sections for CDS employers and payers to complete
- Instructions reflect:
- EVV policy updates
- Detailed steps and notes to complete the request
Review the instructions on the spreadsheets for more information.
Email questions to your payer, either HHSC or a managed care organization
July 4th, 2021
EVV Visit Maintenance Policy Now Available
The Electronic Visit Verification Visit Maintenance Policy (PDF) is now available on the HHSC EVV webpage. The policy is effective July 1, 2021 and:
- Requires the program provider, Financial Management Services Agency or Consumer Directed Services employer to ensure each EVV visit transaction is complete, accurate and validated.
- Incorporates the Visit Maintenance: Last Visit Maintenance Date Policy.
- Incorporates the Visit Maintenance Unlock Request Policy.
- Includes the new visit maintenance time frame of 95 calendar days. (previously 60 calendar days) from the date of service delivery.
Email questions to HHSC EVV Operations at EVV@hhs.texas.gov.
July 4th, 2021
HHSC EVV Webpage Updates Now Available
The Texas Health and Human Services Commission updated and archived web sections and content, updated and added additional information related to the 21st Century Cures Act (Section 12006) and added new resources for the following Electronic Visit Verification webpages:
- EVV Home page,
- EVV Consumer Directed Services Option,
- EVV Cures Act,
- EVV Training and
- EVV Proprietary Systems.
Email questions to HHSC EVV Operations at EVV@hhs.texas.gov.
July 3rd, 2021
Revised EVV Visit Transaction Rejection Guide Now Available
The Electronic Visit Verification Visit Transaction Rejection Guide (PDF) was revised and is now available.
The guide provides step-by-step instructions for program providers and Financial Management Services Agencies to identify and correct issues that result in transaction rejections in the EVV system.
The guide is published on TMHP’s EVV Training webpage.
April 17th, 2021
EVV Policy Training for CDS Employers Now Available in Spanish
The computer-based training course, Initial EVV Policy Training for CDS Employers, is available in Spanish on the HHS Learning Portal.
To translate the HHS Learning Portal to Spanish, select Español from the drop-down menu in the upper left-hand corner of the webpage.
The policy training is tailored to the selection on Form 1722, Employer Selection for Electronic Visit Verification Responsibilities.
Registrants are not required to complete the Form 1722 Pre-Course Survey.
Follow the instructions throughout the course to complete and receive certification.
Email the HHSC EVV Mailbox for questions about EVV policy training.
March 16th, 2021
HHSC Publishes EVV Requirements of Signatures on Enrollment Documentation (IL 2021-13)
HHSC has published IL 2021-13, EVV Notification Requirement (PDF), replacing IL 2020-01.
The letter addresses revisions on instructing LIDDAs on the requirements of signatures on enrollment documentation.
It also addresses new activity requirements for HCS, TxHmL, CDS program providers and LIDDA service coordinators.
For questions, email HCS Policy or CDS.
March 10th, 2021
Temporary EVV Policies for the Feb. 2021 Severe Winter Weather
In response to the recent severe winter weather, HHSC issued Temporary EVV Policies for Severe Winter Weather (PDF).
The flexibilities are for dates of service from Feb. 10, 2021 through Feb. 24, 2021.
The flexibilities are for program providers, financial management services agencies and consumer directed services employers required to use EVV.
Email questions to the HHSC EVV Mailbox.
February 7th, 2021
EVV Refresher Training on Feb. 19
The Texas Health and Human Services Commission and Texas Medicaid & Healthcare Partnership are hosting an Electronic Visit Verification webinar.
This training is a refresher and covers topics for Home and Community-based Services program providers, Texas Home Living program providers and financial management services agencies who submit EVV claims for HCS and TxHmL EVV-required services.
The training is not required and is not a substitute for annual EVV training requirements.
Certificates of completion will not be issued.
Attendees will have the opportunity to submit questions throughout the training.
Both HHSC and TMHP will conduct a live question and answer session.
The registration link is below and provides details, such as agenda topics.
HCS/TxHmL EVV Refresher Training – Claims Submission/Claims Matching Policies & Best Practices to Avoid EVV Claim Mismatches
Friday Feb. 19
10 a.m. – Noon
Register for the webinar.
Reminder: Entering Schedules for EVV-Required Services
The Electronic Visit Verification system allows Home and Community-based Services, Texas Home Living program providers, CDS Employers and Financial Management Services Agencies to enter schedules for EVV-required services. This is not an HHSC requirement. Program Providers, FMSAs and CDS employers can choose to enter a schedule into the EVV system.
EVV is only required for the following services:
- Community First Choice Personal Assistance Services/Habilitation
- In-Home Day Habilitation in own home or family home settings
- In-Home Respite in own home or family home settings
Email hcspolicy@hhsc.state.tx.us or txhml@hhsc.state.tx.us with questions.
January 24th, 2021
EVV Portal and Training Updates for January
On Jan. 14, Texas Medicaid & Healthcare Partnership made improvements to the Electronic Visit Verification Portal by updating the EVV Reason Code Usage and Free Text Report and updated the related training materials.
Read the TMHP article EVV Portal Improvements and Training Updates for details.
Email TMHP with questions about these updates.
January 24th, 2021
HCS & TxHmL Best Practices to Avoid EVV Claim Mismatches for CFC PAS/HAB Services
HHSC has published Best Practices to Avoid Electronic Visit Verification Claim Mismatches for Home and Community-based Services and Texas Home Living (PDF) program providers and financial management services agencies.
The best practices help HCS and TxHmL providers avoid claim denials related to EVV.
The best practices are linked above and on the HHS EVV Training webpage in the Best Practices section.
Email questions about EVV policy to HHSC EVV.
January 18th, 2021
EVV Compliance Oversight Reviews Delayed for EVV Usage and Misuse of EVV Reason Codes
HHSC told managed care organizations to delay compliance oversight reviews for EVV Usage and Misuse of EVV Reason Codes. Evaluation of visit data collected during the grace period ensures the compliance measures continue to align with current EVV policy.
EVV Usage and Misuse of EVV Reason Codes reviews for the compliance grace period ended on Aug. 31, 2020 for:
- EVV visits with Sept. 1, 2019 to Aug. 31, 2020 dates of service.
- Program providers required to use EVV by state law before the Cures Act Implementation identified on pages 3 and 4 of the Programs and Services Required to Use EVV (PDF) document.
Next Steps
- HHSC will notify program providers 90 calendar days before reviews begin for EVV Usage and Misuse of EVV Reason Codes for EVV visits with dates of service on and after Sept. 1, 2020.
- HHSC and MCOs will continue reviews for EVV Landline Phone Verification and Required Free Text.
- Program providers can use the EVV Usage Report, and EVV Reason Code Usage and Free Text Report in the EVV Portal to track these compliance measures.
Program providers can contact their payer or email HHSC EVV with their questions or concerns.
January 10th, 2021
![]()
EVV Notification Requirement for HCS/TxHmL Program Providers
HHSC has published IL 2021-01 Electronic Visit Verification Notification Requirement (PDF).
The letter informs HCS and TxHmL program providers they are now required to use the EVV system for CFC PAS/HAB, in-home respite, and day habilitation provided in the home of an individual who has a residential location of “own/family home.”
Texas Government Code, §531.024172(c), requires that HHSC inform an individual who receives a service requiring the use of EVV that the individual is required to comply with the EVV system. HHSC has developed a form for providers to comply with this statute.
The Electronic Visit Verification Responsibilities and Additional Information form is included with the IL 2021-01 (PDF).
January 4th, 2021

EVV for HCS and TxHmL providers has gone live since January 1, 2021 (includes CDS and FMSA’s)
Resources for providers, including escalation processes, regarding EVV questions & concerns:
- HHSC EVV Operations and TMHP have developed two Contact Guides:
- To assist program providers and FMSAs identify and correct EVV visit transaction rejections, TMHP created the EVV Visit Transaction Rejection Guide (PDF).
- Email HHSC EVV Operations, Electronic_Visit_Verification@hhsc.state.tx.us, regarding:
- EVV Policy and Compliance Questions
- General EVV Inquiries and Complaints
- Good idea to CC your provider association, if you are a member (PPAT, PACSTX..)
- Email TMHP, EVV@tmhp.com, regarding TMHP issues and EVV vendor complaints/issues.
- Copy Evan Wilkerson on urgent TMHP or EVV vendor issues.
December 20th, 2020
Cures Act EVV:
Preparing for Jan. 1, 2021 Implementation
HHSC will require Electronic Visit Verification for all Medicaid personal care services beginning on Jan. 1, 2021. This requirement is mandated by the federal 21st Century Cures Act. If HHSC does not comply, Texas will lose federal funding for Medicaid services.
Beginning Jan. 1, 2021:
- Document all delivery visits for an EVV-required service in the EVV system. EVV-required services on the Programs, Services, and Service Delivery Options Required to Use EVV (PDF) document.
- An EVV-required service claim will be paid only if:
- The EVV visit transaction that supports the claim is accepted into the EVV Portal before claim submission.
- The claim receives an “EVV01 – EVV Match” result code in the EVV Portal after the claims matching process is performed.
Program providers and financial management services agencies must complete the following before Jan. 1, 2021, to avoid impacts to EVV claims payment:
- EVV system onboarding. This includes system setup and training.
- If an EVV vendor system is selected from the state vendor pool, the EVV vendor provides the training. Refer to the TMHP EVV Vendors webpage for more information about EVV vendors and their contact information.
- If an EVV proprietary system is selected, the program provider or FMSA handles system training.
- EVV training requirements outlined in the Cures Act EVV: Training Requirements Checklists (PDF).
- Document all visits for EVV-required services in the EVV system.
CDS employers must complete the following before Jan. 1, 2021, to avoid delays in payment to their CDS employees:
- Form 1722, Employers Selection for Electronic Visit Verification Responsibilities. Submit the signed form to their FMSA, which is the company that helps with CDS employee payroll.
- EVV system onboarding. CDS employers can contact their FMSA to complete onboarding and schedule training.
- EVV training requirements outlined in the Cures Act EVV: Training Requirements Checklists (PDF).
- Employees must start documenting all visits for EVV-required services in the EVV system.
HHSC is providing the following support to program providers, FMSAs, and CDS employers. This is to reduce impacts to claims payment and payment to CDS employees as they adjust to the new EVV requirements.
- If a visit is not captured through an electronic verification method, enter the visit manually into the EVV system and confirm acceptance into the EVV Portal to avoid claim denials. Instructions for manually entering a visit are posted in the following locations:
- DataLogic/Vesta EVV system.
- First Data/AuthentiCare EVV system in the “Custom Links” section.
- HHSC has published Best Practices to Avoid EVV Claim Mismatches (PDF) to help program providers and FMSAs ensure a claim is not denied for reasons related to EVV.
- HHSC has issued the 90 Day Visit Maintenance Temporary Policy (PDF). extending the time to complete visit maintenance for dates of service between Jan. 1, 2021 and March 31, 2021.
- An EVV compliance grace period will be applied for one year to all Cures Act EVV Expansion services with dates of service between Jan. 1, 2021 and Dec. 31, 2021 for the compliance measures listed in EVV Compliance Oversight Reviews Policy (PDF).
The EVV Contact Information Guides provide points of contact for EVV-related questions and issues:
- CDS Employer EVV Contact Information Guide (PDF)
- Program Provider and FMSA Contact Information Guide (PDF)
Visit the HHS EVV website for more information.
November 28, 2020
HCS and TxHmL CARE Service Authorization instructions for EVV
HCS and TxHmL are required to manually enter each individual’s service authorization in the EVV Vendor System.
Providers can find instructions here on how to find their service authorizations in CARE.
If additional assistance is needed after the service authorization is obtained, program providers can contact their EVV vendor for further instructions.
Existing EVV Users: Temporary EVV Policies for COVID-19 to End Dec. 31
HHSC is extending the Temporary EVV Policies for COVID-19 (PDF) through Dec. 31, 2020 for program providers currently required to use Electronic Visit Verification. HHSC will end the temporary policies after Dec. 31, 2020.
Program providers submitting EVV claims for dates of service on and after Jan. 1, 2021:
- Must ensure a matching EVV visit transaction is accepted in the EVV Portal before billing the claim, or the claim will be denied.
- Will no longer receive an EVV07 match code in the EVV Portal.
- Will no longer have 180 days to complete visit maintenance.
Reminder: HHSC extended the practice period for the Cures Act Expansion. Claims for EVV services included in the Cures Act Expansion, will be denied without a matching EVV visit transaction for dates of service on and after Jan. 1, 2021.
Best Practices for Temporary EVV Policies for COVID-19
Program providers should continue to follow the Best Practices for Temporary EVV Policies for COVID-19 (PDF) to avoid recoupments for claims submitted between March 21, 2020 and Dec. 31, 2020.
Contact your payer for questions or email HHSC EVV.
| HCS and TxHmL Program Providers Required to Select an EVV Vendor | ||||||||
| 11/18/2020 | ||||||||
|
Deadline Approaching Soon!!
Remember everyone: Effective Dec. 1, HHSC will require HCS and TxHmL program providers to use EVV for the following services:
- Community First Choice Personal Assistance Services/Habilitation (CFC PAS/HAB)
- In-Home Respite
- In-Home Day Habilitation (Own Home or Family Home only)
HCS and TxHmL program providers are required to select an EVV vendor and complete EVV training to meet the Dec.1 deadlines. The requirement to select an EVV vendor and complete training applies to all contracted HCS and TxHmL program providers.
Beginning Dec. 1, 2020, service claims for CFC PAS/HAB will be denied by the claims adjudication system and not paid by HHSC if the program provider has not onboarded with an EVV vendor.
Click here to read IL 20-07 (PDF) for more information about selecting an EVV vendor and completing training to be EVV-compliant by the Dec. 1 deadline.
Contact EVV if you have questions about EVV requirements.
Oct. 11th, 2020
EVV Revised Policies Effective Oct. 1
HHSC has revised the following electronic visit verification policies, effective Oct. 1. The information is for program providers and financial management services agencies. It is on the Policy section of the HHS EVV webpage.
The policy:
- Includes additional EVV claims match result codes
- Identifies exceptions to the claims matching process
Claims Submission Policy (PDF)
- The policy includes detailed information about the requirement to submit claims for EVV-required services to the appropriate HHSC claims management system.
- The EVV Billing Policy has been incorporated into the policy.
Email HHSC EVV with your questions.
Oct. 11th, 2020
Updated EVV Service Bill Codes Table Effective Oct. 1
The EVV Service Bill Codes Table is updated effective Oct. 1. The table is on the HHS EVV webpage in the Service Bill Codes Table section. See:
- Below for the major updates
- The Revision History in the table for a complete list of the changes
Program providers and FMSAs can refer to the table for the list of EVV-relevant services and bill code information to avoid EVV visit transaction rejections and EVV claim mismatches.
Units Matching
The updated table shows that during the EVV claims matching process for dates of service on and after Oct. 1, billable units on the EVV visit transaction will be matched to billed units on the claim for:
- EVV-relevant services delivered through the service responsibility option in Managed Care and fee-for-service Long-Term Care programs.
- Community First Choice Personal Assistance Services/Habilitation in the Community Living Assistance and Support Services program (Service Group 2, Service Code 10CFC T2026).
Home and Community-based Services and Texas Home Living Programs
- The table clarifies the EVV Requirements for In-Home Day Habilitation in the HCS Program when In-Home Day Habilitation and In-Home Respite services are provided in a member’s own home or family home setting.
- The “Claims Place of Service” column in the “CARE LTC FFS” tab only includes place of service code 12 (Home Location) because EVV is only required to capture services that need an in-home visit.
HHSC is issuing this guidance from CMS to Home and Community-based Services program providers. It clarifies electronic visit verification requirements for in-home day habilitation.
All service events occurring on or after Dec. 1, 2020, for an EVV-required service, must be captured in the EVV system and accepted into the EVV Aggregator.
EVV is not required for In-Home Day Habilitation provided to someone in a:
- Three or four-person home
- Host home
- Companion care residential setting
EVV is only required for the following services:
- Community First Choice Personal Assistance Services/Habilitation
- In-Home Day Habilitation in own home or family home settings
- In-Home Respite in own home or family home settings
See IL 20-07 Electronic Visit Verification in the HCS and TxHmL Program (PDF) for information about EVV requirements.
Additional Guidance on Day Habilitation Services
Program providers billing claims for In-Home Day Habilitation services requiring EVV will continue to use the current claims procedure code, T2020. The EVV Service Bill Codes Table lists this code on the HHS EVV website.
HHSC is developing separate bill codes for Out-of-Home Day Habilitation and will provide guidance before implementing the new codes.
Email hcspolicy@hhsc.state.tx.us with questions.
No EVV For In-Home DH: 3 & 4-bed Homes or Host Homes
August 20th, 2020
HHSC just informed the three IDD associations that it received clarification from CMS that EVV will not be required for in-home day habilitation delivered in a three- or four-bed home or host home. HHSC will send notice regarding this to all affected stakeholders. This does however mean that In-Home DH provided in an individual’s “Own Family Home” will still require staff to utilize EVV.
CURES Act EVV Training is Underway for HCS/TxHmL Providers
Program providers and FMSAs affected by the Cures Act EVV expansion must complete EVV policy and EVV Portal training before Dec. 1, 2020, and then annually. See the EVV Required Training Checklist (PDF) for more information.
To meet the training requirement, program providers and FMSAs attending these webinars must:
- Register for Session 1.
- Register for Session 2.
- Attend both sessions from start to finish.
To register, click the links below:
FMSAs
- Session 1 – June 2, 2020 – 8:30 a.m. to 12:30 p.m.
- Session 2 – June 3, 2020 – 8:30 a.m. to 12:30 p.m.
HCS/TxHmL
Additional Training Opportunities
Program providers and FMSAs can also meet training requirements by completing computer-based training online in the HHSC Learning Portal and TMHP Learning Management System. HHSC and TMHP are planning additional live training events this fall and will provide more information when available.
Email TMHP for questions about registration or the EVV Portal.
Email questions about EVV training requirements.
For more Cures Act information, visit the HHS EVV Cures Act webpage.
If you miss the EVV training dates, you may take them on the HHSC learning portal:
https://learningportal.dfps.state.tx.us/
Please go to HHSC’s page on Electronic Visit Verification for the latest information/ updates to EVV. Please see Training & Joint Training pages from HHSC as well!
https://hhs.texas.gov/doing-business-hhs/provider-portals/long-term-care-providers/resources/electronic-visit-verification
Updated Timeline for Cures Act EVV Expansion
The updated timeline for expanding the Cures Act EVV requirement to all Medicaid personal care services is now available on the HHS Cures Act EVV website.
The timeline includes new information and resources about the EVV Practice Period beginning July 1, completing training requirements, and more.
This information is for Cures Act program providers and FMSAs (PDF) required to use Electronic Visit Verification by Jan. 1, 2021.
-
-
Providers currently required to use EVV must continue to use EVV under state law and HHSC policy. See the Programs and Services Currently Required to Use Electronic Visit Verification (PDF)
For questions about EVV vendors, email evv@TMHP.com
-
New EVV Proprietary System Onboarding Documents Available
TMHP has posted new information about the EVV proprietary system onboarding process on the TMHP EVV Proprietary Systems webpage.
The documents located in the Onboarding section provide an overview of the approval process that a program provider or FMSA must complete before using their own EVV proprietary system. For more information, refer to the article on the TMHP EVV website (PDF).
Resources
- Contact: Electronic_Visit_Verification@hhsc.state.tx.us
- Website: HHSC EVV Cures Act
Trainings Available:
EVV Policy Training (Provided by your payer)
- The HHSC EVV Policy computer-based training (CBT).
- The MCO Policy training. Contact your MCO for EVV Policy training opportunities.
EVV Aggregator and EVV Portal Training (Provided by TMHP)
There will also be instructor-led trainings (EVV Roadshow) in October. Find the schedule and register on the HHS Learning Portal.
Additional training resources are available on the HHSC EVV website and the TMHP EVV Provider Training webpage.
For questions about this alert, email Electronic_Visit_Verification@hhsc.state.tx.us.
Online, interactive EVV training courses are available
in the HHS Learning Portal and TMHP Learning Management System. Completing these courses help program providers meet EVV training requirements.
The HHS Learning Portal includes training about HHSC EVV Policy.
The TMHP Learning Management System includes training about:
- EVV Vendor Selection
- EVV Portal
- EVV Portal Standard Reports and Search Tools
- EVV Claims Submission and Billing
ICF/IID UPL Supplemental Payment Program FFY 2026 Enrollment Update
December 14th, 2025
ICF/IID UPL Supplemental Payment Program: Enrollment Portal Update
HHSC has updated the location of the enrollment portal for the federal fiscal year (FFY) 2026 Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) Upper Payment Limit (UPL) supplemental payment program.
Enrollment for the FFY 2026 program year opened on Dec. 1, 2025, and will remain open until 11:59 p.m. Dec. 31, 2025. Enrollment instructions can be downloaded from the portal.
To log in and enroll, enter your email address on the portal’s landing page, and a login code will be sent to you via email. If you do not receive a response email within a few minutes, reach out to Provider Finance Long-Term Services and Support for assistance.
December 7th, 2025
ICF/IID UPL Supplemental Payment Program
Enrollment for the federal fiscal year (FFY) 2026 Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) Upper Payment Limit (UPL) supplemental payment program opened on Dec. 1, 2025. The enrollment portal will remain open until 11:59 p.m. Dec. 31, 2025. Instructions are available for download in the portal.
Per Title 1 Texas Administrative Code, Section 355.458, non-state government-owned ICF/IID providers are eligible for this supplemental payment program. The eligibility list for FFY 2026 can be found on the ICF/IID UPL Supplemental Payment Program Website.
Questions regarding eligibility, enrollment, or the program calendar should be directed to Provider Finance Long-Term Services and Support.
April 12th, 2025
HHSC is providing notification of the Intergovernmental Transfer (IGT) call for the Intermediate Care Facilities Upper Payment Limit (ICF UPL) 2Qtr2025 payment.
The federal fiscal year 2025 ICF UPL Quarterly Payments file was updated on April 15, 2025, and can be found on the Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) UPL Supplemental Payment Program website. IGT amounts due are in Column J, under the “2nd Quarter Maximum IGT” heading.
Below are the pertinent dates associated with the 2025 ICF UPL 2nd Qtr. 2025 Payment:
- May 7, 2025: Last date to schedule transfer in TexNet.
- May 8, 2025: IGT Settlement Date.
- May 28, 2025: Payments expected to be released by the Comptroller.
Select the ICF UPL bucket in TexNet when you enter your IGT. Funds should be transferred through TexNet using the TexNet instructions. After transferring funds, send a screenshot or PDF copy of the confirmation or trace sheet from TexNet to the Provider Finance Department Payments Team.
ICF/IID Updates

December 11th, 2025
ICF Quarterly Webinar with HHSC LTCR
For ICF Providers, and will discuss the latest information from LTCR.
Those using Internet Explorer may have difficulties registering for the webinar. If so, try using another browser, such as Google Chrome or Microsoft Edge.
ICF Provider Webinar with LTCR
Jan. 14, 2026
2–3 p.m.
Email LTCR Policy to request agenda items or for questions related to this webinar.
November 15th, 2025
UPL (Upper Payment Limit) Supplemental Payment Program FFY 2026 Eligibility List Published
The HHSC Provider Finance Department has published the eligibility list for the federal fiscal year (FFY) 2026 Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) Upper Payment Limit (UPL) supplemental payment program on the program webpage.
Per Title 1 of the Texas Administrative Code, Section 355.458, non-state government-owned ICF/IID providers are eligible for this supplemental payment program.
Under this program, a participating non-state government entity would contribute the “state share” of the supplemental payment in the form of inter-governmental transfers (IGTs). The state will claim matching funds and will make a supplemental payment to the ICF/IID facility based on the supplemental amount calculated by the state and the IGT amount transferred by the entity.
Enrollment for the FFY 2026 program will open on Dec. 1, 2025, and will last for 30 days.
To increase transparency with the program we are sharing additional information to include a list of facilities we deemed eligible to participate in the voluntary program based on the eligibility criteria. This includes the eligibility list, which reflects which facilities are not eligible and which facilities are eligible. If a facility has a question related to our initial eligibility assessment, they can contact Provider Finance. “
FFY 2026 ICF UPL Supplemental Payment Program Eligibility List (.xlsx)
ICF/IID UPL Supplemental Payment Program FFY 2026 Eligibility List Published
The HHSC Provider Finance Department has published the eligibility list for the federal fiscal year (FFY) 2026 Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) Upper Payment Limit (UPL) supplemental payment program on the program webpage.
Per Title 1 of the Texas Administrative Code, Section 355.458, non-state government-owned ICF/IID providers are eligible for this supplemental payment program. Under this program, a participating non-state government entity would contribute the “state share” of the supplemental payment in the form of inter-governmental transfers (IGTs). The state will claim matching funds and will make a supplemental payment to the ICF/IID facility based on the supplemental amount calculated by the state and the IGT amount transferred by the entity.
Enrollment for the FFY 2026 program will open on Dec. 1, 2025, and will last for 30 days. HHSC will publish both a link to the enrollment portal and a GovDelivery alert when the enrollment period opens.
**HHSC will publish both a link to the enrollment portal and a GovDelivery alert when the enrollment period opens.
September 15th, 2025
Updated ICF/IID Services Payment Rates
HHSC has published updated fee schedules for Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) regarding the approved payment rates for services.
The HHSC Provider Finance Department (PFD) webpage has more information about the approved payment rates.
If you have further questions, email HHSC PFD, Long-term Services and Supports (LTSS), Center for Information and Training, or call us at (737) 867-7817.
June 26th, 2025
HHSC Publishes Revised Process for Reporting Incidents, Complaints and HHSC Investigations of Abuse, Neglect, and Exploitation (PL 2025-02) for ICF
HHSC Long-Term Care Regulation updated Provider Letter (PL) 2025-02 Process for Reporting Incidents, Complaints and HHSC Investigations of Abuse, Neglect, and Exploitation for Intermediate Care Facilities for Individuals with an Intellectual Disability (ICF/IID) to include the facility must report the alleged abuse, neglect, and exploitation (ANE) to HHSC Complaint and Incident Intake within one hour of suspecting or learning of the allegation. This includes instances in which the facility learns of the alleged ANE when the surveyor enters the ICF on the complaint investigation and informs the provider of the allegation. This PL replaces PL 2024-04.
For questions contact LTCRPolicy@hhs.texas.gov.
April 8th, 2025
April & May Trainings for ICF
Reporting Abuse, Neglect, Exploitation Changes and Self-Reporting Incidents for Intermediate Care Facilities
Wednesday, April 9
10 – 11 a.m.
Register here for the webinar.
Reporting Abuse, Neglect, Exploitation Changes and Self-Reporting Incidents for Intermediate Care Facilities
Thursday, May 22
2 – 3 p.m.
Register here for the webinar.
Hurricane Season – Ready or Not! Preparedness for Intermediate Care Facilities (ICF)
Wednesday, May 28
10 a.m. – noon
Register here for the webinar.
February 22nd, 2025
HHSC LTCR Updates Tag Crosswalks for Intermediate Care Facilities
LTCR has updated the ICF federal, licensure and state standards of participation tag crosswalks to the most current version.
Each crosswalk provides a detailed table that identifies the applicable tag numbers, title, Code of Federal Regulations and Texas Administrative Codes for providers to reference.
These documents are posted on the ICF Provider Portal HHSC website.
For questions, email LTCRPolicy@hhs.texas.gov.
November 13th, 2024
HHSC Rescinds PL 2024-20 Requirements for Tuberculosis Screening and Testing
HHSC rescinded PL 2024-20 Requirements for Tuberculosis Screening and Testing. Additional guidance regarding tuberculosis screening and testing will be forthcoming.
In the interim, providers should follow their program regulations and internal communicable disease and infection control policies and procedures to address tuberculosis screening and testing.
Providers may use recommendations from the Centers for Disease Control and the Texas Department of State Health Services to inform their policies.
For more information, follow the links below:
Frequently Asked Questions About TB | Texas DSHS
Tuberculosis Screening for Adults in Various Settings (PDF)
August 12th, 2024
PL 24-04 –Changes & Guidance To ICF/IID Provider Reporting Processes and HHSC Investigating Processes- Effective March 1, 2024.
As the ICF/IID rules to implement HB 4696 applies to the 6-13 bed facilities and is not yet adopted, yet the provisions in the bills became effective 9/1/2023. We are unclear if or how HHSC is monitoring for compliance as the only guidance released to date is PL 24-04 . And, this PL only addresses the provider reporting processes and HHSC investigating processes which became effective March 1, 2024. The PL does not provide guidance or address compliance related to the directives in the bill which, as of September 1, 2023, is now law.
In response to inquiries from providers and provider associations, HHSC has now stated that “at this time ICF/IID surveyors are surveying for compliance with the current regulations located in 26 TAC 551 and guidance issued in PL 2024-04.“
NOTE: HCS/TxHmL: It’s anticipated the rules to implement HB 1009 in HCS/TxHmL will be posted for ‘informal’ comment this fall. Rules to implement HB 4696 are postponed until after the 89th Session.
March 10th, 2024
ICF/IID ANE Webinar- Very Important!
Thursday, March 21
2–3:30 p.m.
Register here for webinar.
HHSC Long-term Care Regulation has published Provider Letter 2024-04 Revised (Replaces PL 17-02 and 17-03) Revised Process for Reporting and HHSC Investigations of Abuse, Neglect, and Exploitation for Intermediate Care Facilities for Individuals with an Intellectual Disability (ICF/IID). Don’t forget, as of March 1st, 2024, this replaces the previous ANE Reporting & Investigations process. Reporting is now done to (CII) Complaint & Incident Intake.
February 25th, 2024
New Reporting Process for ANE Reporting & Investigations for ICF/IID Program
HHSC has released a new letter of guidance regarding the revised ANE reporting process to CII and the ANE investigation process for ICF/IID. Here is the published provider letter (PL) 2024-04
Beginning March 1, 2024, reporting of investigations for allegations of abuse, neglect, and exploitation (ANE) for Medicaid consumers served by an Intermediate Care Facility for Intellectual and Developmental Disabilities (ICF/IDD) will transition from the Department of Family and Protective Services Statewide Intake (DFPS SWI) to HHSC Regulatory Services Complaint and Incident Intake (CII).
Additionally, processes related to investigations of ANE of ICF/IDD will change as of March 1, 2024.
For questions contact LTCRPolicy@hhs.texas.gov.
January 20th, 2024
Surrogate Decision-Making Program (SDMP)
Randy Rowley, Manager, SDMP, HHSC, provided an overview of the surrogate decision-making program to the workgroup. Click here for link to ppt
HHSC December 27, 2023 Bulletin:
The legislatively mandated Surrogate Decision-making Program (SDMP) authorizes Surrogate Consent Committees (SCCs), comprised of trained volunteers, to provide written informed consent for individuals residing in community-based ICFs/IID who have been assessed to lack the capacity to make certain treatment decisions for themselves and have no legal guardian or actively involved family members serving as Surrogate Decision Makers (SDMs) or the treatment decisions are beyond the scope of the SDMs.
The SDMP facilitates compliance with Code of Federal Regulations (CFR) Title 42 and state ICF/IID rules regarding protection of individuals rights.
For the list of treatment decisions that a SCC can make see the HHS SDMP webpage.
Watch for upcoming training event announcements.
For questions about SCCs, or if you want to volunteer to serve on a SCC, email SDMP Manager Randy Rowley or call 512-438-4306.
ICF Rules-TAC Code Draft Title 26 Part I Ch 551
Personal Needs Allowance Information Letter
Personal Needs Allowance (PNA): PNA of individuals residing in a nursing home or ICF/IID from $60/month to $75/month, and for couples from $120/month to $150/month effective January 1, 2024. HHSC posted an information letter regarding this change:
IL 2023-45 Personal Needs Allowance (PNA) Adjustment (Replaces IL 2022-16) (texas.gov).
June 15th, 2023
Personal Needs Allowance Increase Bill passed during 88th legislature session
December 15th, 2022
ICF Resources
These resources can also be found on the ICF Provider Portal page.
September 25th, 2022
HHSC Publishes Updated Guidance on the Amelioration of Administrative Penalties for ALF, ICF/IID, and NF Providers
HHSC Long-term Care Regulation has published Provider Letter 2022-24 – Amelioration of Administrative Penalties (replaces PL 2013-18).
The letter provides guidelines to assisted living facilities,
intermediate care facilities for individuals with an intellectual
disability or related conditions, and nursing facilities about
the amelioration of administrative penalties assessed for state licensure
violations.
Read the provider letter details.
June 12th, 2022
ICF COVID-19 Vaccination Reporting Emergency Rules Expired June 6!!
Emergency rules for Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions that require COVID-19 vaccination reporting expired June 6.
This means that effective June 7, ICFs no longer have to report COVID-19 vaccination data for staff and individuals to HHSC.
The following rules expired June 6:
- 26 TAC §551.48 – ICF/IID Provider COVID-19 Vaccination Data Reporting Requirement.
Here is a copy of the previous rule that expired:
551.48.ICF/IID Provider COVID-19 Vaccination Data Reporting Requirement.
(a) An intermediate care facility administrator and one additional designee must enroll in an emergency communication system in accordance with instructions from Texas Health and Human Services Commission (HHSC).
(b) An intermediate care facility must respond to requests for information received through the emergency communication system in the format established by HHSC.
(c) Within 24 hours of becoming aware of a staff or resident’s COVID-19 vaccination, an intermediate care facility must accurately report COVID-19 vaccination data for staff and individuals in the format established by HHSC.
(d) Subsection (c) of this section does not apply to state supported living centers.
The agency certifies that legal counsel has reviewed the emergency adoption and found it to be within the state agency’s legal authority to adopt.
Filed with the Office of the Secretary of State on August 10, 2021.
Email questions to LTCR Policy.
April 29th, 2022
ICF Visitation Rules Update
An alert went out to remind providers that all visitation must be allowed. Essential caregiver and end-of-life visits must be allowed for all individuals with any COVID-19 status. A facility may be cited if visitation is not allowed.
Review ICF/IID visitation rules from April 4th, 2022, for additional information.
April 10th, 2022
COVID-19 ICF Mitigation, Response Rule Revised Effective April 6
HHSC Long-term Care Regulation has published a revised Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions COVID-19 Mitigation and Response Emergency Rule. It is effective April 6, 2022.
The revised rule:
- Removes the requirements to have plans for obtaining and maintaining a two-week supply of full PPE.
- Clarifies that a facility does not have to provide the name of the person who tested positive for COVID-19 when reporting to CII.
April 10th, 2022
HHSC Publishes Description of Key Changes to 26 TAC 551, ICF/IID (PL 2022-07)
HHSC has published Provider Letter 2022-07, Description of Key Changes to 26 TAC 551, Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions, for ICF/IID providers. This letter describes the key changes to Title 26 of the Texas Administrative Code, Chapter 551, that were effective on Feb. 24.
Throughout the rule, HHSC updated citations, agency names, and terminology; corrected minor grammatical and punctuation errors; and revised sentence structures to make the chapter easier to read. In addition, the following items are addressed in this letter:
– New Requirements for Infection Prevention and Control Policies and Procedures
-HHSC included a state rule that refers to each Centers for Medicare & Medicaid Services (CMS) Condition of Participation (CoP). Additions to 26 TAC 551 include • Governing Body • Client Protections • Facility Staffing • Active Treatment • Client Behavior and Facility Practices • Health Care Services • Physical Environment • Emergency Preparedness • Dietetic Services.
– transition from paper applications to the use of the online licensure portal, called the Texas Unified Licensure Information Portal (TULIP) (Disclose information when applying for “relocation” and application information must be submitted through portal in “TULIP” system)
-Now require evaluation of the emergency preparedness and response plan at least every two years, instead of annually.
-ANE & Incident definitions
-Administrative penalties for each visit are limited to the cap amount, regardless of the number or duration of violations as of Sept. 1st, 2021
****If you have any questions about this letter, please contact the Policy and Rules Section by email at LTCRPolicy@hhs.texas.gov or call (512) 438-3161
April 6th, 2022
COVID Screening in ICF’s
ICF COVID-19 Mitigation and Provider Response emergency rules require an intermediate care facility must screen individuals according to HHSC guidance
.ICFs must screen individuals:
•upon admission or readmission to the facility; and
•at least once a day.
ICFs must screen each employee or contractor for the following criteria (listed below) before entering the facility at the start of their shift.
•Staff screenings must be documented in a log kept at the facility entrance and must include the name of each person screened, the date and time of the evaluation, and the results of the evaluation.
**Staff who meet any of the criteria must not be permitted to enter the facility.
As per ICF/IID Expansion of Reopening Visitation Emergency rules, ICFs are required to screen all visitors for signs or symptoms of COVID-19.
*Visitor screenings must be documented in a log kept at the entrance to the facility, which must include the name of each person screened, the date and time of the screening, and the results of the screening. The visitor screening log may contain protected health information and must be protected in accordance with applicable state and federal law .
*A visitor may not participate in a visit if the visitor has signs and symptoms of COVID-19 or active COVID-19 infection.
Screening Criteria:
•fever, defined as a temperature of 100.4 Fahrenheit and above, or
signs or symptoms of a respiratory infection, such as cough, shortness of breath, or sore throat;
•other signs or symptoms of COVID-19, including
-chills,
-new or worsening cough,
-shortness of breath or difficulty breathing,
-fatigue,
-muscle or body aches,
-headache,
-new loss of taste or smell,
-sore throat,
-congestion or runny nose,
-nausea or vomiting,
-or diarrhea;
•any other signs and symptoms as outlined by the CDC in Symptoms or Coronavirus at cdc.gov;
•contact in the last 14 days with someone who has a confirmed diagnosis of COVID-19, is under investigation for COVID-19, or is ill with a respiratory illness, regardless of whether the person is fully vaccinated, unless the person is entering the facility to provide critical assistance; or
•testing positive for COVID-19 in the last 10 days.
April 6th, 2022
Reporting Confirmed Case of COVID-19 in ICF/IID
A facility must notify the Texas Health and Human Services Commission (HHSC) Complaint and Incident Intake of COVID-19 activity as described below.
(1) A facility must notify HHSC of the first confirmed case of COVID-19 in staff or individuals, and the first confirmed case of COVID-19 after a facility has been without cases for 14 days or more, at HHSC Complaint and Incident Intake (CII) through TULIP, or by calling 1-800-458-9858, within 24 hours of the positive confirmation.
(2) A facility must submit a Form 3613-A Provider Investigation Report, minus the name of the person who tested positive for COVID-19, to HHSC Complaint and Incident Intake, through TULIP, by email at ciiprovider@hhs.texas.gov, or by fax at 877-438-5827, within five working days from the day a confirmed case is reported to CII.
April 6th, 2022
COVID-19 Mitigation and Response Emergency Rule Updated
HHSC Long-term Care Regulation has published a revised Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions COVID-19 Mitigation and Response Emergency Rule.
It became effective April 6, 2022.
The revised rule:
•Points to guidance from the Texas Department of State Health Services and HHSC rather than the CDC.
•Removes the requirements to have plans for obtaining and maintaining a two-week supply of full PPE.
•Removes the requirement to have spaces to don and doff PPE
•Clarifies that a facility does not have to provide the name of the person who tested positive for COVID-19 when reporting to CII.
February 27th, 2022
HHSC Adopts Revised ICF/IID Rules – Effective Feb. 24th, 2022
HHSC Long-term Care Regulation has adopted updates to the Intermediate Care Facilities for Individuals with an Intellectual Disability (ICF/IID) or Related Conditions program rules. The revised rules are in the Texas Administrative Code Title 26, Chapter 551. They are effective Feb. 24, 2022.
Key changes to the rule are to:
- Implement House Bill 1848 from the 86th Legislature, Regular Session, 2019 which requires new infection control policies and procedures in long-term living facilities.
- Implement House Bill 3720 from the 87th Legislature, Regular Session, 2021 which limits the total amount of an administrative penalty assessed against an ICF/IID.
- Reintegrate the conditions of participation from the Code of Federal Regulations.
- Corrects legacy agency terms, update rule citations, and edit for clarity and consistency.
COVID-19 ICF/IID Webinar Recording from Feb. 14 Available
A recording of the Feb. 14 Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions COVID-19 Q&A with HHSC Long-term Care Regulation and DSHS is available for those who could not attend.
There have been changes made to the PowerPoint based on the information provided by DSHS during the webinar.
Listen to the webinar recording.
Email LTCR Policy for the transcript.
February. 20th, 2022
Mar. 07 ICF COVID-19 Webinar with HHSC LTCR
Long-term Care Regulation and the Department of State Health Services will provide the latest information on the COVID-19 pandemic and take live questions from participants in this intermediate care facilities provider webinar.
Provider attendance is critical to staying current with COVID-19 requirements and guidance. ICF/IID providers are strongly encouraged to attend all COVID-19 webinars with LTCR and DSHS.
Those using Internet Explorer may have difficulties registering for the webinar. If so, try using another browser, such as Google Chrome or Microsoft Edge.
March 7, 2022
11 a.m.–12 p.m.
Register for the COVID-19 Webinar.
February 13th, 2022
HHSC is not currently assessing compliance with CMS’s Omnibus COVID-19 Health Care Staff Vaccination rules, published in the Federal Register on November 5, 2021.
ICF COVID-19 Vaccination Data Reporting and Emergency Communication System – Feb 7
HHSC Long-term Care Regulation has published a revised ICF/IID Provider COVID-19 Vaccination Data Reporting Rule (PDF). It became effective February 7, 2022 and includes Emergency Communication System Enrollment for Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions providers.
The rule requires ICF/IIDs to:
- Report COVID-19 vaccine data within 24 hours
- Enroll in an emergency communication system
January 7th, 2022
ICF COVID-19 Response Plan and FAQ Updated – Jan. 7
Document Version Date Change Comments
Version 3.5 1/5/2022 Changes to pages 6, 31, 38, 39, 40, 51, 72 71, and Changes made to reflect the most updated CDC guidance.
Version 3.4 12/07/2021 Changes to pages 15, 16, 25, 26, 31, 35 Edited to include revised ICF COVID-19 Provider Response Mitigation Rules for ICFs/IID
For changes made previous to 12/07/2021, please read the Table of Changes starting with page 7 of 19 of the Response Plan.
Update your Infection Control Policies and other related policies accordingly.
HHSC has revised the ICF COVID-19 Response Plan and Frequently Asked Questions document in response to the most recent CDC guidance.
November 21st, 2021
HHSC Publishes PL 2021-38 Medicaid Bed Reallocation
HHSC published Provider Letter 2021-38 Medicaid Bed Reallocation which explains the process to request reallocated ICF/IID Medicaid beds from HHSC. This letter replaces Provider Letter 2019-21.
November 4th, 2021
Updated ICF/IID COVID-19 FAQ and COVID-19 Response Plan Revised
HHSC has revised the Frequently Asked Questions for ICF/IIDs about COVID-19 (PDF) and the ICF/IID COVID-19 Response Plan (PDF) in response to the revised COVID-19 Expansion of Reopening Visitation for ICF Providers rules.
October 24th, 2021
New PL 2021-21 COVID-19 – Expansion of Reopening Visitation for ICF Providers
Super important!!!!
HHSC has published Provider Letter 2021-21, COVID-19 Response – Expansion of Reopening Visitation (PDF) for ICF/IID providers. This letter replaces Provider Letter 2021-10. This letter describes the criteria for expanded visitation as well as address changes in response to Executive Order No. GA-38(link is external) and updated CDC guidance.
Updated COVID-19 Expansion of Reopening Visitation Emergency Rules for ICF Providers
HHSC Long-term Care Regulation has published revised COVID-19 Expansion of Reopening Visitation Emergency Rules for Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICFs/IID) or Related Conditions (PDF). The rules address changes in response to Executive Order No. GA-38 (PDF)(link is external) and updated CDC guidance.The rules became effective on October 20, 2021.
September 15th, 2021
HHSC Publishes Amended Statutory Cap Regarding Administrative Penalties for ICFs: (PL 21-34)
HHSC published Provider Letter 21-34 Amended Statutory Cap Regarding Administrative Penalties for Intermediate Care Facilities. PL 21-34 notifies providers of changes to how HHSC determines and imposes administrative penalties based on changes made by House Bill 3720 (87th Legislature, Regular Session, 2021).
September 5th, 2021
Guidance for Providers Regarding Entry into LTC Facilities (PL 2021-33)
HHSC Long-term Care Regulation has published Provider Letter 2021-33, Authority to Enter Long-term Care Facilities (PDF), for ALF, HCS, ICF/IID and NF providers. This letter reminds providers that they must allow persons providing critical assistance and providers of essential services to enter the facility if they pass the facility’s COVID-19 screening.
September 5th, 2021
ICF/IID Leave During COVID-19 Rule Reinstated
HHSC has published IL 2021-42 ICF/IID Services During COVID-19 (PDF), which replaces IL 2020-43.
A resident must be discharged from the Intermediate Care Facility for Individuals with an Intellectual Disability or Related Conditions, with or without a contract to hold the resident’s placement in accordance with 26 TAC Section 261.227(j), if the resident is absent from the ICF/IID for one full day or more and the absence is not during leave described in 26 TAC Section 261.226.
August 1st, 2021
HHSC Publishes Updated COVID-19 Response Plan and Frequently Asked Questions for ICF Providers
HHSC Long-term Care Regulation updated the ICF COVID-19 Response Plan and FAQ document on July 29, 2021.
Read the updated ICF COVID-19 Response Plan (PDF).
Read the updated ICF FAQs (PDF).
March 24th, 2021
HHSC Adopts New Expansion of Reopening Visitation Emergency Rules for ICF Providers!!!
HHSC has adopted new Expansion of Reopening Visitation (PDF) emergency rules that establish criteria for expanded indoor and outdoor visitation as well as essential caregiver visits. These rules are effective March 24, 2021.
HHSC Publishes COVID-19 Response – Expansion of Reopening Visitation for ICF Providers (PL 2021-10)
HHSC has published Provider Letter 2021-10, COVID-19 Response – Expansion of Reopening Visitation (PDF) for ICF/IID providers. This letter replaces Provider Letter 2020-43. This letter describes the criteria for expanded indoor and outdoor visitation as well as essential caregiver visits.
March 22nd, 2021
ICF COVID-19 March 22 Webinar Recording Available
A recording of the March 22, 2021, ICF/IID COVID-19 Q&A with HHSC LTC Regulation and DSHS is available for those who could not attend.
Listen to the COVID-19 Q&A recording.
March 11th, 2021
Recording of ICF COVID-19 March 8 Provider Webinar Available
A recording of the March 8, 2021 ICF/IID COVID-19 Q&A with HHSC LTC Regulation and DSHS is available for those who could not attend.
Listen to the COVID-19 Q&A recording.
February 8th, 2021
Draft ICF/IID Rule Changes
- Draft ICF/IID Rule Changes- See link: https://documentcloud.adobe.com/link/track?uri=urn:aaid:scds:US:cf5ea154-04b4-4c75-8aec-7e230c3cfda0
- High Level Summary of Proposed Changes See link: https://documentcloud.adobe.com/link/track?uri=urn:aaid:scds:US:2aa689d6-3018-4ab9-8d75-04578f4c922d
February 7th, 2021
Feb. 8- ICF/IID Provider Bed Hold Payments Webinar &
Reminder to Provide Letter to Families
IL 2020-43, ICF/IID Services During COVID-19 directed program providers to give a copy of the letter attached to that IL to each resident who was:
- Absent from an ICF/IID
- Not on leave
- Was not discharged from the ICF/IID
If you have not provided the letter to residents who meet that criteria, do so immediately. It was to be complete by Oct. 5, 2020. You must assist residents in deciding to do only one of the following:
- Return to the facility.
- Continue to be absent from the facility, be discharged, but enter into an agreement with the ICF/IID to hold your place at the facility.
- Continue to be absent from the facility and be discharged.
HHSC Medicaid and CHIP Services will issue instructions to providers about entering COVID-19 therapeutic leave for days a resident was away from an ICF/IID to reduce the risk of COVID-19 transmission. Register for the following webinar to review the emergency rules authorizing this leave and the instructions for entering it.
ICF/IID Provider Bed Hold Payments Webinar
Friday, Feb. 5
9:30-11 a.m.
Register for the Bed Hold Payment Webinar.
The emergency rule authorizing payment for COVID-19 therapeutic leave (PDF) is effective Jan. 29, 2021.
January 19th, 2021
HHSC Updates the ICF COVID-19 Response Plan and FAQ Document
Please be sure to update your infection control and other related policies based on the updated Response Plan!!!
Let us know if we can help. We will be working on some of these addendums in the next few weeks.
HHSC Long-term Care Regulation updated the ICF COVID-19 Response Plan and FAQ document on Jan. 12, 2021.
Read the updated ICF COVID-19 Response Plan (PDF).
Read the updated ICF FAQs (PDF).
Jan. 25 ICF Provider COVID-19 Webinar with HHSC LTC Regulation
Long-term Care Regulation and the Department of State Health Services provide the latest information on the COVID-19 pandemic and take live questions from participants in this ICF provider webinar. Provider attendance is critical to staying current with COVID-19 requirements and guidance.
ICF/IID providers are strongly encouraged to attend this and all biweekly COVID-19 webinars with LTCR and DSHS.
Those using Internet Explorer may have difficulties registering for the webinar. Please try another browser such as Google Chrome or Microsoft Edge.
ICF Provider Webinar
Jan. 25, 2021
11 a.m. – 12:30 p.m.
Register for the COVID-19 Webinar.
Recording of ICF COVID-19 Jan. 11 Provider Webinar Available
A recording of the January 11, 2021 ICF/IID COVID-19 Q&A with HHSC LTC Regulation and DSHS is available for those who could not attend.
Listen to the COVID-19 Q&A recording.
January 10th, 2021
Informal Comments on Draft Rules for ICF/IID or Related Conditions
HHSC is accepting informal comments from stakeholders on the following draft rules, which are now posted on the HHS Rulemaking page. The comment period ends Jan. 19, 2021.
This project implements two bills from the 86th Legislature, Regular Session, 2019. House Bill (H.B.) 1848 contains required elements for infection prevention and control. H.B. 3803 limits the daily amount of an administrative penalty assessed against an ICF/IID. The project will also update rule references and agency names, amend rules to align with Centers for Medicare & Medicaid Services conditions of participation in the ICF/IID program, and edit the rules for clarity and consistency.
HHSC Publishes Revised Reporting Guidance for Long-Term Care Providers
(PL 20-37)
HHSC has published a revised version of Provider Letter 20-37, Reporting Guidance for Long-Term Care Providers (PDF). The revision includes information for ALF and ICF providers offering point-of-care testing for COVID-19 and clarifies reporting requirements for NF providers.
November 22nd, 2020
November 30 ICF Provider COVID-19 Webinar with HHSC LTC Regulation
LTCR and DSHS provide the latest information on the COVID-19 pandemic and take live questions from participants in this ICF provider webinar. Provider attendance is critical to staying current with COVID-19 requirements and guidance.
ICF/IID providers are strongly encouraged to attend this and all biweekly COVID-19 webinars with HHSC Long-term Care Regulation and the Department of State Health Services.
Those using Internet Explorer may have difficulties registering for the webinar. Please try another browser such as Google Chrome or Microsoft Edge.
ICF Provider Webinar
November 30, 2020
11 a.m. – 12:30 p.m.
Register for the COVID-19 webinar.
Recording of November 16 ICF COVID-19 Q&A Provider Webinar Available
A recording of the November 16, 2020 ICF/IID COVID-19 Q&A with HHSC LTC Regulation and DSHS is available for those who could not attend.
View the COVID-19 Q&A recording.
10/16/20
Important Information!
LTCR FORM 2195: Expansion of Reopening Visitation Status Attestation and Letter PL 20-43 (for ICF Only)
Note: to receive an approved general visitation designation, a small ICF/IID that cannot provide separate areas, units, wings, halls, or buildings for individuals who are COVID-19 positive, COVID-19 negative or unknown COVID-19 status, based on the status of the entire facility, must:
- have no facility-acquired COVID-19 cases in individuals for at least 14 consecutive days; and
- have no COVID-19 cases in staff.
An ICF/IID must provide instructional signage throughout the facility and proper visitor education regarding
- signs and symptoms of COVID-19;
- infection control precautions; and
- other applicable facility practices (e.g., the use of facemasks or other appropriate PPE, specified entries and exits, routes to designated visitation areas, and hand hygiene).
An ICF/IID that does not meet the criteria for a visitation designation must permit closed window visits and end-of-life visits for individuals regardless of their COVID-19 status, as well as essential caregiver visits for individuals with COVID-19 negative or unknown COVID-19 status.
Such an ICF/IID must also develop and implement a plan to meet the visitation criteria and submit the plan to the regional director in the Long-term Care Regulation (LTCR) region where the ICF/IID is located within five days of submitting the new 2195 Expansion of Reopening Visitation Status Attestation Form,
or
within five days of receiving notification from HHSC that the ICF/IID was not approved for general visitation designation.
LTCR Form 2195
Each ICF/IID must submit LTCR Form 2195 to the Regional Director in the LTCR region where the facility is located and must provide information about whether the ICF/IID meets or does not meet the criteria for expanded general visitation.
Each ICF/IID must submit a completed form 2195 to the Regional Director no later than October 31, 2020.
An ICF/IID that does not meet the visitation designation criteria must attest that it:
- is permitting closed window visits, end of life visits, and essential caregiver visits;
- will develop and implement a plan to meet the visitation designation criteria as defined in 26 TAC §551.47; and
- has included the plan with the form or will submit the plan within five business days of submitting the form.
To seek a designation for general visitation, an ICF/IID must complete LTCR Form 2195, Expansion of Reopening Visitation Status Attestation, to notify LTCR that the ICF/IID seeks a designation as a visitation facility.
The form must be emailed to the LTCR regional director in the LTCR region where the facility is located. Any applicable pictures and facility maps must also be included with LTCR Form 2195.
The LTCR regional director or designee will review the form within three working days of submission and notify the ICF/IID whether it has received been approved for a visitation designation.
An ICF/IID with previous approval for visitation does not have to submit LTCR Form 2195 or other documentation unless the previous visitation approval has been withdrawn, rescinded, or canceled, or was for only indoor or outdoor visitation instead of both indoor and outdoor visitation.
If approved, the ICF/IID must allow outdoor visits, indoor plexiglass visits, open window visits, and vehicle parades in accordance with the applicable emergency rule. HHSC LTCR can conduct an on-site visit to confirm an ICF/IID’s compliance with the requirements. If HHSC determines that the ICF/IID does not meet the requirements for the designation as a visitation facility, the ICF/IID must immediately stop all visitation except a closed window visit, end-of-life visit, and visits by persons providing critical assistance, including designated essential caregivers.
If, at any time after a visitation designation is approved by HHSC, the ICF/IID experiences an outbreak of COVID-19, the ICF/IID must notify the Regional Director in the LTCR Region where it is located that the ICF/IID no longer meets visitation criteria, and the ICF/IID must immediately stop all visitation, except a closed window visit, end-of-life visit, or visits by persons providing critical assistance, including essential caregivers.
The ICF/IID can submit a new request for designation when it meets all visitation criteria.
Under Section 37.10 of the Texas Penal Code, a person commits a criminal offense if he or she makes a false entry in a governmental record; makes, presents, or uses any record or document with knowledge of its falsity and intent that it be taken as a genuine governmental record; or makes, presents, or uses a governmental record with knowledge of its falsity. In addition, making a false statement on the attestation form can result in the imposition of an administrative penalty as described in Texas Health and Safety Code, Chapter 252, section 252.065(a)
Contact Information for Submitting LTCR Form 2195 to the LTCR Regional Director: https://hhs.texas.gov/about-hhs/find-us/long-term-care-regulatory-regional-contact-numbers
If you have any questions about this letter, please contact the Policy, Rules and Training Section by email at PolicyRulesTraining@hhsc.state.tx.us or call (512) 438-3161.
10/05/20
Deadline for Decision To Return to Facility/Payment to Hold Bed/Discharge Option
Information Letter No. 20-43 ICF/IID Services During COVID-19
10/03/20
Quick TIPS on New Changes for Expansion of Facility Visitation Rules & Other Policies Concerning COVID-19
Essential Caregiver Visits and Salon Services Visitor (Visitor types above and beyond normal designated visiting facility type)
Essential Caregivers are allowed even if the facility does not have designated visitation. They must be at least 18 years of age. Can be family, friend, guardian.
- 1.They must wear a facemask. 2. They must have evidence of negative COVID-19 test in the past 14 days and must be screened by facility staff prior to the visit. (Pay attention to the new additional symptoms and discontinuation of asking about international travel). 3. There is a 2- hr limit unless the facility allows a longer period of time. 4.They can have physical contact with their individual (and only their individual) 5.They must be limited to access to their person. 6.An assigned person must escort them to and from the location they are going to meet with the individual- room, outside… 7. The facility must approve the face mask they are going to wear or provide an appropriate mask. 8.If they do not have an appropriate face mask or the facility can’t provide one, they will need to reschedule the visit. 9. The facility must create an identifying badge for the essential caregiver or any salon service visitors. 10. The facility must have attestation stating the essential caregiver has visited and when they left (include time arrived, when they left, who they visited). 11. Essential caregivers must be trained on PPE and how to wear PPE, handwashing, and other infection control practices and there must be proof of this training that the facility maintains. 12..The individual must be COVID-19 negative to have an Essential caregiver visit or Salon Service Visitor.
- ***(If client status is unknown, the essential visitor would have to wear a face mask (not N-95, save that for your staff who need to work with COVID-19 + individuals), gown, gloves, goggles or face shield, so the facility might need to provide these other items)
Phase I Visitation Rules, no longer in effect!
Expanded Visitation Rules now in effect: The facility must apply with form 2194 for the Designated Visitation Facility, do not require all these same requirements an essential visitor (or Salon Service Visitors)- Designated visits include: open window visits, closed window visits, parade visits (open window or closed) outside visits, (and in plexiglass separate areas). Must use physical distance, visitor screening, individual will wear face mask or face covering if tolerated and the same for the visitor -they must wear a face mask or face covering. Provider Letter 20-38 has the link with form 2194 at the end of it. We encourage you to email the form. Most staff at HHSC are not in the office Visitation Designation department has 3 days to approve or deny the 2194 form request. Only the administrator or director can fill out form 2194!!
Previous Level 1 Attestation Approval: If you previously submitted the 2192 and received approval, you do not need to request a new one with form 2194, if your status is the same. If you want to change the visitation type, then you will need a new form. ( i.e. you did not want plexiglass partition previously and now you do.)
Small facilities must request visitation designation for the whole facility (unless you have a way to separate all cohort areas completely.) Do not fill out section #3. That is only for NF’s.
The provider must develop and must enforce policies and procedures including testing strategies for Essential Visitors, in addition to the testing that must occur at least 14 days prior to 1st visit and all other polices related, such as essential visitor requirements discussed above. Remember your testing strategies are required to provide expectations for the essential visitor for how often they will be required to test and when, for any visits they are making, after the initial “essential caregiver visit”.
For vehicle parades, the individual needs to remain 10 ft or more from the vehicle for safety.
Plexiglass booths on the inside must be approved by a life safety person for your region. Send in pictures. Does have to be a plexiglass barrier, does not have to be 2 and 3 sided.
**Closed window and End of Life visits are the only visits an individual may have if they are COVID-19 + (positive)
Remember staff should be assigned to an appropriate cohort (COVID-19 +, COVID-19 Negative or Unknown) then they should stay with that Cohort. In addition, there should be a policy at the facility for limiting the sharing of staff. If you need help with your policy concerning “COHORTS” and ” Mitigation of COVID-19 by Limiting Sharing of Staff”, please contact us. I do have some policies you can purchase if needed. Please contact me at: info@twogetherconsulting.com
FAQ’s (June 2020)
Answer: Regulations regarding ICF/IID discharge have not been waived. A discharge, even on a temporary emergency basis, requires that key developmental, behavioral, social, health and nutritional information be shared with the accepting facility in the community or non-facility provider. CMS is aware that staffing shortages and/or client surges due to the PHE create a high demand on available staff time that makes it difficult to complete a full discharge summary for each client. Each ICF will need to evaluate what amount and detail of documentation is necessary to ensure that critical health information is shared with the accepting facility or other provider. When available and if appropriate, the Interdisciplinary Team (IDT) should maximize the use of telehealth for the completion of a client’s discharge plan during the PHE.
Answer: Yes. CMS has temporarily waived certain regulatory requirements providing flexibilities to assist RHCs and FQHCs in furnishing services during the COVID-19 PHE. This includes temporarily modifying the following:(a)50% mid-level staffing requirement for RHCs;(b)Physician supervision requirement for nurse practitioners (NPs), to the extent permitted by State law; and(c)Location requirements for existing RHCs and FQHC to allow additions of temporary service locations.Please see https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf for additional waiver information. Additional flexibilities, including guidance for RHCs and FQHCs furnishing telehealth services during the PHE, are also described in this CMS MLN Article: https://www.cms.gov/files/document/se20016.pdf
Answer: Yes. During the COVID-19 PHE, CMS is allowing currently approved RHCs/FQHCs to provide patient care services in temporary expansion sites to help address the urgent need for supplementary care. These temporary sites are not restricted to the rural/shortage area location requirements. Each location is obligated to follow RHC/FQHC regulations to the extent not waived. Therefore, the RHC/FQHC may provide services provided at a temporary location under the CMS Certification Number (CCN) for the permanent location. The RHC/FQHC is expected to be operating in a manner not inconsistent with its state’s emergency preparedness plan. Note: FQHCs must also have an updated Health Resource and Service Administration (HRSA) Notice of Award, expanding the scope of service to include the temporary location(s) to support response to the COVID-19 PHE.
My RHC participates in Medicare through one of the two CMS-approved RHC Accreditation Organizations (AOs). Do waivers of CMS regulations apply to CMS-approved accrediting programs? Do I need to notify the AO of my desire to temporarily add a service location during the COVID-19 PHE?
Answer: To assist RHCs and FQHCs in furnishing service during the COVID-19 PHE, CMS has provided additional flexibilities related to billing for services. These temporary flexibilities currently include Expansion of Virtual Communication Services for RHCs and FQHCs to include online digital evaluation and management services using patient portals, and Revision of Home Health Agency Shortage Area Requirement for Visiting Nursing Services Furnished by RHCs and FQHCs. Please see the Medicare FFS Billing FAQ document available at https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf. Please see Section II.L of the Interim Final Rule with Comment Period, “Medicare and Expanded Flexibilities for Rural Health Clinics (RHCs) Medicaid Programs; Policy and Federally Qualified Health Centers (FQHCs) During Regulatory Revisions in Response to the COVID-–19 Public Health Emergency (PHE)”(85 FR 19230, 19253), available at https://www.federalregister.gov/documents/2020/04/06/2020-06990/medicare-and-medicaid-programs-policy-and-regulatory-revisions-in-response-to-the-covid-19-public, for more information on regulatory changes for RHCs and FQHCs.
Webinar info: How to prevent infectious diseases and the spread of infectious diseases in ICF-Specifically COVID-19 (May 27th, 2020)
See the following pdf link from HHSC
https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/providers/long-term-care/icfiid-covid-updates-qa-webinar-may-27-2020.pdf
 Survey Operations Resume as of June 15th, 2020
Survey Operations Resume as of June 15th, 2020
 Providers Must Log Residents’ Leave
Providers Must Log Residents’ Leave
All community-based ICF/IID program providers must submit an absence request in the TMHP ICF/IID Online Portal for a resident away from the facility for one or more full days. See the TMHP ICF/IID Online Portal User Guide (PDF) starting on page 52 for more information. The program provider must submit a return request within three days after a resident returns to the facility. See page 58 of the Online Portal User Guide for an explanation.
Please ensure that information entered in the portal for absences is current. HHSC uses the information to determine how many residents are absent from their facilities and the length of those absences.
PolicyRulesTraining@hhsc.state.tx.us or call (512) 438-3161.
Provider Joint Training Opportunities
Check out Joint Provider Trainings link from HHSC, for more info:
https://apps.hhs.texas.gov/providers/training/jointtraining.cfm#course_112
Survey Process for ICF Has Changed: Please Be Aware
You may check your SOMA (Surveyor’s Operational Manual for ICF in Appendix J) for these changes.
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_j_intermcare.pdf
http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R178SOMA.pdf
Appendix Q of SOMA (Immediate Jeopardy) Changes
CMS clarifications letter
SOMA appendix Q Section Immediate Jeopardy
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_q_immedjeopardy.pdf
|
LON & Facility Size |
Current Rates |
Proposed Rates |
|
SMALL |
|
|
|
LON 1 |
$144.25 |
$150.31 |
|
LON 5 |
$160.74 |
$167.90 |
|
LON 8 |
$182.82 |
$191.85 |
|
LON 6 |
$223.88 |
$236.59 |
|
LON 9 |
$406.11 |
N/C |
|
MEDIUM |
|
|
|
LON 1 |
$118.04 |
$123.14 |
|
LON 5 |
$134.06 |
$140.24 |
|
LON 8 |
$158.90 |
$166.92 |
|
LON 6 |
$190.24 |
$200.79 |
|
LON 9 |
$385.84 |
N/C |
|
LARGE |
|
|
|
LON 1 |
$112.09 |
$116.30 |
|
LON 5 |
$119.64 |
$124.64 |
|
LON 8 |
$133.22 |
$139.44 |
|
LON 6 |
$179.40 |
$188.96 |
|
LON 9 |
$387.25 |
N/C |
STEPS Replacing STAIRS In Early 2026
December 7th, 2025
STEPS Replacing STAIRS -December Update
Starting in early 2026, HHSC will transition to a new web-based software application to collect information from providers for Medicaid and non-Medicaid cost reports, Supplemental and Directed Payment Program enrollments, and legislatively directed reports. The new system, the State of Texas Electronic Provider System (STEPS), will update and simplify the reporting and directed payment program enrollment processes. The current system, the State of Texas Automated Information Reporting System (STAIRS), will remain in use until the transition is complete.
STEPS Provider Webinar
The HHSC Provider Finance Department (PFD) will host a webinar about the STEPS system on Dec. 10, 2025, from 10 a.m. to 11:30 a.m. CST.
Register for the webinar here through GoToWebinar.
Webinar ID 641-739-747
STEPS Resources
- STEPS Webpage
The STEPS webpage is the central location for major announcements and resources. Updates regarding STEPS will be posted regularly before the system goes live.
- Frequently Asked Questions (FAQ)
The STEPS webpage includes an FAQ document to address your questions. This document is updated in response to questions received through the online portal referenced below.
- STEPS Transition Guides – Updated Dec. 1
The STEPS webpage includes transition guides that provide more details regarding access to the new STEPS system, training, and other related topics. New guides will be added as information is available.
- PFD Cost Report Webpages
The PFD Cost Report Information and PFD Cost Report Training webpages have been updated with new information about STEPS, cost report cycles, and cost report training requirements.
Questions?
HHSC encourages providers to submit additional questions not answered in the FAQ and transition guides through the online questions and feedback portal. These questions will not receive a direct response, but they will help guide future updates.
October 6th, 2025
October Update
HHSC will switch to a new web-based software application that will be used to collect information from providers for Medicaid and non-Medicaid cost reports, Supplemental and Directed Payment Program enrollments, and legislatively directed reports, starting in early 2026. The new system, State of Texas Electronic Provider System (STEPS), will update and simplify the reporting and directed payment program enrollment processes. The current system, the State of Texas Automated Information Reporting System (STAIRS), will remain in use until the transition is complete.
Resources
- STEPS Webpage
- The STEPS webpage will serve as a central location for major announcements and resources.
- Updates regarding STEPS will be posted regularly before the system goes live.
- Frequently Asked Questions (FAQ)
- The STEPS webpage includes an FAQ document to address your anticipated questions. This document has been updated in response to questions received through the online portal referenced below.
Questions
HHSC encourages providers to submit additional questions not answered in the FAQ through the online questions and feedback portal. These questions will not receive a direct response but will help guide updates to the FAQ.
Form 8578 (Intellectual Disability or Related Conditions) IDRC Assessment Update- Effective Nov. 14, 2025
December 4th, 2025
Very Important: IDRC Form Updated
Form used for: HCS/TxHml/ICF/CLASS/DBMD
Form 8578 Intellectual Disability or Related Conditions Assessment and Instructions Update:
An update to Form 8578 Intellectual Disability or Related Conditions Assessment and Instructions is now available.
The effective date for the form and form instructions is the date of publication, Nov. 14, 2025.
LTCR Provider Webinar Training
December 4th, 2025
December 2025 LTCR Provider Webinar Training Opportunities
Home and Community-Based Services and Texas Home Living Provider (HCS/TxHmL) Joint Training Webinars
Plan of Removal for HCS/TxHmL Providers
Tuesday, Dec. 16
2–3:30 p.m.
Register here for the webinar.
Medication Management for HCS/TxHmL Providers
Monday, Dec. 22
1:30–3 p.m.
Register here for the webinar.
For more training opportunities, visit the Joint Training Course Catalog.
National Influenza Vaccination Week 2025-Digital Toolkit
December 3rd, 2025
The Texas Department of State Health Services (DSHS) Immunization Section has announced the release of the National Influenza Vaccination Week (NIVW) 2025 Digital Toolkit.
NIVW takes place each December and highlights the importance of flu vaccination during influenza season. This week-long observance reinforces that it is not too late for Texans to receive a flu vaccine and protect themselves, their families, and their communities.
The NIVW 2025 Digital Toolkit provides communication materials to support your outreach efforts from December 1–5, 2025, including:
- Key flu vaccination messages
- Daily themes and talking points
- Social media copy
- Printable posters and flyers
- Fact sheets and educational resources
We encourage you to share these resources through your websites, social media platforms, newsletters, clinics, schools, and community channels throughout NIVW and the flu season.
You may access the complete toolkit on the DSHS website at Order Publications | Texas DSHS.
If you have questions or need additional support, please contact the Immunization Section at immunization.info@dshs.texas.gov.
Dates Twogether Consulting Will Be Closed During The Holiday Season
November 18th, 2025
Holiday Season Availability:
Twogether Consulting will be closed from November 25th, 2025-November 30th, 2025.
We will be closed from December 17th, 2025-January 4th, 2026.
You may email of course, and we will be checking it periodically, but we will not be taking on any new client projects or assignments these days, as no one will be available in the office. If you already have scheduled dates and projects with us during that time, we will still be providing those services. We do have other consultants that may be available during those times to refer out to, so please email us at info@twogetherconsulting.com or my regular email address for those of you who already have it.
Tips Concerning Survey Expectations For HCS Providers
November 16th, 2025
HCS providers have been contacting Twogether Consulting about certain requirements and/or changes in what surveyors are asking for this year from HCS providers. Below are a few things you should make sure you have completed and/or corrected prior to your survey. I will try to update this as we receive feedback from providers, provider associations, and even HHSC staff.
Here are some areas surveyors are focusing on:
-
- Smoke detectors: must be in working order and have working batteries, and they need to have appropriate placement inside each bedroom and “immediately” outside of the bedrooms
- (This last part is subject to interpretation, but to be safe we would recommend you have a smoke detector just outside of each bedroom, even if they are in the same hallway)
- This goes for Host Homes and Group Homes
- In some cases, surveyors have asked providers for their “smoke detector” policy, but I am assuming this is due to the fact that batteries were not being replaced regularly..
- We advise making this part of a regular inspection process of the home or scheduling your direct care staff in the home to inspect 1 x a month/qtr, or perhaps if you have maintenance staff or residential/house managers, this might be a part of their responsibilities.
- (This last part is subject to interpretation, but to be safe we would recommend you have a smoke detector just outside of each bedroom, even if they are in the same hallway)
- Emergency evacuation plans, policies, and training
- Provider must have a current and appropriately updated ER/EVAC Plan. Review and revise at least annually
- ER/EVAC policy and procedures
- Evidence of training on ER/EVAC plans to staff
- Posting of exit routes/egresses
- Fire drills:
- Must be completed quarterly for both Group Home and Host Home
- Group Homes: (1 per shift, per qtr/Q 90 days)
- Host Homes: (quarterly). At least 2 of which must be overnight/when individuals are asleep.
- Documentation: For each drill, the facility must maintain a record that includes the date, time, and the name of the staff member who conducted the drill. Copies must be maintained in the home.
- Reporting: Providers must complete and maintain the HHSC Fire Drill Report form (4719) for each drill. Please be sure you are using this form.
- Availability: Records must be provided to HHSC surveyors upon request
- Staff training:
- New staff must participate in a fire drill within 90 days of being hired.
- Staff must participate in a fire drill at least once per year.
- The provider must ensure staff can explain the emergency plan for the residence.
- If a staff member does not follow the emergency plan during a drill, they must receive additional training
- Must be completed quarterly for both Group Home and Host Home
- Registering with the new emergency communication tool-AlertMedia ( This also applies to providers of ICF/IID,TxHmL, HCSSAs and DAHS which includes ISS)
- Matresses
- In the Group Home or Host Home
- Must have a mattress cover
- mattress must not be on the floor (needs to be on bed frame)
- Any modification (a reason for not having the mattress cover or having an individual sleeping on a matress on the floor) must be discussed with SPT, approved by SPT, and written into the PDP
- Adaptive Aids
- Are the individuals’ AA’s in the home of the individual requiring them?
- Are AA’s in working order?
- Has the individual and/or all appropriate staff received training on the AA?
- Is there evidence of this training with signatures and inservice sheet or material for any staff trained?
- Have they been replaced if the equipment is broken/not working anymore and did you document when that was replaced?
- Ensuring that Group Homes have working equipment for taking vitals signs (blood pressure devices, digital thermometer or other device for temps, pulse oximeters for SAO2’s, etc.. specifically for persons with these “special needs” requiring for them to have regular vitals taken (blood pressure, temperature, oxygen saturation levels, etc.
- If you do have someone in the home requiring regular vital checks it might be a good idea to have staff check the equipment regularly (monthly/quarterly) to ensure the items are in the home, working and have working batteries is necessary
- Smoke detectors: must be in working order and have working batteries, and they need to have appropriate placement inside each bedroom and “immediately” outside of the bedrooms
Note: Enforcement and Survey are 2 different departments. Enforcement applies the administrative penalties based on scope and severity of the violation.
In addition, please be sure to appeal any violations you do not agree with, including the severity (critical vs non-critical), immediately upon receiving your final report. You only have 10 days from receiving your final report/ statement of deficiencies to request an informal dispute resolution (IDR). If you need help with your IDR or Plans of Correction (POC’s), please contact us at: info@twogetherconsulting.com. We have resources, contractors, and other consultants who can help you.
IDD-PASRR Handbook: Revision 25-1
November 16th, 2025
The IDD Preadmission Screening and Resident Review (IDD-PASRR) Handbook, revision 25-1, updates the handbook.
This revision is effective Nov. 12, 2025. Review the updates linked here.
CLASS and DBMD Quarterly Webinar on December 17th, 2025
November 16th, 2025
HHSC will be providing ongoing opportunities for CLASS and DBMD providers and FMSAs to hear about recent program updates.
CLASS and DBMD Quarterly Webinar
December 17, 2025
10 a.m. – 11:30 a.m.
Topics discussed will include:
- CLASS – Training Module Updates, Adding AA to an IPC
- DBMD – Region 1 Update, SPT meetings
- PES – Submission standards for ID/RCs, IPC Pre and Enrollment Packets
- Fair Hearings – The appeals process with a loss of financial eligibility
- HCS – Crisis Diversion and NF Diversion process
- EVV – Updates
- CAPM – New PM webpage and monitoring documentation
Register here for the webinar.
Run a test of your computer’s connectivity if you have never attended a webinar from your computer. You can run this test at any time before the date of the webinar. Perform this test early to allow time to address any technical issues.
Email questions to:
CLASSPolicy@hhs.texas.gov and DBMDPolicy@hhs.texas.gov
February 28th, 2025
HHSC will be providing ongoing opportunities for CLASS and DBMD providers and FMSAs to hear about recent program updates.
CLASS and DBMD Quarterly Webinar
March 19, 2025 10–11:30 a.m.
Topics to be discussed will include:
- CLASS/DBMD — Upcoming form updates, June webinar.
- UR/PES — UR/PES responsibility changes.
- EVV — EVV updates.
- Fair Hearing — Fair hearings information.
Email CLASSPolicy@hhs.texas.gov and DBMDPolicy@hhs.texas.gov with any questions.
Medical Care Advisory Committee: Concerning Rider 23
November 15th, 2025
HHSC Cross-Agency Employment Conference : Info For Those Who Could Not Attend
November 14th, 2025
If you were unable to attend the virtual conference, copies of the handouts can be found below
Cross-Agency Employment Conference 2024 Program Handout
HHSC was not able to able to record the event nor did they allow time for Q&A.
Questions, however, may be submitted to: employment_services_virtual_conference@hhs.texas.gov
Recordings of Previous DAHS and ISS Webinar with LTCR
November 11th, 2025
A recording of the October 30 DAHS and Individualized Skills and Socialization provider webinar with HHSC Long-term Care Regulation is now available. The presentation (PDF) is also available.
Listen to the webinar recording.
Email LTCR Policy for a transcript.
May 4th, 2025
A recording of the April 24 DAHS and Individualized Skills and Socialization provider webinar with HHSC Long-term Care Regulation is now available. The presentation (PDF) is also available.
Listen to the webinar recording.
Email LTCR Policy for a transcript.
IL 2025-25 Now Published- HHSC Rider 23
November 10th, 2025
HHSC Rider 23 from the 2026-2027 General Appropriations Act, Senate Bill 1, 89th Texas Legislature
HHSC has published the Information Letter IL 2025-25 regarding the Rider 23: Texas Administrative Code Rule Amendments, Personal Attendant Base Wage Discontinuation, Rate Enhancement Discontinuation, Established Average Hourly Wage Assumed in Methodology, and Established Direct Care Wage and Benefits Expense Ratio, effective September 1, 2025. Review the IL for more information.
More information about the attendant programs and payment rates is available on the HHSC Provider Finance Department (PFD) webpage.
If you have questions, contact the HHSC PFD, Long-term Services and Supports (LTSS), Center for Information and Training at PFD-LTSS@hhs.texas.gov or (737) 867-7817.
LTC Provider Bulletin Now Available
Nov 10th, 2025

The November 2025 Long-Term Care (LTC) Provider Bulletin has been published on the LTC homepage on TMHP.com.
Visit the TMHP LTC homepage regularly for news, reminders, training opportunities, and other important program updates.
May 5th, 2025
The May 2025 Long-Term Care (LTC) Provider Bulletin has been published on the LTC homepage on TMHP.com.
Visit the TMHP LTC homepage regularly for news, reminders, training opportunities, and other important program updates.
February 15, 2025
The February 2025 Long-Term Care (LTC) Provider Bulletin has been published on the LTC homepage on TMHP.com.
Joint Training From HHSC For Providers
Joint Training Page Available for HCS/TxHmL/ICF/ISS Providers
The HCS and TxHmL programs now have a Joint Training Opportunities page where providers can register for upcoming classes. Class size will be limited to maximize participation, but classes will be offered regularly. Providers should check the page often for updates. There will be recordings of special presentations available for viewing on-demand later.
November 2025 LTCR Provider Webinar Training Opportunities
HCS/TxHmL Webinars
Death Notifications and Provider Investigation Reports for HCS/TxHmL Providers
Tuesday, Nov. 25
3–4 p.m.
Register here for the webinar.
HCS/TxHmL In-Person Training
Register here for any of the following HCS and TxHmL Joint Training Opportunities
Writing Acceptable Plans of Correction for HCS and TxHmL Providers
Thursday, Nov. 13
9:30 a.m. to 4 p.m.
Palestine, TX
ISS Webinars
Writing Plans of Correction for Individualized Skills and Socialization Providers
Wednesday, Nov. 19
1:30–3 p.m.
Register here for the webinar.
For more training opportunities, visit the Joint Training Course Catalog.
* Reminder about New Long-Term Care Regulation Training Registration From HHSC
HHSC has announced that registering for Joint Training will be easier and more efficient through our new Learning Management System (LMS), Learning Tree. Long-Term Care Regulation (LTCR) Joint Training began using the LMS for training registration on Sept. 1, 2025.
What is the Learning Tree LMS?
- A user-friendly online platform designed to enhance your learning experience.
- Centralizes course registration and access.
You’ll need an account to register for in-person trainings or virtual webinars.
How do I register for an Account?
Step 1: Create an Account
- Navigate to the Registration Link.
- Fill in the required information:
- First Name, Last Name – Formatted as it would appear on any training certificates.
- Email Address – It’s important to obtain your certificates in your Completed Courses. We recommend using your personal email address. This will also be your username.
- Cell Phone – This is not required.
- Select the correct Affiliation for your account or role.
- Select the Register button to create your account on our system.
Step 2: Create a New Password
After registering for an account, you will be taken to a new screen to reset your password. Passwords created in the Learning Tree LMS must include:
- Minimum of 8 characters
- Maximum of 12 characters
- 1 uppercase letter
- 1 lowercase letter
- 1 number
- 1 special character
Special Characters include: ~!@#$%^&*_-+=’|(){}[]:;”<>,.?/
Step 3: Register for Training
After you reset your password, you’ll be re-directed to your Learner Dashboard.
- Select Register for Course on the left navigational pane.
- Locate the course you are signing up for.
- If you know the name of the training you’re looking for you can also type it in the search bar at the top. Press <Enter> on your keyboard or Find Course to search, and the course should appear.
- Click Register.
- Click Proceed to Checkout.
- Click Confirm.
- Click Go to Dashboard.
Courses are free of charge unless otherwise noted.
September & October 2025 LTCR Provider Webinar Training Opportunities
ICF Webinars:
Hurricane Season – Ready or Not! Preparedness for Intermediate Care Facilities
Tuesday, Sept. 23
10–11:30 a.m.
Register here for the webinar.
(HCS/TxHmL) Webinars:
Plan of Removal for HCS and TxHmL Providers
Thursday, Sept. 25
3:30–5 p.m.
Register here for the webinar.
Hurricane Season – Ready or Not! Preparedness for HCS/TxHmL and Individualized Skills and Socialization Providers
Monday, Sept. 29
1:30–3 p.m.
Register here for the webinar.
Death Notifications and Provider Investigation Reports for HCS/TxHmL Providers
Wednesday, Oct. 8
2–3 p.m.
Register here for the webinar.
HCS/TxHmL Certification Standards: An Overview of Changes
Wednesday, Oct. 29
3–4 p.m.
Register here for the webinar.
LIVE In-Person Training
Writing Acceptable Plans of Correction for HCS and TxHmL In-Person Training
HHSC Long-Term Care Regulation will provide an in-person training event for HCS and TxHmL Providers. This course will cover the necessary components for a Plan of Correction and the Informal Dispute Resolution process along with other related topics. This is an interactive training, and participants will be expected to engage with one another and the instructor during the training. Continuing education credit will not be offered for this training, but a certificate of attendance will be provided to all participants who meet attendance requirements.
Writing Acceptable Plans of Correction for HCS and TxHmL Providers
Thursday, Oct. 2, 2025
9:30 a.m. to 4 p.m.
Brownwood, TX
June & July 2025 LTCR Provider Webinar Training Opportunities
- Tuesday, June 17, 2025
- 10:00 AM – 11:30 AM
- Registration
Regional Offsite Review Process for Critical Incidents Reported into the Critical Incident Management System for HCS/TxHmL
- Thursday, June 19, 2025
- 3:00 PM – 4:00 PM
- Registration
Medication Management for HCS/TxHmL Providers
Wednesday, July 9, 2025
- 1:30 PM – 3:00 PM
- Registration
Hurricane Season – Ready or Not! Preparedness for Intermediate Care Facilities (ICFs)
- Monday, July 14, 2025
- 1:30 PM – 3:00 PM
- Registration
Reporting Abuse, Neglect, Exploitation Changes and Self-Reporting Incidents for Intermediate Care Facilities
- Wednesday, July 23, 2025
- 9:30 AM – 10:30 AM
- Registration
Hurricane Season – Ready or Not! Preparedness for Home and Community-Based Services, Texas Home Living (HCS/TxHmL), and Individualized Skills and Socialization Providers
- Tuesday, July 29, 2025
- 3:30 PM – 5:00 PM
- Registration
Live Training
Writing Acceptable Plans of Correction for HCS and TxHmL Providers (Longview, Tx)
- Wednesday, June 25, 2025
- 9:30 AM – 4:00 PM
- Registration
Writing Acceptable Plans of Correction for HCS and TxHmL Providers (Victoria, Tx)
- Wednesday, July 16, 2025
- 9:30 AM – 4:00 PM
- Registration
April & May 2025 LTCR Provider Webinar Training Opportunities
Webinars
License Types for Individualized Skills and Socialization Providers (course description)
- Wednesday, April 23, 2025
- 1:00 PM – 2:00 PM
- Registration
- Tuesday, May 6, 2025
- 2:00 PM – 3:00 PM
- Registration
Writing Acceptable Plans of Correction for ISS Providers (course description)
- Thursday, April 24, 2025
- 1:30 PM – 3:30 PM
- Registration
Death Notifications and Provider Investigation Reports for HCS/TxHmL Providers (course description)
- Friday, April 25, 2025
- 2:30 PM – 3:30 PM
- Registration
Understanding Reportable Incidents for Individualized Skills and Socialization Providers (course description)
- Tuesday, May 20th, 2025
- 3:30 PM – 4:30 PM
- Registration
Administrative Penalties and Related Processes in HCS & TxHmL Providers (course description)
- Wednesday, May 21, 2025
- 3:00 PM – 4:00 PM
- Registration
Live Trainings
- Writing Acceptable Plans of Correction for HCS and TxHmL Providers (course description)
- Wednesday, May 14, 2025
- 9:30 AM – 4:00 PM
Edison Plaza
350 Pine Street 9th floor
Room: 9036 B
Beaumont, TX 77701
From Awareness to Action: Responding to Abuse, Neglect and Exploitation
Tuesday, May 6
8:30 a.m. to 4:30 p.m.
Amarillo, TX
Register for in-person training
Infection Control – Break the Chain of Infection
Wednesday, May 7
8:30 a.m. to 4:30 p.m.
Amarillo, TX
Register for in-person training.
Web-Based Training
Top 10 Citations for Home and Community-based Services and Texas Home Living Fiscal Year 2023
Long-Term Care Regulation
https://apps.hhs.texas.gov/business/CBT/deficiences/hcs-txhml-2023/
January 2025 LTCR Provider Webinar Training Opportunities
Reporting Abuse, Neglect, Exploitation Changes and Self-Reporting Incidents for Intermediate Care Facilities
Tuesday, Jan. 14
2–3 p.m.
Register here for the webinar.
Regional Offsite Review Process for Critical Incidents Reported into the Critical Incident Management System for HCS/TxHmL
Wednesday, Jan. 15
2–3 p.m.
Register here for the webinar.
Flu and COVID-19: What You Need to Know
Thursday, Jan. 16
1:30–2:30 p.m.
Register here for the webinar.
Individualized Skills and Socialization Survey Process and ANE Overview
Tuesday, Jan. 21
2–3:30 p.m.
Register here for the webinar.
AlertMedia: Be Prepared. Stay Informed.
Friday, Jan. 24
1:30–2:30 p.m.
Register here for the webinar.
These 3 webinars below are not for HCS/TxHmL/ICF specifically, but they do apply to those in Long-Term Care Facilities or Programs
Weight Loss in Older Adults
Thursday, Jan. 23
1:30–3:30 p.m.
Register here for the webinar.
Dehydration: Prevention and Intervention in Long-Term Care Communities
Tuesday, Jan. 28
9:30–11:30 a.m.
Register here for the webinar.
Pressure Injury Prevention
Thursday, Jan. 30
1:30–3:30 p.m.
Register here for the webinar.
IDD and PI Quarterly Webinar-LTCR Recording Available – October 29
November 7th, 2025
The October 29th recording of the IDD Programs and Provider Investigations Quarterly Webinar with Long-term Care Regulation is now available.
Listen to the webinar recording.
Read the IDD and PI Quarterly Webinar PDF
Winter Weather Emergency Resources & Considerations: Update
October 31st, 2025
Now Is The Time To Start Prepping For Winter Weather Emergencies
It finally feels like fall weather in Texas, and before you know it, winter will be upon us. As IDD providers, you all know that you can’t wait til the last minute.
For winter weather preparation, IDD providers should focus on creating an emergency kit with supplies like food, water, medication, and batteries, and ensuring a backup heat and power source. It is crucial to make a plan for both individuals and staff, including communication and transportation, and to ensure all necessary equipment, medication, and clothing are available for each individual.
- Emergency kit: Assemble a kit with non-perishable food, water, medications, first-aid supplies, and extra warm clothing for each individual.
- Medication and medical supplies: Refill all necessary prescriptions in advance and have an emergency supply of medical items.
- Backup power: Have a backup power source, such as a generator, and ensure batteries for medical equipment and flashlights are fully charged and extra batteries are on hand.
- Backup heat: Plan for an alternative heat source if the primary one fails, such as a fireplace or a space heater, and have the necessary safety equipment, like a fire extinguisher.
- Home insulation: Seal windows and doors to prevent cold air from entering.
- Plumbing: Winterize pipes to prevent them from freezing and bursting.
- Communication plan: Create a plan for how to communicate during an outage, including having a battery-powered radio to receive weather alerts.
- Charging devices: Keep all mobile phones and other essential devices charged and have a plan for charging them if power is lost.
- Transportation: Plan for accessible transportation options in case of evacuation or an emergency.
- Vehicle preparedness: Ensure vehicles are winter-ready with proper fluid levels, good tires, and a winter storm kit in the car.
- Assistive devices: Tune up and prepare assistive technology devices, making sure they have their own emergency kits and model information.
- Service animals: Prepare service animals with necessary gear like coats and boots for extreme cold.
- Stay informed: Sign up for local alerts and warnings and stay informed about the weather forecast.
- Dress in layers: Advise individuals to dress in layers and wear waterproof, insulated boots, and a hat to stay warm.
- Know the risks: Be aware of the signs of cold-related illnesses like hypothermia and frostbite.
- Community resources: Connect with community groups or organizations like religious communities or food banks that may host clothing drives.
- Emergency committee: Create a winter weather emergency committee to oversee preparation and response efforts.
- Staffing: Plan for staff coverage and ensure there are enough people to care for individuals in the event of transportation issues.
December 30th, 2024

HHSC reminds long-term care facilities and agencies to review and update emergency plans for freezing temperatures and snow. Emergency plans for extreme weather should include the provider’s plan to address:
- Power loss.
- Water and food needs.
- Medical and pharmaceutical supplies.
- Communication to families and staff.
- Staffing shortages.
- Sheltering in place and evacuation, as applicable.
Providers must follow emergency preparedness rules and their own internal emergency preparedness policies and procedures.
Facilities with generators should perform any maintenance or needed testing while the weather is mild. This will ensure the equipment functions in case of extreme cold or power loss.
It’s important to review building integrity and identify any areas that may need repair, reinforcement, or weatherproofing. Multi-story buildings should review any other needed measures should evacuation be required and have a plan in place for how to move residents around or out of the building if there’s a loss of power.
Preparing for disaster is the most important step in protecting the Texans we serve and reducing the risk for loss of life.
Email questions to LTCRpolicy@hhs.texas.gov.
December 22nd, 2023
LTC Provider Resources During an Emergency
Long-term care providers impacted by the current severe weather event should be implementing emergency management plans. LTC providers in need of resources or assistance during an emergency, such as the current severe weather, are reminded that you can:
- Contact your LTCR regional office regarding events that are affecting residents (such as no heat, evacuation, frozen fire sprinkler systems, etc.). They can initiate an emergency request.
- Contact your local emergency management or Regional Advisory Council, who can initiate a STAR request.
- Contact your local power company if you are having power issues. Nursing facilities, assisted living facilities, and inpatient hospices should inform the power company that you are an LTC provider, as those providers are prioritized for service restoration per the Public Utility Commission rules.
- Contact your Texas Department of Emergency Management District Contacts if you are having challenges getting generator fuel.
If you need guidance or assistance in relocating residents, work with your LTCR Regional Director. All requests to exceed licensed capacity must be approved by the Director of Survey Operations. If your facility is projected to exceed its licensed capacity because it is accepting residents who have been evacuated from another facility, email Renee Blanch-Haley and include State Capacity Increase Request in the subject line.
Please refer to Provider Letter 2018-19 (PDF) as applicable and to your program’s rules for additional important information regarding emergency preparedness. If you have any questions, contact your LTCR regional office, email LTCR Policy Rules and Training or call 512-438-3161.
Where To Find Medicaid Eligibility Information for LTC Providers: TexMedConnect
October 28th, 2025
Medicaid Eligibility Reports – SSI Medicaid
HHSC has been working on enhancements to improve awareness and visibility of the Medicaid recertification date to increase timely submission. HHSC announced that be making changes to the current training video on this subject and will release info about this in the near future.
Current video on this topic (updated 7 months ago) is available at: https://www.youtube.com/playlist?list=PLIe60BLvrbESNOLho-L03v4Vf-GH4TNv1
March 25th, 2025
Video About Medicaid Eligibility Reports on the LTCOP Dashboard Now Available on YouTube
An educational video focused on Medicaid eligibility reports on the Long-Term Care Online Portal (LTCOP) Dashboard has been added to the Texas Medicaid & Healthcare Partnership’s HCS and TxHmL YouTube Playlist. Read the full alert.
November 14th, 2024
Eligibility Information Available for Long-Term Care Providers and LIDDAs
LTC providers and LIDDAs that are seeking eligibility information can pull Medicaid Eligibility and Service Authorization Verification (MESAV) using any of the following field combinations through TexMedConnect.
This service can be accessed 24 hours a day, 7 days a week
. • Medicaid/Client No. and Last Name
• Medicaid/Client No. and Date of Birth
• Medicaid/Client No. and Social Security Number
• Social Security Number and Last Name
• Social Security Number and Date of Birth (DOB)
• Last Name, First Name, and DOB
MESAV can provide the Medicaid eligibility Program Type, Coverage Code, and Medicaid Recertification Due Date to help providers ensure appropriate and continued Medicaid eligibility for long-term care services.
Upcoming Webinars Presented By Consolidated Planning Group
October 28th, 2025
Click On The Webinar Name Below To Register For Upcoming Webinars From Consolidated Planning Group
November 4, 2025
12:00p – 1:00p
Webinar
November 6, 2025
12:00p – 1:00p
Webinar
November 11, 2025
12:00p – 1:00p
Webinar
November 12, 2025
12:00p – 1:00p
Webinar
November 13, 2025
12:00p – 1:00p
Webinar
November 18, 2025
12:00p – 1:00p
Webinar
November 18, 2025
6:30p – 7:30p
Webinar

The Team at Consolidated Planning Group
SNAPS Status Update: Beginning Nov. 1st, 2025
October 28th, 2025
November SNAP Benefits & Information Resources
OIG Audits & Inspections: Update
October 28th, 2025
OIG Beginning Auditing of Cost Reports
Link to OIG FY 2026 Audit Work Plan:
OIG Response To Inquiries:
-We will look at the cost reports for this audit. Since many cost report preparers are external to the entity providing the cost report and one cost report preparer might be used for multiple entities, we wanted to gain an understanding of how the contracts with cost report preparers are written.
-After reviewing the contracts, we will determine next steps. For the audit we will probably engage both the entity submitting the cost report and the preparer. Those entities selected will receive more information about the scope and objective(s) of the audit. More information will be requested after that to support the expenses and to ask specific preparation questions as needed.
–We take multiple factors into account when determining which entities to look at, including how much is reported in the cost reports, are some outliers, can we gain efficiencies in any way, like the same preparer did multiple cost reports. If we decide to narrow our scope to a specific line item in the cost reports, we might look at more providers than we would if we focus on the cost report as a whole.
–Once we are farther along in the process and have determined our preliminary scope and objective(s), I will be happy to have further discussions about which entities we determined to include in the audit
October 5th, 2025

What triggers an OIG audit or investigation?
The Texas Health and Human Services (HHS) Office of Inspector General (OIG) is charged with preventing fraud, waste and abuse in health and human services programs to protect taxpayer dollars and program clients. To achieve this, OIG conducts audits, inspections, and investigations to ensure that Medicaid funds are used appropriately and efficiently. Another important fact is that TMHP (Texas Medicaid Health Portal), HHSC, and OIG are all part of the enrollment and revalidation process for HCS/TxHmL.
Some of you may be familiar, for example, with the “site visit” conducted by CMS for TMHP, for all new applications submitted for enrollment to PEMS (Program Enrollment Management Services). The OIG reviews these site visit reports and enrollments into TMHP. Some common deficiencies in this area are:
Incomplete Items-such as criminal hx checks, license checks, and managing employees or subcontractor checks.
Tips: Double-check disclosures before submitting the application or revalidation. OIG also recommends that you start the revalidation process early, it can be a very long process. During Revalidation, you may expect site visit to verify if the provider is actually at that location. This would be for re-enrollment or revalidation, as far as my understanding, and that this is not the same as the federal OIG site visit. This is the state OIG visit to verify your program is actually at that location.
Audits: To mitigate their own risks, providers should be aware of some of the issues that could lead to OIG scrutiny. Some of the common HCS/TxHmL errors seen:
–LIDDAS-lack sufficient progress notes
–Missing progress notes, service delivery logs
–False Documentation
-Facility did not have records to support telehealth-consents and records for what they are billing that meets billing requirements for what is billable
–Telemedicine must have written permission and include observation, diagnoses, training and testing
–Medication Administration: Billing For services not rendered
–Quality of Care-billing for expensive services but giving low end service/care
–Misappropriation of Funds
Some new areas that OIG has noted they are concentrating on that come under their purview are:
-Solicitation (Can’t do anything to influence the individual’s choice of provider). OIG is hitting hard in this area now and in the next year!
-Also Reviewing Cost Reports in some cases as well now. Due to complaints and due ot risk assessments they have completed concerning cost reports.
Common Triggers:
Billing errors
High Dollar Claims
Unusual Payment Patterns
Inappropriate Documentation (missing documentation for service billed, missing appropriate dates, times, signatures for each service entry of billable services, etc…)
Billing For Services Not Defined As Billable in The “Billing Requirements”
A note about common triggers
**It’s important to note that being flagged for an OIG data review does not automatically indicate wrongdoing. These flags may simply reflect billing or service patterns that differ from peers and may warrant a closer look. Tip from OIG: If you self-disclose during an audit, you may get to keep some or all of the money or at least avoid additional fees being charged.
Report waste, fraud, and abuse of HHSC programs to: ReportTexasFraud.com
For questions, please email: Jeremy.fuchs@hhs.gov
Rider 56: Appropriate Care Settings for Individuals with Severe and Persistent Mental Illness and Co-Occurring Conditions Study
October 27th, 2025
(a) For the purposes of developing the study and proposal:
(1) An individual must meet the following eligibility criteria to qualify for the pilot program:
(A) Have a diagnosis of severe and persistent mental illness and may have a cooccurring condition, such as a traumatic brain injury or intellectual and developmental disability; and
(B) Spent three or more of the past five years in a psychiatric hospital; or
(C) Have been incarcerated more than three times and experienced two psychiatric crises in the previous three years; and or,
(D) Have been admitted to hospital emergency rooms more than three times with psychiatric crises.
(2) The proposed location of the pilot program shall not be classified as an Institution of Mental Disease under federal Medicaid regulations and shall be designed to ensure compliance with federal funding requirements.
(b) The study and proposal shall:
(1) Assess the existing unmet needs in the service continuum for the target population;
(2) Assess the need for nursing-level care and other specialized services for the target population;
(3) Identify opportunities to modify or expand eligibility criteria for existing programs and services;
(4) Scalable options for implementing the program at residential care facilities and nursing facilities;
(5) Evaluate whether vacated buildings on state hospital campuses or other state facilities could be rehabilitated and used to provide intensive residential services for the target population; and
(6) Evaluate statutory changes and funding needed to establish the pilot program to serve the target population, including the estimated cost to provide intensive residential services for the eligible population and the estimated cost to rehabilitate vacated buildings on state facility campuses to serve as the location of the pilot program.
No later than October 15, 2026, HHSC shall submit findings and recommendations from the study to the Senate Finance Committee, the House Appropriations Committee, the Legislative Budget Board, the Office of the Governor, and permanent standing committees in the House of Representatives and the Senate with jurisdiction over health and human services.
ICAP Scoring Software Update
October 27th, 2025
Cameras In Private Areas (HCS Program): Update
October 23rd, 2025
HCS Program & Cameras in Private Areas:
HHSC Medicaid division sent Regulatory staff at HHSC an email informing them that “CMS thinks there’s a privacy concern regarding cameras being allowed in private areas (even if justifications are in place), and that CMS will no longer permit this practice.”
According to HHSC, currently, there are no HCS rules specific to this matter. HHSC stated that more details will be forthcoming, but for now, members should be informed that, in the future, this will no longer be permissible. They will provide more clarification in the near future.
Change in IDD Waiver Cost Limits
October 23rd, 2025
New cost limits for the IDD waivers are as follows:
- For DBMD and CLASS, HHSC updated the individual cost limits from $114,736.07 to $149,774.
- For TxHmL, HHSC updated the individual cost limit from: $17,000 to $31,684.
- For HCS, HHSC updated the individual cost limit based on level of need (LON) as described below:
- Intermittent (LON 1), Limited (LON 5), and Extensive (LON 8)
- The amount is increasing from $167,468 to $169,182.
-
- Pervasive (LON 6)
- The amount is increasing from $168,615 to $211,822.
-
- Pervasive plus (LON 9)
-
-
- The amount is increasing from: $305,877 to $392,318
-
PEMS Streamlining Process For TMHP Enrollment
October 22nd, 2025
April 15th, 2025
Beginning May 30, the Provider Enrollment and Management System (PEMS) will be enhanced to streamline the process for Texas Medicaid enrollment, managed care organization (MCO) and dental maintenance organization (DMO) credentialing.
PEMS will feature a new Credentialing Tab for the credentialing application that will allow providers to complete and submit their credentialing information as part of the enrollment process, the reenrollment process, or as a maintenance request.
For more information, refer to Coming Soon: PEMS to Be Updated to Allow Provider Credentialing on TMHP’s Provider Enrollment webpage.
ANE Investigations Backlog Issue: HHSC Rider 164
AAIDD: Texas Chapter Annual 49th Convention (Sept. 30th-Oct. 3rd, 2025) Post Convention Update
October 14th, 2025

Post Convention Report
This year’s AAIDD-Texas Chapter 49th Annual Convention was on Sept. 30th-Oct. 3rd, 2025, and we had a wonderful turnout. As you may or may not know, this is my first year on the board, and it was an awesome experience. I know there were some providers, LIDDA’s, and individuals who just didn’t have funding to come this year or possibly the timing was just not right, and we thank all of you who could make it to the convention. This has been a tough year for everyone in IDD services, especially in the state of Texas.
Next year is our 50th anniversary, so I hope even more of you can attend the convention next year. We plan to go all out for the event! Please don’t forget to sign up to be a member of AAIDD, which gets you so many professional resources, including free material, webinars, and discounts on other resources for IDD, as well discounted rate on the registration for our annual Texas Chapter of AAIDD Convention. Basic Membership cost is very good rate ($90-$185 per year for basic) for national membership, and there is no extra cost for Texas Chapter membership.
I would like to thank all board members for their tireless work to make this happen this year, as well as all the sponsors and vendors. I would like to also thank all the wonderful presenters for the breakout sessions, like Nursing Innovations, Rachel Hopkins from Molina Health Care, and the Transition Support Team members from several of the LIDDAs– Integral Care, Texana, Nueces County. We had an incredible guest, James Meadours for the Opening Session. James is a passionate self-advocate for persons with disabilities and for those who have suffered abuse and has been presenting across the US for many years.
Shelbi Davenport (of the Shelbi Show podcast) did a wonderful job in the general session of hosting her live podcast interview with 3 incredible individuals with Down Syndrome: Martha Haythorn, Jenny Stone (now Underwood), and Austin Underwood. The premise of the interview was to look at the personal perspective of 3 incredible people with Down Syndrome and how the lives of these three people were given the support and freedom to pursue their dreams and how they are now living their best lives.
Austin and Jenny Underwood were actually married not long ago and are both working in jobs they love, which has been a lifelong dream for both of them. After earning a certificate as a prep chef and working as a head of house and chef at an Italian restaurant, Austin founded his own company in 2016 and owns a food truck called “Austin’s Underdawgs” in the DFW area. I have been told they also cater for events! Jenny and Austin both have amazing family support, and we were able to meet their parents at this year’s convention. Jenny has worked as a Teacher’s Aide at the KinderFrogs School at Texas Christian University (TCU) for 20 years. KinderFrogs is a family-focused, early intervention program for children with developmental delays. In her role as a teacher’s aide, Jenny performs many duties from assisting with circle time to preparing lunches and assisting children on the playground.
Martha Haythorn came all the way from Atlanta, Georgia to be with us, and she stole everyone’s heart this week. Martha is incredibly passionate and quite funny, I discovered as well! She was a recipient of a scholarship from Ruby’s Rainbow that allowed her to fund her college time at Georgia Tech and graduate. She has been asked to present at Emory College in 2026 and now has a job providing social media marketing for a medical supplier of respiratory aids that also happens to help many individuals with Down Syndrome with respiratory issues. Martha also sits on the Council for Developmental Disabilities for the State of Georgia. It was my privilege to ask her to present this year and host her for her time here. So happy I got to meet her in person.
Check out some of our photos of the convention!











August 29th, 2025
We invite you to this year’s Texas State Chapter of AAIDD 49th Annual Convention. I am officially a board member this year (Julie Blacklock), and I will also be presenting a breakout session on October 2nd, 2025 especially for HCS providers. Please share with providers, families, and individuals. All are welcome to come. For more information and registration, go to: https://www.aaiddtx.org/2025-convention

KEYNOTE SPEAKER

Opening Session
Wednesday, October 1, 8:45 – 10:30 a.m.
James Meadours, Self-Advocate, National Speaker, Disability Rights Leader
A Journey from Group Living to Independent Living
James Meadours, a nationally recognized self-advocate, shares his powerful story of moving from a group home to living independently in “The Right Direction.” With honesty and courage, James outlines the milestones, setbacks, and supports that helped him take control of his life. From building daily living skills and speaking up for his rights, to embracing community inclusion, James offers a message of hope and empowerment. Attendees will leave with deeper insight into how to support others on their own path to independence.
GENERAL SESSION
Wednesday, October 2nd, 3:00 p.m.-4:30 p.m.
Taking Our Lives in the Right Direction
• Shelbi Davenport, B.S. Better Lives Senior Associate/Practicum Coordinator at TAMU
• Martha Haythorn, Georgia Tech ExCel Graduate, Policy Specialist-Georgia State Legislature
• Austin Underwood, Operator-Austin’s UnderDawgs
• Jenny Stone, Outspoken Self-Advocate and Austin’s partner
This presentation is intended to be a general session in the format of a structured interview that will provide the audience with a personal perspective on how the lives of three people with Down Syndrome were given the support and freedom to doggedly pursue their dreams and who are now living their best lives, with even better things to come. Shelbi Davenport of The Shelbi Show will host the session, interspersing interview questions with video snippets to facilitate and drive the discussion. The audience will be motivated to encourage others with disabilities to let nothing get in the way of following their desired path.
OR
Click on: Tx Chapter AAIDD Convention 2025-brochure-agenda
Remember, as an AAIDD member, you receive a discounted rate for this year’s Texas Convention
Membership: How To Join AAIDD
AAIDD welcomes you to become a member or renew your annual membership now. Click on the link below to choose from the benefit packages that best match your needs.
https://www.aaidd.org/about-aaidd/membership-join/member-types
AAIDD membership advantages include access to a global network of professionals, free webinars, discounts on publications and the annual meeting, eligibility to vote and hold office, access to members-only content like Interest Networks and newsletters, and subscriptions to peer-reviewed journals like AJIDD and Inclusion. Members can also participate in scholarship opportunities and join the Students and Early Career Professionals (SECP) Interest Network.
Why Should I Join AAIDD?
-
Journals and Publications:
Members gain access to peer-reviewed journals and resources on the latest research and policy developments in the field of intellectual and developmental disabilities (IDD).
-
Webinars:
Free access to educational webinars and an archive of past sessions is available to members.
-
Interest Networks:
Members can join specialized groups to connect with peers who share similar interests or disciplines.
-
Global Network:
Connect with a worldwide network of professionals working in the IDD field.
-
Interest Networks:
These provide a forum to share information, network, and find leadership opportunities.
- Annual Meeting: Receive discounts on registration for the AAIDD Annual Meeting.
- Bookstore: Get discounts on books and other resources from the AAIDD bookstore.
Information on Job Opportunities working with IDD services
Phishing Alert: Emails From “Fake” HHSC Email Addresses
October 12th, 2025

DO NOT CLICK FILES, LINKS, OR FWD!
The Texas Health and Human Services Commission has identified an active phishing attempt.
The message may appear to come from a trusted colleague, sender, or HHSC email address and often includes links, meeting invites, or file attachments that appear to be legitimate.
If you receive an unexpected or suspicious email, don’t click on the links, open the attachments, or accept the invite.
HHSC is actively working to resolve this issue and will communicate updates.
**Tip From Twogether Consulting:
If you are unsure and know the sender or sender’s email, or if you are expecting an email from HHSC, you may want to contact them by phone or contact them some other way directly to ensure they did actually send you an email, especially if it contains links or attachments.
TULIP: Unavailable Oct. 31st-Nov, 3rd, 2025!
October 6th, 2025
TULIP System Updates
PLEASE BE ADVISED THAT HHSC WILL BE PERFORMING SYSTEM UPDATES TO TULIP.
Don’t forget all EMR checks (Misconduct & Nurses Aids checks) are done through TULIP for HCS/TxHmL/ISS Providers
TULIP will be unavailable from October 31st, 2025 @ 5:00pm to November 3, 2025 @ 8:00am.
These updates are necessary to improve system performance and reliability. More details on issues like password reset will be sent out as they approach the transition date.
Employment First/Employment Services LIVE In-Person Trainings (Oct.-Dec. 2025)
October 5th, 2025
Texas Human Services Commission (HHSC) will be hosting free in-person Employment First/Employment Services trainings across the state from October to December 2025.
What: Employment First/Employment Services Training
Where: Wichita Falls, San Angelo, Weslaco, Lufkin, Sugar Land, and San Antonio
When: Various dates from October to December 2025
Time: 9 a.m. to 4 p.m. CST
Register: Select your session and register now.
Space is limited to 50 seats per event, so register early to reserve your seat.
About the Training
This training is specifically designed for any staff member who has a role in supporting people with disabilities who set employment goals. This includes people with direct, hands-on roles such as:
- Service coordinators,
- Employment specialists,
- Direct care staff,
- Day habilitation staff, and
- Job coaches, supervisors, and others who support individuals as they pursue competitive and integrated employment.
Training topics include:
- Overview of Employment First and the national movement,
- Providing employment services,
- Employment and soft skills,
- Apprenticeship programs, and
- Employer relationships.
DAHS and Individualized Skills and Socialization Provider Webinar with HHSC LTCR:: October 30th, 2025
October 5th, 2025
HHSC Long-term Care Regulation will host a webinar for Day Activity and Health Services (DAHS) and Individualized Skills and Socialization providers
Date: October 30, 2025
Time: 11 a.m. to noon.
Place: Webinar
DAHS and Individualized Skills and Socialization providers should attend this and all webinars with HHSC LTCR.
LTCR will provide the latest updates and answer questions from participants.
Cross Agency Employment Conference – Thursday, November 13
October 3rd, 2025
Save the date for the second annual Cross Agency Employment Conference on Thursday, November 13, 2025.
What: Cross Agency Employment Conference
When: Thursday, November 13, 2025
Where: Online
Registration: Registration will open in mid-October.
More Information
The Cross Agency Employment Conference will feature presenters from Texas HHS, the Texas Workforce Commission, and the Texas Education Agency.
The conference is open to agency staff, job seekers, providers, family members, and advocates who want to understand the job seeker’s journey to employment, and the services and support available to them through each life stage.
ASL/CART services will be provided for this event.
This conference is supported by the Centers for Medicare & Medicaid Services (CMS) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $27.7 million with 100 percent funded by CMS/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CMS/HHS, or the U.S. Government.
HHSC Webinar: Advances in Trauma Informed Care- Oct. 10th, 2025
Oct 3rd, 2025

HHSC is hosting a free webinar on World Mental Health Day, Friday, October 10, 2025, from 9:30 a.m. to 11 a.m. CST.
What: Webinar on Advances in Trauma Informed Care
When: Friday, October 10, 2025, 9:30 a.m. to 11 a.m. CST
Register Now: Register for the webinar.
Trauma is not just an event, it’s an experience that disrupts a person’s sense of safety, stability, and connection. It can alter brain development, behavior, and emotional regulation. For many people, trauma leaves invisible wounds that shape how they learn, relate, and navigate the world. We’ll unpack how trauma manifests across developmental stages and why people with intellectual or developmental disabilities face heightened risks. We’ll also share how professionals, caregivers, and advocates can foster environments of psychological safety, healing, and resilience
Payment Rates For Attendants-Information Letter 2025-24
September 19th, 2025
“HHSC has published the Information Letter IL 2025-24 (Replaces IL 2025-17), regarding the approved payment rates for personal attendant services in various programs. The HHSC Provider Finance Department webpage has more information about the approved payment rates.
Review the IL for more information. If you have further questions, contact HHSC PFD, Long-term Services and Supports (LTSS), Center for Information and Training at PFD-LTSS@hhs.texas.gov or (737) 867-7817.Payment Rates”
PPAT Fall Conference For September 24th-26th, 2025
September 17th, 2025
August 30th, 2025
August 29th, 2025
Information below is from PPAT for Registration and Info!
MARK YOUR CALENDAR & RESERVE YOUR ROOM NOW!
PPAT’s 28th Annual Fall Conference
DoubleTree Hotel * Austin, Texas
September 24-26, 2025
Preview of Sessions (The list is not inclusive and is subject to change)
· –Office of Inspector General: Responsibilities & Interactions with IDD Services
· All Things TMHP: Changes coming to PEMS, Claims Submission & Payment Overview, Etc.
· Updates on HHSC Office of Disability & Coordinating Services Activities
· LON Increases: Overview of Process & Requirements for Securing an Increase
· Status of Court Ruling on 2010 Class Action Lawsuit Re: Violation of the ADA (failure to integrate persons with disabilities into the community from nursing homes)
· Building Collaborative Relationship with Your LIDDA
· 89th Legislative Session: What Happened & Next Steps and Sunset Review of HHSC
· Abuse, Neglect & Exploitation Investigative Processes for ICF/IID & HCS
· Regulatory Year in Review & More: Joanalys B. Smith, Attorney at Law
· Billing & Payment Audits: Overview of Process, What to Expect, Etc.
· Implementation of HB 1041 (Turner, 89 R) re: insurable interest of certain persons providing care to individuals with IDD.
· Rider 23: Changes to Reimbursement Methodology & Cost Report Process
· Change of Ownership (CHOW): Step-by-step review of process
Registration Information & Marketing Opportunities (please contact Jaim Kaysonphet)
· Registration Form (one must be completed per person)
· Sponsorship Forms (Levels and Event)
· Marketing Forms (Ads, Goody Bag Donations, Silent Auction Donations)
· Exhibitor Form (Discounted registration up to two additional attendees)
Forms can be completed through the online registration link below, emailed to PPAT100@aol.com, faxed to 512-458-3078 or mailed to the PPAT Office at 8711 Burnet Road, Ste. E-53, Austin, TX 78757. Questions? Call the PPAT Office at 512-452-8188 or email Jaim Kaysonphet, Administrative Assistant at jaimppat@aol.com. EARLY Registrations ends on August 22!
Online Registration: 2025PPATConfREGISTRATION
Online Room Reservations: 2025PPATConfHotelReservations
Hotel Information:
DoubleTree Hotel North
6505 IH 35 North
Austin, TX 78752
You can also make reservations with the DoubleTree Hotel toll-free national reservation center line at 1.800.866.3126, by the August 22, 2025 designated cut-off date to receive the special rate of $175.00 Single/Double. Identify yourself with the Private Providers Association of Texas (promotional code CDTPAT). Reservations are subject to space and availability. All reservations must be guaranteed by credit card or advance deposit. Reservations must be canceled by 1:00 PM (noon) local time, 48 hours before the day of arrival or the first night of the stay will be charged.
Parking:
Covered self-parking for conference attendees is $10/day. Parking based on availability. Valet parking is not available at this location.
We Look Forward to Seeing You!
Employability Status Check Changes For All LTCR Providers
September 17th, 2025
Employability Status Check Changes As Of September 7th, 2025
HHSC recently moved the Employability Status Check search to the Texas Unified Licensure Information Portal (TULIP).
FYI-An issue was found by HHSC, during the transition process, with the Employability Status Check data retrieval process, which is causing some difficulty for providers conducting due diligence searches.
HHSC is working diligently to resolve the problem.. Providers will be notified about a workaround if it is not fixed in a timely fashion.
-
What do you need to do?
- Providers must now use the my.site.com/EMR/ link to conduct employability status checks in TULIP.
- If the previous Employability Status Check website is accessed, please click on the home link to be directed to the new employability searches in TULIP.
- The new searches in TULIP now display the search criteria and “no results found” on the same screen. A fix is now deployed to include a User Guide.
- The Employability Status Check search checks licensure status (Nurse Aides, Medication Aides and NFAs).
- The Employability Status Check search does not display anything when no records are found. The lack of results means the person is not part of the searched registry. Screenshot this search, including the search criteria and computer date and time. Until a fix is deployed, follow this guidance.
- The EMR search displays the first name, last name and social security number when no records are found. To download the results, click the download button in the top right corner of the yellow results bar. The download contains the date and time of the search. If no date is present under “Misconduct Registry Enter Date,” the searched person is NOT on the EMR.
- Please reference the User Guide which can be accessed on the new Employability Status Check search page under the heading “additional links” located at the bottom left-hand side of the page.
- To remain in compliance, providers must redo all searches conducted from Sept. 7, 2025, to Sept. 12, 2025, and take a screenshot of the results, including the date and time for searches that yield “no results found.”
- As required by Title 26 of the Texas Administrative Code, Chapter 561, Rule 561.3, providers must search the Employee Misconduct Registry and Nurse Aide Registry to determine if the person applying for employment is listed as unemployable on either registry. With the transition of the Employability Status Check to TULIP, providers are now required to conduct both searches in TULIP.
For questions, email CARE@hhs.texas.gov.
ISS Updates & New Rules (HCS/TxHmL)
September 11th, 2025
Employability Status Check (Nurse’s Aide/Misconduct Registry) Update
As of Sept. 11th, 2025
HHSC has moved the Employability Status Check search to the Texas Unified Licensure Information Portal (TULIP).
During this transition, Regulatory staff identified an issue with the Employability Status Check data retrieval process that is causing some difficulty for providers conducting due diligence searches.
HHSC is hoping to resolve the issue by tomorrow. HHSC will provide a workaround if they are unable to resolve it, and providers will be notified. We appreciate your patience.
What you need to do:
- Moving forward, providers will need to check the employability status in TULIP.
- If you access the previous Employability Status Check website, click on the home link to be directed to the new employability searches in TULIP.
- As required by Title 26 of the Texas Administrative Code, Chapter 561, Rule 561.3, providers must search the Employee Misconduct Registry and Nurse Aide Registry to determine if the person applying for employment is listed as unemployable on either registry. With the transition of the Employability Status Check to TULIP, providers are now required to conduct both searches in TULIP.
For questions, email CARE.
September 5th, 2025
ISS FAQ’s Updated Sept. 2nd, 2025
The current revision has added the link to PL 2025-01 (AlertMedia), updated TAC links to the new TAC website, added information about AlertMedia and information for providing information to HHSC during an emergency, and added a response regarding after-hour care and charging families.
In addition, there are comments to some of the questions concerning the revisions made to Emergency Response Plans and Fire Drills, and various sections containing the old TAC links.
August 15th, 2025
Current ISS Rules-July 24th, 2025 edition
August 1st, 2025
HHSC has published the following proposed amendments to the rules governing an ISS program provider. They are currently taking comments until August 25th, 2025. Please notify your provider association that your program is affiliated with for assistance with submitting comments. (PPAT, PACSTX, etc…)
Also provided below are the proposed schedule of administrative penalties for ISS providers and the current schedule of administrative penalties for DAHS providers. As you will see, the DAHS administrative penalties are less than the ISS provider penalties; however, HHSC has no say over the ISS administrative penalties, as they are under DAH’s Enforcement Division.
Proposed Amendments to ISS Rules
ISS Scope & Severity Grid For Penalties
DAHS Scope & Severity Grid For Penalties
July 23rd, 2025
HHSC Publishes Revised PL 2019-24
HHSC has published revised Provider Letter 2019-24, Informal Dispute Resolution Process for Day Activity and Health Services (DAHS), DAHS with Individualized Skills and Socialization, and DAHS with Individualized Skills and Socialization Only providers. Revisions include updated hyperlinks to reflect the new website location for TAC rules, clarification to distinguish the Informal Dispute Resolution (IDR) request process for each provider type, and non-substantial revisions throughout this Provider Letter to enhance clarity.
DAHS and ISS IDR revise process
April 6th, 2025
Register Now for April 24 DAHS and Individualized Skills and Socialization Provider Webinar with HHSC LTCR
HHSC Long-term Care Regulation will host a webinar for Day Activity and Health Services (DAHS) and Individualized Skills and Socialization providers on April 24 from 11 a.m. to noon.
DAHS and Individualized Skills and Socialization providers should attend this and all webinars with HHSC LTCR.
LTCR will provide the latest updates and answer questions from participants.
October 26th, 2024
HHSC Publishes Revised PL 2023-01
HHSC has published revised Provider Letter 2023-01 New Regulatory Rules for Long-term Care Regulation (LTCR) Individualized Skills and Socialization Services.
Revisions include information regarding the issuance of temporary initial licenses to applicants for DAHS-Individualized Skills and Socialization Only licensure, clarification on capacity, LTCR surveys, Form 3613-A requirements, emergency response plan requirements, and updates to contact information for TULIP Support.
September 9th, 2024
HHSC Publishes PL 2024-15: Return To Temporary Licensure for DAH’s ISS Only Providers
HHSC has published Provider Letter 2024-15 Temporary Initial Licensure for DAHS-Individualized Skills and Socialization Only Providers.
Beginning September 9th, 2024, HHSC will resume issuing temporary initial licenses to DAHS-Individualized Skills and Socialization Only providers prior to conducting a health survey.
May 5th, 2024
UPDATED ISS FAQ’S
- Pages 18, 21 & 24
- Pages 32, 33, and 36 thru 39
- Pages 41, 57 & 58,
- Pages 63, 68, 71, 73 and 75 thru 80.
HHSC Long-term Care Regulation updated the Individualized Skills and Socialization frequently asked questions document on May 2, 2024.
April 1st, 2024
ISS Administrative Penalties Scope and Severity Grid
Figure: 26 TAC §559.253(b)
| SCOPE AND SEVERITY GRID FOR ADMINISTRATIVE PENALTIES | |||
| ISOLATED | PATTERN | WIDESPREAD | |
| Immediate threat | Substantial=NRTC | Substantial=NRTC | Substantial=NRTC |
| J | K | L | |
| Initial | $400–$600 | $450–$650 | $500–$700 |
| Repeat | $500–$700 | $550–$750 | $600–$800 |
|
Actual harm |
Substantial=NRTC | Substantial=NRTC | Substantial=NRTC |
| G | H | I | |
| Initial | $250–$450 | $300–$500 | $350–$550 |
| Repeat | $350–$550 | $400–$600 | $450–$650 |
|
No actual harm with a potential for more than minimal harm |
Non-Substantial=RTC | Non-Substantial=RTC | Substantial=NRTC |
| D | E | F | |
| Initial | $100–$300 | $150–$350 | $200–$400 |
| Repeat | $200–$400 | $250–$450 | $300–$500 |
|
No actual harm |
Non-Substantial=RTC | Non-Substantial=RTC | Non-Substantial=RTC |
| A | B | C | |
| Initial | $0–$0 | $0–$0 | $0–$0 |
| Repeat | $0–$0 | $0–$0 | $0–$0 |
March 18th, 2024
New Rules For ISS
PL-2023-01(Revised)
https://www.hhs.texas.gov/sites/default/files/documents/pl2023-01.pdf
March 7th, 2024
HHSC Hold Harmless Period Ending
This “hold harmless” period is ending for ISS providers on March 17, 2024.
Beginning March 18, 2024, HHSC will survey for compliance with all regulatory requirements, including off-site provision of services, and move forward with applicable enforcement actions as outlined in Title 26 Chapter 559, Subchapter H, Division 4 (Survey, Investigations & Enforcement)
Draft Amendments to ISS Licensing Rules
February 14th, 2024
Delays In Receiving ISS Licenses
December 15th, 2023
Clarification on Licensure Renewals
All licensed long-term care providers must submit a renewal application in the Texas Unified Licensure Information Portal (TULIP) before their current license expires. While a re-licensure/recertification survey is part of the renewal process, it doesn’t take the place of submitting a renewal application in TULIP.
HHSC encourages providers to submit the application as soon as possible within the 120 days prior to the expiration of their license, so that if there are issues with TULIP — such as the renewal application not being in the TULIP account — the provider has time to work with TULIP Support prior to their license expiring.
If the provider is waiting on pending documentation — such as a current fire marshal report — it’s better to go ahead and submit the renewal application with the deficiency and upload a letter explaining why they don’t have the required documentation.
***If the application isn’t submitted before the license expires, the provider risks providing services without a license. This is only for licensed LTC providers. Does not include HCS/TxHmL providers as they are contracted, not licensed.
December 14th, 2023
ISS UPDATE WEBINAR DECEMBER of 2023
Please review webinar handout for changes to the Implementation Plan and Person-Directed Plan for ISS.
*PDP’s need to reflect type of ISS (In-Home, On-Site, Off-Site) and activities and schedule.
*IP’s need to also reflect type and objectives for type as well as hourly amount and dollar amount for each type of ISS.
August 18th, 2023
Transition to Individualized Skills and Socialization Survey Deadline Extended
HHSC implemented individualized skills and socialization services in the Home and Community-Based Services (HCS) and Texas Home Living (TxHmL) Medicaid 1915(c) waiver programs, effective Jan. 1, 2023.
HHSC is requesting feedback from HCS and TxHmL program providers only on the impact this change has had on individuals receiving services in the form of a short survey.
Take the survey to provide your feedback.
We thank you for your input. HHSC is extending the deadline to submit responses until Aug. 31, 2023.
All HCS and TxHmL program providers who have not submitted a response must complete the survey by this deadline. Providers who have already completed the survey do not need to submit an additional response.
July 17th, 2023
HHSC Updated the Individualized Skills and Socialization Hold Harmless Period through March 17th, 2024
On Jan. 1, 2023, HHSC implemented the DAHS Individualized Skills and Socialization program and offered an initial hold harmless period from Jan. 1, 2023, through June 30, 2023.
HHSC agreed to extend part of the hold harmless period related to the provision of off-site services.
HHSC will survey for compliance with off-site service delivery but will not move forward with enforcement action.
For all other regulatory requirements, beginning July 1, 2023, HHSC will survey for compliance and move forward with applicable enforcement actions as outlined in Title 26 Chapter 559, Subchapter H, Division 4.
The new hold harmless period related to the provision of off-site Individualized Skills and Socialization services begins July 1, 2023, and ends March 17, 2024.
March 28th, 2023
Host Home Companion Care Providers Concerning ISS & PHE Flexibilities For In-Home ISS
Clarification Concerning Information Letter No. 2023-10 (Replaces IL 2023-06) from February 2023
In-Home Individualized Skills and Socialization Information for Program Providers for COVID-19 PHE
In response to COVID-19 and to provide access to day habilitation services, the Health and Human Services Commission (HHSC) temporarily waived certain requirements in Sections 3710, 4381.3, 4381.7(6) and 4381.7(7) of the HCS Billing Requirements and the TxHmL Billing Requirements. Until the end of the COVID-19 PHE, this flexibility will continue as part of in-home individualized skills and socialization.
Effective May 12, 2023, these flexibilities will no longer be in effect:
The flexibility has allowed HCS and TxHmL program providers to provide in-home individualized skills and socialization to an individual in the individual’s residence, including those residing in their own homes or family homes, without having the required justification outlined below. Program providers and LIDDAs need to have transition plans ready for individuals who receive in-home individualized skills and socialization prior to this end date (before May 12th, 2023).
Beginning May 12th, 2023:
in order to receive in-home individualized skills and socialization, individuals must meet all requirements outlined in the HCS and TxHmL Program Rules, the HCS Billing Requirements, and the TxHmL Billing Requirements, which include:
• A physician has documented that the individual’s medical condition justifies the provision of in-home individualized skills and socialization; or
• A licensed professional or behavioral support service provider has documented that the individual’s behavioral issues justify the provision of in-home individualized skills and socialization; or
• The individual is 55 years of age or older and requests to receive in-home individualized skills and socialization.
In addition, after May 11, 2023, a service provider of host home/companion care will not be permitted to provide in-home individualized skills and socialization to the individual to whom they provide host home/companion care services.
Clarification & Answer to Question From Some of Our Readers:
This letter indicates that HHSC does not appear to prevent a host home provider from becoming an ISS provider, nor does it prevent that licensed ISS provider from providing on-site and/or off-site services to their own individuals living with them. In other words, it would appear they can be a HH/CC provider and licensed ISS provider at the same time and they can provide ISS services to their own individuals they are serving as HH/CC providers. They can not provide their own in-home ISS (anymore) as an HH/CC provider as of May 12th, 2023. The only ISS they can provide after May 11th, is if they are a licensed on-site and/or off-site provider.
March 1st, 2023
Reminder Must Be Licensed As ISS Provider To Bill As Of March 1st, 2023
![]()
For HCS/TxHmL Providers, you can’t bill for On-site &/or Off-site ISS as of today March 1st, 2023, if you send someone to an ISS location or have staff providing Off-site services (previously Community DH), if they are not listed as a licensed ISS program.
The directories may be accessed at: https://www.hhs.texas.gov/providers/long-term-care-providers/day-activity-health-services-dahs to find out if the ISS program is licensed.
**You can bill for In-Home ISS as persons providing In-Home ISS do not have to be licensed! No justification is needed for In-Home through May 11th, 2023 I believe. I believe HH/CC providers can still provide In-Home (This was part of the PHE exception prior to March 1st) up through May 11th, 2023, but I am still unclear and will inquire and update everyone when I get some kind of definitive answer.
Previous DH providers & New ISS Provider applicants: If you do not have a temporary ISS license by March 1, 2023, you may not provide or bill HCS, TxHmL, or DBMD providers for on- and off-site ISS services until the temporary license is received. HCS/TxHmL, DBMD Providers who have individuals attending an ISS program may not send persons to the program until they confirm that the operator of the program has received the license. There are no exceptions.
February 21st, 2023
More ISS Training
Very Important: Surveys of ISS Providers With Temporary Licenses
In case this information was overlooked by new ISS providers:
- Once HHSC issues a temporary license, HHSC may conduct a survey at any time.
- HHSC may conduct a survey of any licensed Individualized Skills and Socialization Providers prior to March 1, 2023.
- i.e. if HHSC issues a temporary license on Feb. 21, 2023, HHSC may conduct an initial survey on Feb. 27, 2023.
- HHSC conducts unannounced surveys of ISS Providers.
- For on-site ISS providers, the address on the license must match the address for service provision.
- ISS providers must allow HHSC surveyors access to the on-site location and off-site activity locations.
Please refer to Texas Administrative Code Title 26, Chapter 559 for more info on the LTCR survey process.
February 10th, 2023

How Do I Find A Licensed ISS Provider?
HHSC has now posted directories on the DAHS webpage to help people find a licensed ISS Provider.
The directories may be accessed at: https://www.hhs.texas.gov/providers/long-term-care-providers/day-activity-health-services-dahs
Please note the following:
- There are 2 directories: DAHS with ISS and DAHS-ISS Only.
- The DAHS with ISS Directory is intended to reflect entities licensed as just a DAHS, and entities licensed as DAHS with ISS.
- At this time, this particular directory lists all entities as just having a DAHS license. This is because the commission has yet to approve any DAHS with ISS licenses. The process for approving a DAHS with ISS application takes longer than that of a provider applying as an ISS-only entity. According to HHSC, the entity must undergo an LSC and Health survey before a license is issued to a DAHS with ISS entity. Once these have been approved, they will be listed in this directory as DAHS with ISS.
- Entities listed in the DAHS – ISS Only Directory, currently reflect a 6-month license. This is because these licenses are considered ‘temporary’ at this time. Once the health survey is conducted the entities will receive a one, two or three-year license.
February 5th, 2023
HHSC LTCR Updates the ISS FAQ’s
HHSC Long-term Care Regulation updated the Individualized Skills and Socialization frequently asked questions document on Feb. 01, 2023.
January 27th, 2023
FYI- somehow I missed this alert back in November for Licensed ISS providers. Please be sure to log in and set up your account.
PL 22-32 letter issued 11/28/22 to ISS providers that was sent out concerning Blackboard Connect Emergency System
The purpose of this letter was to inform providers of the emergency communication system called Blackboard Connect, how it will be used, and your responsibility in signing up for the system if you are an ISS provider. This system will be used to send emergency and outreach notifications through email, phone, voice and text if available.
The rules require program providers to assign a designee to enroll in and respond to requests through the system. The designee should be someone who is associated with the licensed building or someone who is responsible for communicating emergency communications. However, you may also have other designees, such as corporate headquarters staff, sign up.
Blackboard Connect sign-up process:
Go to this link and click “Sign Me Up!”
If you have any questions, please contact the Policy and Rules Section by email at LTCRPolicy@hhs.texas.gov or call (512) 438-3161.
Rember, this also applies to HCS, TxHmL and ICF providers among other services.
January 16th, 2023
- The ‘new’ IPC referenced in IL 2022-03 will most likely not be ready until March. They did not have answers as to what providers should do in the interim or even how service logs should be revised until new ones are available. (The letter does indicate that those individuals receiving DH at the time of the switch to ISS (March 1st, 2023) will initially roll over automatically to ISS ).
- After Feb. 28th this would apply to all current clients as far as IPC units are concerned. Persons who don’t have any Day Hab units/days on their plan as of Feb. 28th, 2023 and want ISS hours, will have to do a new PDP and request IPC hours. Providers will have a new IPC form, with ISS on it, before March 1st, 2023.
- To date, no provider has been issued an ISS license.
- Providers can confirm that an entity has an ISS license by checking the DAHS directory on the DAHS webpage: https://www.hhs.texas.gov/providers/long-term-care-providers/day-activity-health-services-dahs
ISS FAQs and Upcoming Webinars:
On January 26, 2023, from 9:00 to 10:30 HHSC will conduct its quarterly LTC webinar which will focus on ISS. To register for the webinar, go to: https://register.gotowebinar.com/register/5204373791714060639
January 12th, 2023
Information Letter No. 2023-03 Individualized Skills and Socialization Automatic Service Authorizations
Effective January 1, 2023, individualized skills and socialization became an available service in the HCS and TxHmL Programs. For the time period of January 1, 2023 to February 28, 2023 both day habilitation and individualized skills and socialization will be allowable program services.
Day habilitation will no longer be a Medicaid-billable service in the HCS or TxHmL Programs for dates of service beginning March 1, 2023, and ongoing.
On January 9, 2023, HHSC will automatically add units of individualized skills and socialization for all individuals with day habilitation (including individuals receiving in-home day habilitation through the COVID-19 flexibility) currently authorized on their individual plan of care (IPC). The units will be available for billing immediately for the provision of on-site, off-site, or in-home individualized skills and socialization and will be visible to program providers in the Medicaid Eligibility Service Authorization Verification (MESAV). The added units will be authorized beginning January 1, 2023 through the end of the individual’s current IPC period. For individuals with an IPC period that must be renewed between January 1, 2023 – April 30, 2023, the added units will be authorized until December 31, 2023.
These units for individualized skills and socialization will not be visible to program providers or service coordinators on the IPC in the Long-term Care Online Portal (LTCOP) on the Texas Medicaid & Healthcare Partnership (TMHP) website nor on the dashboard until a revision or renewal IPC is entered. This automatic service authorization will give service coordinators additional time to meet with the individual’s service planning team (SPT) to update the individual’s person-directed plan (PDP) and for program providers to update the individual’s implementation plan (IP) as this new service takes effect. HHSC is implementing this process to minimize disruption to an individual’s desired services.
Service Plan Revisions
At the individual’s next service planning team meeting to complete a revision or renewal IPC (whichever occurs first) for individuals receiving individualized skills and socialization, service coordinators should update the individual’s PDP to reflect the new individualized skills and socialization service. During the service planning team meeting, any new goals related to the provision of on-site and off-site individualized skills and socialization should be discussed and documented in the new action plan. Until the PDP is updated, the individual’s current day habilitation goals, frequency, and duration should be followed for the individualized skills and socialization service.
Following the update to the PDP, the IPC and IP must be updated in accordance with applicable HCS or TxHmL Program rules with the appropriate units of individualized skills and socialization. HHSC will update the IPC and IP form to add individualized skills and socialization by March 1, 2023.
All individual’s PDPs, IPCs, and IPs must be updated with the appropriate units of individualized skills and socialization in accordance with applicable HCS or TxHmL Program rules by December 31, 2023.
For new enrollees and current enrollees who are not currently receiving day habilitation, individualized skills and socialization will need to be added, once the IPC and IP form have been updated, to the individual’s service plan because units will not be auto-authorized for these individuals. Day habilitation can be added and delivered until February 28, 2023.
To read more, please click on link below, for Information Letter 2023-03 related to ISS automatic service authorizations and EVV
January 3rd, 2023
Easier Format For ISS Licensing Rules effective Jan. 1, 2023
The link below provides a format that is easier to read and understand the newly adopted licensing rules rather than those when published as adopted in the Texas Register
Effective Jan. 1, 2023, HHSC adopts new Individualized Skills and Socialization rules for providers who want to deliver individualized skills and socialization services. New rules provide guidance regarding:
- applying for an Individualized Skills and Socialization license;
- provider requirements; and
- HHSC survey and enforcement actions.
Read the new rules in Title 26 of the Texas Administrative Code, Chapter 559, Subchapter H.
HHSC also published Provider Letter 2023-01 New Regulatory Rules for Long-term Care Regulation (LTCR) Individualized Skills and Socialization Services. This PL provides guidance to Individualized Skills and Socialization providers about the new rules.
Read PL 2023-01.
December 23rd, 2022
NEW RULES FOR ISS & ISS LICENSE
HHSC Adds Individualized Skills and Socialization to Email and Text Updates
HHSC added an option to the HHSC email and text update GovDelivery system that subscribers can select to receive updates related to the Individualized Skills and Socialization services program. Users can select to receive Individualized Skills and Socialization program alerts from the “Provider Alerts” drop-down menu.
To sign up for updates, select this link Texas Health and Human Services Commission (govdelivery.com).
For questions about Individualized Skills and Socialization, please email LTCRPolicy@hhs.texas.
November 28th, 2022
Webinar for New Licensing Process Nov. 30th, 2022 Extended to 2 hrs
All providers interested in the new licensing process for the Day Activity Health Services Individualized Skills and Socialization program are invited to a 2-hour webinar on Nov. 30. Originally it was a 1 hr session but has now been extended to have enough time for questions and explanations.
HHSC Long-Term Regulation staff will discuss how to navigate TULIP, the licensing system, explain the license application process and provide an overview of the survey process. There will also be a Q&A session as time allows.
Register for the webinar: Licensing Process Webinar
November 19th, 2022
DAHS ISS Licensing Application Available!
On Dec. 1, 2022, HHSC will launch the Day Activity Health Services (DAHS) Individualized Skills and Socialization License Application in the Texas Unified Licensure Information Portal (TULIP).
Link to TULIP: https://txhhs.force.com/TULIP/s/
Email TULIP_Support@hhsc.state.tx.us with questions related to TULIP functionality or if you have issues gaining access.
Email LTC_NF_DAHS_Licensing@hhs.texas.gov with questions related to the DAHS Individualized Skills and Socialization licensing application
October 13th, 2022
Licensing Application Process For ISS:
October 2nd, 2022
Register for Individualized Skills and Socialization Provider Portal Trainings
Individualized Skills and Socialization Provider applicants are required to complete HHSC Individualized Skills and Socialization Provider Trainings. Below are two computer-based trainings, which will assist Individualized Skills and Socialization Providers with applying for a license and preparing for an inspection.
- Prelicensure Training for Individualized Skills and Socialization Providers
This training was designed for providers who wish to offer individualized skills and socialization services. Prior to surveys or inspection, an entity must submit an application for a Day Activity and Health Services license. Information about the requirements to obtain a license will be shared. Register for the training. - Preparing for an Inspection
This training was designed to assist Individualized Skills and Socialization Providers to prepare for an inspection. In this course, information about the inspection process and licensure rules will be shared. Register for the training.
September 24th, 2022
HHSC Moved The Individualized Skills and Socialization Webpage
The Individualized Skills and Socialization webpage moved from the Resources webpage to the main Long-term Care Providers webpage. This was done so its location is consistent with other Long-term Care Regulation programs and is easier to find.
Individualized Skills and Socialization can be found under the “Community-based Programs” heading.
August 23rd, 2022
No Public Hearing on ISS Licensing Rules
Comments must be submitted no later than 31 days after the date the rules were published in the Texas Register; i.e., 31 days after August 12, 2022.. Comments must be (1) postmarked or shipped before the last day of the comment period; (2) hand-delivered before 5:00 p.m. on the last working day of the comment period; or (3) emailed before midnight on the last day of the comment period. If the last day to submit comments falls on a holiday, comments must be postmarked, shipped, or emailed before midnight on the following business day to be accepted. When emailing comments, please indicate “Comments on Proposed Rule 22R050” in the subject line.
Public Hearing on ISS Program Rules
HHSC will conduct a public hearing on the proposed HCS, TxHmL and DBMD ISS program rules on September 7, 2022 from 8:00 am. until Noon. To register for the virtual hearing, go to: https://attendee.gotowebinar.com/register/927810115195515152
For a copy of the proposed ISS license rules or go to: https://www.hhs.texas.gov/regulations/policies-rules/health-human-services-rulemaking/comment-proposed-draft-rules
August 13th, 2022
Texas HHSC has developed the Individualized Skills and Socialization Provider Portal, an online source of information for providers of individualized skills and socialization.
The Individualized Skills and Socialization Provider Portal will allow providers to:
- Complete and review trainings on the Individualized Skills and Socialization service.
- Find and review provider letters and other information and releases related to Individualized Skills Socialization.
- Link to rules and other services related to Individualized Skills and Socialization.
Provider Communications
- PL 2021-42 – This Provider Letter offers a brief introduction to the new individualized skills and socialization service and what providers can expect as HHSC implements the service.
- Individualized Skills and Socialization Services webinar – This helpful webinar provides an introduction and overview to Individualized Skills and Socialization
- Individualized Skills and Socialization FAQs – revised April 26, 2022
- July 2022 – Individualized Skills and Socialization Provider Webinar – This webinar covers the service description, ratio requirements, and licensing information based on HHSC’s draft individualized skills and socialization rules.
August 6th, 2022
See Draft/Proposed Rules for ISS in HCS and TxHmL below:
Proposed ISS Rules (Main portion of rules start on page 13-52)
- The anticipated adoption date is October, 2022 with an effective date of November 2022. These dates also apply to the proposed rules for the DBMD waiver program.
- Very few changes were made from comments HHSC received during the informal comment period earlier this year. Though we had been apprised of such before this positing, know that any comments you submitted during the informal comment period will need to be resubmitted.
- Carefully review the introduction to the HCS and TxHmL rules on pages 1 -4, including the sections on Issues and Alternatives and Stakeholder Involvement on page 3.
- Carefully review the preamble to the rules before reading the actual rules and pay attention to the sections on Impact to Small Businesses.
- The proposed HCS and TxHmL rules are included in one document. To help you navigate the document, the following is offered:
Reminder about New Long-Term Care Regulation Training Registration From HHSC
September 10th, 2025
“From HHSC”
HHSC has announced that registering for Joint Training will be easier and more efficient through our new Learning Management System (LMS), Learning Tree. Long-Term Care Regulation (LTCR) Joint Training began using the LMS for training registration on Sept. 1, 2025.
What is the Learning Tree LMS?
- A user-friendly online platform designed to enhance your learning experience.
- Centralizes course registration and access.
You’ll need an account to register for in-person trainings or virtual webinars. For those looking for modern therapeutic approaches, check out here for more info.
How do I register for an Account?
Step 1: Create an Account
- Navigate to the Registration Link.
- Fill in the required information:
- First Name, Last Name – Formatted as it would appear on any training certificates.
- Email Address – It’s important to obtain your certificates in your Completed Courses. We recommend using your personal email address. This will also be your username.
- Cell Phone – This is not required.
- Select the correct Affiliation for your account or role.
- Select the Register button to create your account on our system.
Step 2: Create a New Password
After registering for an account, you will be taken to a new screen to reset your password. Passwords created in the Learning Tree LMS must include:
- Minimum of 8 characters
- Maximum of 12 characters
- 1 uppercase letter
- 1 lowercase letter
- 1 number
- 1 special character
Special Characters include: ~!@#$%^&*_-+=’|(){}[]:;”<>,.?/
Step 3: Register for Training
After you reset your password, you’ll be re-directed to your Learner Dashboard.
- Select Register for Course on the left navigational pane.
- Locate the course you are signing up for.
- If you know the name of the training you’re looking for you can also type it in the search bar at the top. Press <Enter> on your keyboard or Find Course to search, and the course should appear.
- Click Register.
- Click Proceed to Checkout.
- Click Confirm.
- Click Go to Dashboard.
Courses are free of charge unless otherwise noted.
Transition Support Teams: 8 LIDDA’s Provide These Resources
September 3rd, 2025
Individuals that reside in institutions such as a nursing facility, state-supported living center (SSLC), or intermediate care facilities, who have IDD often have many significant medical, psychiatric, and behavioral needs that create challenges to living successfully in the most integrated community setting. Serving individuals who transition or divert from these institutions often requires specialized staff, intensive training, and expertise across several fields of study as well as ongoing support and technical assistance. As these individuals transition to an HCS program, for example, providers and family members have a difficult time finding the needed support for their individual in the community, particularly in rural areas, to maintain the care they need.
The Texas Health and Human Services Commission (HHSC) secured Money Follows the Person (MFP) Demonstration funding to help individuals who have complex medical and behavioral needs and want to live or remain in the community to receive the services and supports they need.
Texas has 8 regional Transition Support Teams (TSTs), often referred to as Hubs, to serve all 254 Texas counties, including all 39 local intellectual and developmental disability authorities (LIDDAs) and the community waiver providers within a designated region. These interdisciplinary teams provide the following support services:
- Educational and training activities and materials, such as webinars, videos, and other correspondence, are provided at least quarterly and focus on increasing the expertise of LIDDAs, providers, and community members in supporting individuals with complex needs.
- Technical assistance provided to LIDDAs, program providers, and other community support services on specific disorders and diseases, emerging and best practices, and evidence-based services for individuals with significant challenges.
- Case consultations and peer reviews are provided to service coordinators, crisis intervention staff, direct care staff, and other members of an individual’s service planning team who need assistance providing effective care for an individual.
A licensed professional, such as a clinical social worker, serves as each TST coordinator. TSTs include licensed medical staff such as physicians, physician’s assistants, nurse practitioners, and registered nurses as well as psychiatrists, psychologists, behavioral specialists, and other professionals who have expertise working with individuals with IDD. These interdisciplinary teams support the LIDDAs and service providers within their designated service areas.
TSTs are also designed to address unique regional and cultural issues and challenges as well as identify gaps in medical, psychiatric, and behavioral resources. They report information about these identified gaps to Texas HHSC.
| Designated LIDDA | Covered LIDDA Service Areas |
|---|---|
| Alamo Local Authority for IDD | Alamo Local Authority for IDD Camino Real Community Services Gulf Bend Center Hill Country MHDD Centers |
| Behavioral Health Center of Nueces County | Behavioral Health Center of Nueces County Border Region Behavioral Health Center Coastal Plains Community Center Tropical Texas Behavioral Health |
| Emergence Health Network | Concho Valley Center for Human Advancement Emergence Health Network Permian Basin Community Centers West Texas Centers |
| Integral Care | Bluebonnet Trails Community Services Central Counties Services Heart of Texas Region MHMR Center Integral Care MHMR Authority of Brazos Valley |
| Metrocare Services | ACCESS Andrews Center Burke Community Healthcore Denton County MHMR Center Lakes Regional Community Center LifePath Systems Metrocare Services Spindletop Center Texoma Community Center |
| My Health My Resources of Tarrant County | Betty Hardwick Center Center for Life Resources Helen Farabee Centers My Health My Resources of Tarrant County Pecan Valley Center for Behavioral and Developmental Healthcare |
| StarCare Specialty Health System | Central Plains Center StarCare Specialty Health System Texas Panhandle Centers |
| Texana Center | The Gulf Coast Center The Harris Center for Mental Health and IDD Texana Center Tri-County Behavioral Healthcare |
If you need help to locate offices that can help you with intellectual or developmental disabilities, aging, behavioral health, and other disability services, please visit Where Can I Find Services?
HHSC: HCS Amendment To Rates Effective Sept. 1, 2025-Update
August 30th, 2025
CMS has approved the 1915 (c) waiver amendments with an effective date of September 1, 2025. This means that the rates funded by Rider 23 and posted by HHSC on August 19, 2025 will be effective September 1, 2025.
Copy of Information Letter 2025-17 and link to approved rates – https://www.hhs.texas.gov/sites/default/files/documents/il2025-17.pdf
August 15th, 2025
In September 2025, Texas will see changes to HCS (Home and Community-based Services) rates, including the discontinuation of the Attendant Compensation Rate Enhancement program and increased rates for identified attendant services. These changes are tied to the 2026-27 General Appropriations Act, specifically Rider 23
-
Discontinuation of Attendant Compensation Rate Enhancement:
The current program will end, effective September 1, 2025.
-
Rate Increases for Attendant Services:
HHSC will propose increased rates for certain attendant and attendant-like services, also effective September 1, 2025.
-
Funding for Wage Increases:The 2026-27 General Appropriations Act, Rider 23, provides funding for HHSC to increase the wage for personal attendants to $13.00 per hour and adjust related payroll costs.
June 21st, 2025
HHSC is accepting comments on the amendment of the 1915(c) Home and Community-based Services Waiver. View the HCS amendment details.
Through this amendment, HHSC updated the attendant rates and increased the HCS individual cost limits. The cost limits were updated as described below:
-
Intermittent (LON 1), Limited (LON 5), and Extensive (LON 8)
-
The amount is going from $167,468 to 210 percent of the annualized cost of care in an Intermediate Care Facility for Individuals with an Intellectual Disability or Related Condition (ICF/IID) using the fiscal year 2026 non-state-operated small facility daily rate for Level of Need (LON) 8, rounded to the nearest dollar, which is estimated to be $169,182 pending finalization of the fiscal year 2026 rates for ICFs/IIDs.
-
-
Pervasive (LON 6):
-
The amount is going from $168,615 to 210 percent of the annualized cost of care in an ICF/IID using the fiscal year 2026 non-state-operated small facility daily rate for LON 6, rounded to the nearest dollar which is estimated to be $211,822 pending finalization of the fiscal year 2026 rates for ICFs/IIDs.
-
-
Pervasive plus (Level of Need 9):
-
The amount is going from: $305,877 to 210 percent of the annualized cost of care in an ICF/IID using the fiscal year 2026 non-state-operated small facility daily rate for LON 9, rounded to the nearest dollar which is estimated to be $392,318 pending finalization of the fiscal year 2026 rates for ICFs/IIDs.
-
Comments will be accepted until July 21, 2025.
Email comments to the Texas Medicaid Waivers inbox.
HCS Home Page, Provider Letters, Contacts and Resources (Update)
July 28th, 2025
Home and Community-based Services (HCS)
Provider Letters/Provider Communications!!!
Click here for news, information letters (ILs) & provider letters (PLs).
To receive provider letters & communications for HCS/TxHmL/ICF/ISS or other HHSC programs, please go to GovDelivery signup from Granicus at:
https://service.govdelivery.com/accounts/TXHHSC/subscriber/new
Remember to only sign up for the alert letters and communications for the programs that apply to you or that you would like to receive information about!
Receive Emails from HHS Every Sunday
The Texas Health and Human Services Commission contracts with a company called Granicus to provide email updates, called GovDelivery. In accordance with your contract, and contracting rules at 40 Texas Administrative Code §49.302(g), you must subscribe to receive HHSC email updates, using this GovDelivery signup, and select Information Letters, Provider Alerts and the contract program type(s).
When you sign up for email updates, you are giving your information to both HHSC and to Granicus. When HHSC has your information, it is subject to the HHSC privacy policy. When Granicus has your information, it is subject to the Granicus GovDelivery privacy policy.
Contact Program Staff
- Provider/policy information: hcs@hhsc.state.tx.us / hcspolicy@hhsc.state.tx.us
- Contracting information: 512-438-3234 / IDDWaiverContractEnrollment@hhsc.state.tx.us
- Eligibility information: Your local authority
- Regional nurses: Community Services regional contacts for your region
Emergency Alert Communication System: AlertMedia
PL-2025-01
All HCS Providers must complete the following steps:
• Register your AlertMedia account using the steps provided in the Self Registration Guide.
Registration process:
Users will enter their contact information, provider choices, and set a password. Users will be sent an activation pin to enter. Once the user selects Submit, registration is complete.
Registration Page: https://texashhsc.alertmedia.com/public/v2?
• HHS will send a test alert. Please save that number to your phone to ensure receipt of future communication.
• Download the optional AlertMedia mobile app for iPhone or for Android to ensure the receipt of emergency-related messages.
Providers will receive a confirmation code to their email address after registration and should refer to the Self-Registration Guide for any questions regarding registration or troubleshooting.
*Note: PL-2025-01 contains the AlertMedia Self Registration Guide – Attachment A
Contact Information
Please reach out to RSDAlertMedia@partner.hhs.texas.gov with any questions.
Resources
Infection Control & Vaccine Resources
- Infection Prevention and Control Measures for Common Infections in LTC Facilities (PDF)
- Infection Control Basics & PPE Training for Essential Caregivers (PDF)
HB 3720
State Rules (Title 40 Subchapter D replace with Title 26 part I Ch 263 & 565)
- Texas Administrative Code, Title 26, Part 1, Chapter 263: Home and Community-based Services (HCS) Program and Community First Choice (CFC)
- Texas Administrative Code, Title 26, Part 1, Chapter 565: Home and Community-Based Services (HCS) Program and Community First Choice (CFC)
- Texas Administrative Code, Title 40, Part I, Chapter 41: Consumer Directed Services
- Texas Administrative Code, Title 40, Part 1, Chapter 49: Contracting for Community Services
Review Tools and Forms
- ISS Attestation and Provider Compliance Form (PDF)
- Form 1573, Residential Review Evidence of Correction for Results Less Than 90%
- Form 8576, Individual Profile Information
- Form 8608, Sample Appeal Letter
Additional Resources (Updated)
-
- HCS and TxHmL FAQs ROR CIMS Process (PDF)
- Provider and LIDDA CARE Report Crosswalk (PDF)
- Provider and LIDDA CARE Screen Crosswalk (PDF)
- Comprehensive Nursing Assessment FAQ (PDF)
- HCS and TxHmL Transformation Webinar (PDF)
- Interpretive Guidance Booklet (PDF)
- HCS Certification Principles Webinar Series Recordings
- Regulation of Individual Skills and Socialization webinar (PDF)
- Regulation of Individual Skills and Socialization webinar recording
- LIDDA Potential Threat DAC Memo (PDF)
- Summary of Employment Readiness Webinar Questions and Answers with Examples (PDF)
- PL 2020-55 Administrative Penalty Process for Home and Community-based Services (HCS) and Texas Home Living (TxHmL) Program Providers (PDF)
- HCS and TxHmL Certification Principle Trainings
- Listen to Module 1: Administrative Penalties recording
- Listen to Module 2: Mission, Development, and Philosophy of Program Operations recording
- Listen to Module 3: Comprehensive Nursing Assessment recording
- Listen to Module 4: Staff Member and Service Provider Requirements recording
- Listen to Module 5: Restraints and Seclusion recording
- Listen to Module 6: Quality Assurance recording
- Listen to Module 7: Rights of Individuals recording
- Listen to Module 8: Abuse, Neglect, and Exploitation recording
- Listen to Module 9: Service Delivery recording
**If you have any questions about any of these resources on this page or about the HCS program, email LTCR Policy and Rules or call (512) 438-3161.
PAT (Provider Applicant Test)-Update 2025 (HCS/TxHmL)
July 22nd, 2025
From HHSC’s PAT FAQ’s as of Jan. 1st, 2023
“Frequently Asked Questions for Providers Applicant Training (PAT) for HCS/TXHML”
-When is the Provider Applicant Training (PAT) and Test available?
This training is available online at this time (training modules). The PAT Test itself is being revamped and is not available to take until September of 2025.
If you are trying to apply for an HCS/TxHmL contract at this time, you will not be able to submit HCS/TxHmL applications without the PAT Test Certificate of Completion (must have passing grade of 85%), until you can schedule the test in September of 2025.
Beginning Sept. 1st, the training modules will still be available online, but applicants will no longer be able to take the test online!. Applicants will need to take the practice modules online and then schedule a time to take the test “in person”. We will keep you posted as to whether they will be available at various testing centers or at one specific location.
The PAT training is one of the first steps for HCS/TxHmL applicants to obtain a contract with HHSC.
Please do not submit your application without the PAT certificate that reflects a passing score of 85% or above.
-Who can take the training and test?
Applicants listed on Form 3681, Section 8.a and 8.b must complete the online PAT training. The Program Manager noted on this form, must complete the training and pass the test with an 85% or above.
See Texas Administrative Code Title 40, Chapter 49, Rule §49.204. You must provide a copy of HHSC Form 3681 along with your certificate of passing by at least 85% to HHSC. The program manager must be the person taking the PAT test.
-How can I access the HHS Learning Portal?
• HHS Learning Portal (texas.gov).
• Set up your new account. You will need to confirm your new account through the email address used.
• Find and select the Medicaid Long Term Services and Support Training under “Course Categories.”
• Select the Provider Applicant Training (PAT) link. Select “Enroll me” to access the Training and get access to the “Welcome” page.
The training is compiled in four different steps.
Step 1. Important to know Before you Get Started
Fill out the Provider Applicant Training (PAT) Information form. This form must be completed to access the introduction and the training modules.
Step 2. Training Modules
Complete each module must be completed to advance to the next module.
Step 3. Evaluation and Certificates
Complete the mandatory survey
Step 4. Provider Competency Exam
Schedule your test with HHSC, after you have completed training modules. Please save your exam certificate upon completion of test. HHSC will issue you your results. Submit the certificate along with your completed application
IMPORTANT: You must take the PAT before you can apply to be an HCS Provider!!!. You must pass the Test by 85 % If you fail the test, you can’t retake the test for a period of 6 months, so please study the TAC before and pay careful attention to the PAT modules before answering test questions.
Note: If you do not pass on your first attempt, please DO NOT apply.
HCS and TxHmL Quarterly Webinar Scheduled for August 28th, 2025
July 23rd, 2025
Program providers and other interested stakeholders can now register for the upcoming HCS and TxHmL quarterly webinar.
HCS and TxHmL Quarterly Webinar
August 28, 2025
10:00am-12:00pm
Register here for the August 28 HCS-TxHmL Quarterly Webinar
Webinar topics include:
- Form Updates
- TMHP: Claims Data Export & Enrollment Form Processing Enhancements for HCS and TxHmL
- Level of Need Submission Requirements and Resources
- EVV Required Services and Documentation
Email questions about the webinar to your program policy mailbox:
Statewise Provides Free EVV Compliance Checklist For Texas
July 22, 2025

From our friends at Statewise:
7 essential steps to EVV compliance, as well as Pro Tips are provided in this free checklist from Statewise.
“At Statewise, we’ve made it easier for providers like you to stay on top of your responsibilities with a free EVV Compliance Checklist—designed specifically for Texas Medicaid agencies.”
Texas EVV Compliance Checklist Free
Discontinuation of Attendant Compensation Rate Sept. 1st, 2025
July 22nd, 2025
Attendant Rate and Cost Limit Revisions Webinar on July 22
HHSC will be providing updates to Home and Community-based Services (HCS) and Texas Home Living (TxHmL) providers, and local intellectual and developmental disability authorities (LIDDAs) on the topic of attendant rate and cost limit revisions for the waivers. Attendant Rate and Cost Limit Revisions Webinar July 22, 2025 2–3 p.m.
Register here for the webinar. Run a test of your computer’s connectivity if you have never attended a webinar from your computer. You can run this test at any time before the date of the webinar. Perform this test early to allow time to address any technical issues.
Email tx_medicaid_waivers@hhs.texas.gov with any questions.
July 16th, 2025
The Health and Human Services Commission (HHSC) will be proposing increased rates for identified attendant services and discontinuing the Attendant Compensation Rate Enhancement (Rate Enhancement) program, effective September 1, 2025. These increases are pursuant to the 2026-27 General Appropriations Act, Senate Bill 1, 89th Legislature, Regular Session, 2025 (Article II, HHSC, Rider 23).
Please pay special attention to the cost reporting guidance in this provider letter.
* Public notices will be published in the Texas Register, which can be accessed on the Texas Secretary of State website.
The Proposed Rate Packet and other information will also be published on the HHSC PFD website.
Lastly, HHSC will be issuing GovDelivery alerts. To begin receiving these alerts, visit the GovDelivery site, select Medicaid Reimbursement Rates and Non-Medicaid Reimbursement Rates as preferences, and enter the requested information.
Please contact the HHSC PFD, Long-term Services and Supports Center for Information and Training Team, if you have questions regarding this provider letter at PFDLTSS@hhs.texas.gov or (737) 867-7817.
Note From Twogether Consulting: From what we understand, essentially the increased rates will help those HCS providers who do not already receive the Attendant Compensation Rate Enhancement (ACRE), but it will be a “wash” for those who currently participate in this rate enhancement. (Although it is not nearly the increase that was wanted and needed to support residential services in particular.) So, what it sounds like, is that those providers who receive ACRE currently would make about the same amount without ACRE, when the increased rates go into effect Sept. 1st, 2025. We have however, been hearing from many providers that they feel that from their calculations, they may actually lose money with the rate increase and loss of ACRE.
Discontinuation of the Attendant Compensation Rate Enhancement Program and Rate Increases for Attendant Services
June 30th, 2025
HHSC Publishes IL-2025-11
HHSC will propose increased rates for identified attendant services and discontinue the Attendant Compensation Rate Enhancement program, effective Sept. 1, 2025.
These changes are pursuant to the 2026-27 General Appropriations Act, Senate Bill 1, 89th Legislature, Regular Session, 2025 (Article II, HHSC, Rider 23).
HHSC has published Information Letter (IL) 25-11, Discontinuation of the Attendant Compensation Rate Enhancement Program and Rate Increases for Attendant Services, effective Sept. 1, 2025. Review the IL for more information.
If you have further questions, contact the HHSC PFD, Long-term Services and Supports (LTSS), Center for Information and Training (CIT) at PFD-LTSS@hhs.texas.gov or (737) 867-7817.
Rate Packets Now Available: For HCS/TxHmL/ICF/CFC/HCBS-AMH Waivers
June 30th, 2025
Rate Packets Now Available
The rate hearing packets were posted on the PFD website on June 23, 2025. The hearing is being conducted to receive public testimony on the proposed Medicaid Rates.
Public Rate Hearing on July 16, 2025
The HHSC Provider Finance Department (PFD) Long Term Services and Support (LTSS) will hold its Public Rate Hearing on July 16, 2025, to address proposed rates for the following:
- Medicaid and Non-Medicaid Payment Rate Actions for Attendant Services in various programs, and
- Medicaid Payment Rate Actions for Nursing Facilities (NFs) and Nursing Facility Special Reimbursement Class for Individuals with Intellectual and Developmental Disabilities (IIDs).
Session One: 9:00–10:45 a.m. CDT
Session Two: 11:15 a.m.–1 p.m.
Session Three: 2:00–3:45 p.m.
This rate hearing will be conducted both in person and as an online event. Register for the hearing to attend this online meeting. After registering, you will receive a confirmation email containing information about joining the webinar.
You can also dial in on your phone. To do so, follow the link above to register. You will then be provided dial-in instructions, including an audio PIN. The audio PIN must be entered to speak over the phone audio during the hearing.
Public Notice and Testimony
The notice for the rate hearing was published in the June 20, 2025, issue of the Texas Register and posted to the HHSC website on June 11, 2025. Unless otherwise noted in the notice and the rate hearing packets, written comments regarding the proposed payment rates may be submitted instead of, or in addition to, oral testimony until 5 p.m. (CDT) on the day of the hearing. Written comments may be sent by U.S. mail, overnight mail, special delivery mail, fax, or email, as follows:
U.S. Mail:
Texas Health and Human Services Commission
Attention: Provider Finance, Mail Code H-400
P.O. Box 149030
Austin, Texas 78714-9030
Overnight mail or special delivery mail:
Texas Health and Human Services Commission
Attention: Provider Finance, Mail Code H-400
North Austin Complex
4601 Guadalupe St.
Austin, Texas 78751
Phone number for package delivery: (512) 730-7401
Fax:
Attention: Provider Finance at (512) 730-7475
Email:
Long Term Support Services – PFD-LTSS@hhs.texas.gov
Persons with disabilities who wish to participate in the hearing and require auxiliary aids or services should contact Provider Finance at (512) 730-7401 at least 72 hours before the hearing so appropriate arrangements can be made.
Preferred Communication
If possible, use email or phone for the quickest response to communicate with HHSC about this rate hearing.
Forward this information to providers and organizations in your programs as appropriate. If you have any questions about this rate hearing, email PFD LTSS.
Twogether Consulting’s Satisfied Customer Page
June 26th, 2025
We would greatly appreciate a quote from any of our clients who would like to write up a short paragraph on how we may have helped your organization or any recommendations you have for others about our services at Twogether Consulting that you may have used over the years. We are also happy to accept updates to previous satisfied customer quotes that are currently posted on the site.
Link to Satisfied Customers Page
If you would like to send us a quote, feel free to email us at info@twogetherconsulting.com
Note: Please type Satisfied Customer Quote in the subject line. Be sure to leave your full name, company name, and title. You are also welcome to leave a website link or email if you would like.
Twogether Consulting Newsletter Library

Subscribe To The Twogether Consulting Mailing List!
2025
April 17th, 2025-correction/addendum
2024
To Read previous newsletter editions from 2023, please click here

If you would like to be on our mailing list for this free publication, please click here to subscribe through Mailchimp for the newsletter subscription or if you prefer, you may click on our website link for newsletter subscription
TMP Merger With Cubhub: Rebranded as Statewise
June 26th, 2025
![]()
What Providers Need To Know
“TMP has joined Cubhub as part of the Statewise family—but nothing’s changing for Texas providers. TMP remains your trusted platform for IDD services.”
Important: What’s changing?
Just the name of the platform (From TMP to Statewise). With the support of Cubhub, TMP will get stronger and gain improved features, but it will continue to serve as the primary platform for Texas-based IDD and personal care providers. You will continue using the TMP platform as you know and trust, and the support team will remain the same.
For more information: https://statewise.com/blog/what-providers-need-to-know-as-tmp-merges-with-cubhub
Press Release: In Dallas, Texas, as of June 16th, 2025
More than a name change, the move to Statewise marks a bold step forward—focused on equipping Medicaid-based providers with the tools, insights, and support they need to deliver exceptional care across every state. The company has plans to expand features and refine modules alongside its partner companies to meet the challenges of a market that is undergoing seismic changes.
ICF Provider 2024 Conference Recordings Available For Viewing
June 25th, 2025
In case you were not aware, and you missed last year’s conference, we wanted to make sure ICF providers knew they could still watch the sessions. Great For your Q’s, Administrators, and QA staff.
HHSC Long Term Care Regulation has posted 4 recorded sessions from the 2024 ICF Conference “Embracing Change to Enhance Value” held Dec. 5, 2024.
No CEs or certificates of attendance are offered for viewing these recorded sessions.
iCareManager EHR System Information
June 25th, 2025

From iCareManager email received on June 25th, 2025
“We are thrilled to introduce you to the innovative & efficient iCareManager
All-In-One EHR Solution!
Whether you connected with us at a conference or online, you’ve just taken the first step towards smarter, simpler, and more efficient IDD service delivery.
To kick things off, we’re attaching our 2025 e-book. It will give you a complete overview of who we are, what we offer, and how our EHR system is built to make life easier for IDD service providers.”
| Download e-Book For FREE |
What Sets iCM Apart From Others?
- A Completely User-Friendly Dashboard
- SOC 2 & HIPAA Certification
- Holistic Solution To All Service Provision Needs
This is just the beginning, and we’re here to support you every step of the way
iCareManager, 6103 Parkway Dr, Laurel, MD 20707, United States
You may unsubscribe or change your contact details at any time.
Free IDD Provider Resource Webinar Series
Free Webinars!!
June 22nd, 2025

Here Are Just Some Of Our Previously Recorded Free Webinars of Interest
Please see all recordings of previous webinars on our Gotostage Channel

Core-VA Solutions “Virtual Healthcare Assistants For LTC Programs”
Virtual Healthcare Assistants Services and Training for Long-Term Care Programs, including HCS, TxHmL, and ICF
Twogether Consulting is happy to have Brittney Russo-COO (Chief Operations Officer) from Core-VA Solutions to discuss her company’s “virtual assistant” services.
Core-VA Solutions provides virtual assistance for any type of long-term healthcare setting, whether it be for a small medical office or therapy office or HCS provider. All of our virtual assistants have a degree in nursing and/or health-related fields.
Core-VA is able to serve clients all over Texas and beyond. Some of the clients these virtual assistants work with are those in HCS, TxHmL, and also other IDD programs. This includes assisting with EVV and TMHP billing. Brittney’s team is able to provide appropriate training to her staff to cater to some of your specific needs, including persons with experience in the HCS/TxHmL programs providing some of that training and the IT solutions which they can learn to use using IT fundamentals here to learn for this. They have “virtual assistants” versed in the use of quite a few electronic health records software such as Taskmaster Pro, Focus, and other EHR and billing software. This is a wonderful resource for HCS/TxHmL providers for sure! This is especially true for some of you, who are brand-new HCS/TxHmL providers. Core-VA serves many different clients in other lines of Long-Term Health Services, but it is so nice to have help from a virtual assistant who understands the world of HCS/TxHmL!
-Core-VA team Solutions is part of our free webinar series for the month of January 2023! Click on their postcard below for more information. Services are available at $10-12/hr and no contracts.
core va post card
“Core-VA Solutions aims to positively change how your long-term healthcare facility operates with our virtual assistants with degrees in nursing and/or health-related fields. We understand that you may currently waste precious time and money completing tedious tasks such as medical reception, appointment scheduling, insurance authorization, receiving and submitting medical information, and so much more. Instead of hiring expensive employees to complete these much-needed tasks, hire our affordable virtual assistants instead, as we can provide you with the same level of service, at a fraction of the price. All you have to do is let us know how we can help, and our team will find the perfect assistant match for your facility!”
“Support & Empowerment Program For Persons With IDD & Their Caregivers”
Twogether Consulting is happy to have Diana Chavarria from AACOG discuss an amazing program offered via a grant from TCDD (Texas Council For Developmental Disabilities). This is a wonderful resource for IDD providers, Caregivers of persons with IDD and persons with IDD. Dianne is part of our free webinar series for the month of January 2023!

The Program Provides Support & Empowerment For Individuals and Their Caregivers Concerning The Following:
-General Health and Aging
-Aging With Specific Syndromes (i.e. Down Syndrome)
-Nutrition & Physical Fitness
-Financial Wellness
-Benefits and Employment
-Planning For The Future
-Mental Wellness
-Coping With A Diagnosis
-Crisis Management
Here is a link to a short, introductory video about the HRST: https://hrstonline.com/video/index.php?id=410335893
Topic: Health Risk Screening Tool
HRST (Health Risk Screening Tool) is an assessment tool that can identify & detect health risks in vulnerable populations. This tool and other services offered by HRS are based on person-centered practices. Here is a little more information about HRS from their website. The Health Risk Screening Tool (HRST) identifies and tracks health risks in vulnerable populations, making it possible to design a plan tailored to meet the unique health and safety needs of each individual in the least restrictive setting. The instrument can objectively justify resources allocated both financially and in service intensity. Used by Case Managers, supervisors, and direct support professionals. HRS also helps the provider to comply with CMS Rules and assist with Person-Centered planning and continuity of care. It is field-tested, reliable, and user-friendly
“Health Risk Screening, Inc.’s roots began in 1992. Along with training courses, webinars, and materials, HRS is the sole developer, producer, and distributor of the web-based Health Risk Screening Tool (HRST). The HRST is the most widely used and validated health risk screening instrument for people with intellectual and developmental disabilities.
HRS was established on the principles of person-centered practices. Our founder, Karen Green McGowan was a pioneer in the early formative days of the person-centered movement.. Our focus is on developing tools and training for the person-centered support of vulnerable populations. Through the education of government agencies and service providers, we have helped improve people’s lives. Along with training courses, webinars and materials, HRS is the sole developer and distributor of the web-based Health Risk Screening Tool (HRST). The HRST is the most widely used and validated health risk screening instrument for people with disabilities.”
For more information, please contact Hillary Gaytan at: Phone: 727.754.9539 Email: hilary@hrstonline.com
You can also go to their website: www.hrstonline.com
Check out this great page they have devoted to COVID-19 Resources: https://hrstonline.com/covid-19-resources/

Guest presenter:
Patrick Lane (PCT Mentor & Trainer)
From: HRS
Date: Thursday -November 12th, 2020 (Session ended)
Where: See recorded link below:
https://attendee.gotowebinar.com/recording/1049673375643527182
Topic: Person-Centered Services
Patrick will be talking about some of the Person-Centered Services offered at HRS including software that helps the provider develop Person-Centered Descriptions. These can be used as a resource for making annual plans Person-Centered by using these same person-centered skills practiced in PCT sessions.
“Person-Centered Planning Training is designed to help you approach support from a more holistic angle, with person-centered practices that respect the autonomy of those with intellectual and developmental disabilities while providing them with the highest possible level of care.”
Improve The Quality of Life
- Balancing personal choice with personal responsibility by establishing and maintaining things that are important to the person with things that are important for the person
- Being integrated in one’s community so that the person is known and respected for her or his contributions.
- Being respectfully communicated with as a person, using language consistent with being a typical adult as opposed to using clinical or system language
- Receiving support that is consistent so that new staff and others know and respect the person’s values and choices, as well as how others can help the person.
- Being matches with staff, housemates, or others that the person making life more enjoyable.
You can contact Patrick at: patrick@hrstonline.com For more info about HRS PCT services, please see the following link: https://hrstonline.com/person-centered-services/
Guest presenter:
Steve Cardie
From: Abundant Health
Date: Tuesday -November 17th, 2020 (Session ended)
Where: See link to the recorded session below:
https://attendee.gotowebinar.com/recording/5931551182568587528
Topic: Cellular Blood Pressure Monitoring System (Free To Medicare Patients!)
“Our new Cellular Blood Pressure Monitor System connects automatically to cell towers and transmits your patient’s information directly to your practice. This device makes it simple for seniors who tend to be more technology challenged to utilize Medicare’s RPM program without the difficulty of connecting to cell phones or the internet. No passwords, no Bluetooth, no internet connections required.
The rapid advance of medical device design plus an enormous upgrade in telecommunications makes Remote Patient Monitoring (RPM) suddenly possible for virtually everyone. Anywhere. In November 2018 CMS officially approved three new billing codes for Remote Patient Monitoring (RPM). The telehealth industry experts agree that this is the biggest financial incentive to date in the history of digital medicine.”
Register for the webinar at https://attendee.gotowebinar.com/register/3642654945259750160
Registration is now open! Quality in Long-Term Care Conference-August 27th -28th, 2025 (Austin, Tx)
June 23rd, 2025
HHS, in collaboration with The University of Texas Steve Hicks School of Social Work, will host an informative two-day, free conference on quality in long-term care.
The 2025 Quality in Long-Term Care Conference (QLTCC) will be held at the Renaissance Austin Hotel, Aug. 27-28, 2025.
This year’s theme is “Blazing a Trail to Quality Improvement in Long-Term Care.”
The QLTCC offers presentations from nationally and internationally recognized experts. The topics include caring for people with dementia; infection prevention and control; current heath care trends; and cutting-edge advances in long-term care, aging, and disabilities. Continuing education credits will be available for multiple disciplines. Both in person and virtual options will be available.
The Quality Monitoring Team (QMP) is committed to providing high quality information and research from top-tier speakers to those working in the long-term care community. To provide quality programming of this caliber and that our attendees have become accustomed to, including the offering of a multitude of continuing education units, we have found it necessary to begin charging a fee. We thank you for your understanding and the continued support of this program.
The QLTCC offers presentations from nationally and internationally recognized experts. The topics include:
- Caring for people with dementia.
- Infection prevention and control.
- Current heath care trends.
- Cutting-edge advances in long-term care, aging, and disabilities.
Continuing education credits will be available for multiple disciplines. Both in person and virtual options will be available. Register for the conference here: 2025 Quality in Long-Care Conference
Email UT Steve Hicks School of Social Work for more information about this event
The conference is free to attend, and continuing education credit will be available for various healthcare disciplines.
Renaissance Austin Hotel
9721 Arboretum Blvd.
Austin, TX 78759
New ICF Provider Training Available: Internal Investigations by Providers for ICFs-July 18th, 2025
June 23rd, 2025
HHSC Joint Training is presenting a new webinar for Intermediate Care Facility (ICF) providers on the internal investigation process for ICFs.
This 1.5 hour webinar provides guidance for ICF providers on conducting a required internal investigation when notified of an incident.
The first presentation of this training will be held July 18, 2025.
Register for this training at HHS Provider Joint Training Opportunities.
Register for Long-Term Care Webinars for Nurses & Nursing Facility Administrators: June 25th, 2025
June 22nd, 2025
The Quality Monitoring Program and The University of Texas at Austin School of Nursing are offering a free webinar for nurses and nursing facility administrators.
“Diving into Enhanced Barrier Precautions for Nursing Facilities,” will be hosted by epidemiologist Annie Nutt on June 25 from noon to 1 p.m. Central time.
The webinar aims to guide and improve the care of Texas residents using evidence-based best practices.
Learning objectives will include:
• Understanding the science behind enhanced barrier precautions (EBP).
• Defining and distinguishing standard precautions, contact precautions and EBP.
• Discussing best implementation practices for EBP.
This webinar provides one continuing nurse education credit for registered nurses, certified nurse aides and licensed nursing facility administrators.
For more information, email Jacki Hecht at jhecht@nursing.utexas.edu.
To register for the webinar, click here.
TxHmL Amendment on Rates Effective Sept. 1, 2025
June 20th, 2025
HHSC Requests Comments on TxHmL Amendment Effective Sept. 1, 2025
HHSC is accepting comments on the amendment of the 1915(c) Texas Home Living Waiver. View the TxHmL amendment details.
Through this amendment, HHSC updated the attendant rates and increased the TxHmL individual cost limit from: $17,000 to 50 percent of the annualized cost of care in an Intermediate Care Facility for Individuals with an Intellectual Disability or Related Condition (ICF/IID) using the fiscal year 2026 non-state-operated small facility daily rate for Level of Need (LON) 1, rounded to the nearest dollar which is estimated to be $31,684 pending finalization of the fiscal year 2026 rates for ICFs/IIDs.
Comments will be accepted until July 21, 2025.
Email comments to the Texas Medicaid Waivers inbox.
CLASS Program Updates
June 20th, 2025
HHSC Requests Comments on CLASS Amendment Effective Sept. 1, 2025
HHSC is accepting comments on the amendment of the 1915(c) Community Living Assistance and Support Services Waiver. View the CLASS amendment details.
Through this amendment, HHSC updated the attendant rates and increased the CLASS individual cost limit from $114,736.07 to 210 percent of the annualized cost of care in an Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Condition (ICF/IID) using the unweighted average of the fiscal year 2026 non-state operated small facility daily rates for Level of Needs (LONs) 1, 5, and 8, rounded to the nearest dollar which is estimated to be $149,774 pending finalization of the fiscal year 2026 rates for ICFs/IID.
Comments will be accepted until July 21, 2025.
Email comments to the Texas Medicaid Waivers inbox.
March 20th, 2025
CLASS Form 3621 and Instructions Update
CLASS Form 3621, CLASS or CFC – Individual Plan of Care and Form 3621-T, CLASS/CFC – IPC Service Delivery Transfer Worksheet have been updated and are now available. The effective date for the forms and forms instructions is February 2025. Click here for the new forms.
March 16th, 2025
CLASS and DBMD Quarterly Webinar Recording Available
The March 19th Community Living Assistance and Support Services (CLASS) and Deaf Blind with Multiple Disabilities (DBMD) Quarterly Webinar with HHSC Long Term Services and Supports is available.
Listen to the webinar recording.
Read the CLASS and DBMD Quarterly Webinar (PDF).
October 8th, 2024
CLASS Program Manual Revised
The Community Living Assistance and Support Services (CLASS) Provider Manual revision 24-2 updates Section 2350 and Form 3595. The revision is effective Sept. 1, 2024.
Hurricane Season Training & Updating Emergency Preparedness Plans
June 1st, 2025
Hurricane Season – Ready or Not! Preparedness for HCS/TxHmL/ISS
Tuesday, June 17
10–11:30 am
Hurricane Season – Ready or Not! Preparedness for Intermediate Care Facilities
Friday, June 20
10–11:30 a.m.
Click on the following links for more training opportunities:
Individualized Skills and Socialization Training
May 18th, 2025

Planning For Flooding & Hurricane Season
** Please remember to address tornadoes in your emergency and evacuation planning, if they apply to your area, as they often occur during or in conjunction with Hurricane Season. Texas has already been hit by some severe storms, large hail, and tornadoes during the past few months. Don’t forget that May is heating up now and that severe storms and tornadoes can leave many people in Texas without electricity in incredibly hot temperatures.
See HHSC Recommendations Below:
“HHSC reminds long-term care facilities and agencies to review and update safety procedures and emergency plans for extreme weather in the 2024 hurricane season. Emergency plans for extreme weather should include the provider’s plan to address:
- Power loss.
- Water and food needs.
- Communication to families and staff.
- Staffing shortages.
- Sheltering in place and evacuation as applicable.
Providers must follow emergency preparedness rules and their own internal emergency preparedness policies and procedures.
Facilities with generators should perform any maintenance or needed testing. This will ensure the equipment functions in case of power loss.
It is important to review building integrity and identify any areas that may need repair, reinforcement or weatherproofing. Facilities in multi-story buildings should review any other needed measures as well. They should also have a plan in place for how to move residents around or out of the building if there is a loss of power or other identified need to move to a safer location.
Facilities should contact their local HHSC Regulatory Services regional office (RO) if they are impacted by an adverse event caused by severe weather — such as flooding, power loss, etc.
This communication is especially critical if a facility is projected to exceed its licensed capacity due to accepting residents that have been evacuated from another facility. All requests to exceed licensed capacity must be made through the RO and approved by the Deputy Associate Commissioner of Survey and Compliance.
Program rules require specific staff or a designee of each program to register with the emergency communication system and respond to requests through the emergency communication system. Please refer to PL 2025-01 (PDF) for instructions and more information regarding the emergency communication system requirements.
For training opportunities related to emergency preparedness for long-term care providers visit the HHSC Provider Training webpage.

BEHAVIORAL SUPPORT SERVICES PROVIDER POLICY TRAINING
 Behavioral Support Services
Behavioral Support Services
HCS and TxHmL Behavioral Support Services Provider Policy Training
(Has been mandated for HCS & TxHmL providers to ensure their contracted Behavioral Support Services providers to take since March 2015)
This course informs service providers of behavioral support services in the HCS and TxHmL programs related to the provision of behavioral support services in those programs. All new behavior support service providers must complete the WBT before providing services to an individual. All providers must complete the course every three years.
***To document successful course completion, participants must print a copy of the certificate provided at the end of the training and submit a copy to a program provider with whom they are employed or contracted.
Ensure Medicaid Continues To Support Individuals With IDD
May 31st, 2025
Please help ensure Medicaid continues to support Individuals in Texas with IDD. More than ever, we need everyone to focus their efforts on contacting our U.S. Senate representatives.
Call Senator John Cornyn (1-202-224-2934) and Senator Ted Cruz (1-202-224-5922) to continue to ensure we have Medicaid to support programs serving individuals with IDD, as well as directly support individuals with IDD in Texas.
The ARC of TEXAS has supplied a nice script for you, or your person with a disability to contact these senate representatives and share your concerns, issues, and need for Medicaid for services:
“Hi, my name is [NAME] and I live in [CITY]. I am a [Texan with a disability / family member of someone with an intellectual or developmental disability]. Medicaid is essential for [me/my family member] to live independently and access the services we need. Without Medicaid, [I/my family member] would not be able to receive critical support such as help with daily activities, therapies, job support, and community integration. Please do not cut funding for Medicaid. It allows [me/my family member] to live in the community, access education and employment opportunities, and fully participate in society. Thank you for your time, and please support Texans with disabilities like [me/my loved one].”
Bill Creating “Building Better Futures Program” Signed Into Law By Governor Abbott
May 30th, 2025
Governor Abbott signed House Bill 2081, officially creating the Building Better Futures program into law on May 26th, 2025.
This will be a step toward a more inclusive and accessible future for all Texans, including those with disabilities.
Rep. John Bucy III authored the bill, and it was sponsored by Senator José Menéndez. This law takes effect immediately and establishes a grant program within the Texas Higher Education Coordinating Board (THECB) to support colleges and universities in developing and expanding Comprehensive Transition and Postsecondary (CTP) programs across the state. CTP programs provide inclusive higher education opportunities for students with intellectual and developmental disabilities (IDD), and will ensure what is hopefully equitable access to postsecondary education and career pathways.
*As of now, only four CTP programs operate in the entire state.
Now that the bill has been signed into law, the THECB is charged with implementing the program and developing rules and policies necessary to administer this program effectively. We hope to keep you posted on developments as they occur.
Greater Inclusion of Children with Disabilities in Early Education Program-Major Bill Passes
May 26th, 2025
As of May 25th, 2025, the House and Senate have passed a bill that will create a plan for greater inclusion of children with disabilities in early education programs.
The Texas Senate gave final passage to House Bill 2310. The bill was authored by Rep. Claudia Ordaz and sponsored by Senator Tan Parker. It would require the TEA (Texas Education Agency), TWC (Texas Workforce Commission), and HHSC (Health and Human Services Commission) to develop a strategic plan to increase the inclusion of children with disabilities in public early childhood education programs.
It is now left up to Governor Abbott for consideration.
IDD Operations Portal Enhanced View Training: May 23rd & May 28th, 2025
May 22nd, 2025
IDD Operations Portal (IDD Ops Portal) Administrators will provide a brief overview of the new and enhanced view of the system.
Attendees are recommended to attend either session as they provide the same information.
Register for the May 23rd IDD Operations Portal
Enhanced View Training 11 a.m. to 12 p.m.
OR
Register for the May 28th IDD Operations Portal Enhanced View Training 2 p.m. to 3 p.m.
Topics include:
- Initial and single user account setup
- Navigation of new portal view
- Types of list views
The webinar will include a handout outlining the new IDD Ops Portal enhanced view. Attendees will receive a copy of the presentation before the webinar starts.
Email questions to idd_ops_portal@hhs.texas.gov.
HHSC has published Information Letter 2025-09 IDD Operations Portal (IDD Ops Portal) Transition to Enhanced View. This letter provides information on the overview of changes in the new enhanced view of IDD Ops Portal.
On Monday, June 2, 2025, the web address, appearance, and tab navigation for the IDD Ops Portal will change.
You may still navigate to the existing web address to log in, and you will be redirected to the new web address: https://ithhs.my.site.com/.
HCBS-Adult Mental Health Program: CBT Trainings
May 20th, 2025
Home and Community-Based Services – Adult Mental Health Program
CBT trainings
- Home & Community-Based Services – Adult Mental Health (contains provider training and resource information)
- Adult Mental Health Home & Community-based Services
Other information about the program:
Frequently Cited Deficiencies-HCS/TxHmL/ICF
May 20th, 2025
These are the most recent postings from HHSC, hopefully, those for 2024 will be posted soon,
Home and Community-based Services
- 10 Most Frequently Cited Deficiencies in Home and Community-based Services (HCS) & Texas Home Living (TxHmL) — Fiscal Year 2023 (July 16, 2024)
Texas Home Living
- 10 Most Frequently Cited Deficiencies in Home and Community-based Services (HCS) & Texas Home Living (TxHmL) — Fiscal Year 2023 (July 16, 2024)
Intermediate Care Facilities
Texas Parks & Wildlife Explore Webinar: New Initiatives Focusing on Accessibility & Inclusivity
May 18th, 2025
From HHSC Deat & Hard of Hearing Services:
“Join the Texas Health and Human Services Commission Deaf and Hard of Hearing Services for EXPLORE!, a webinar presented by the Texas Parks and Wildlife Department (TPWD) Accessibility Team. Discover the latest updates and initiatives across Texas public lands, focusing on accessibility and inclusivity. From camping in a state park to touring a fish hatchery or renewing your hunting license at a law enforcement office, TPWD is committed to outdoor access for all Texans and is making strides every day to increase accessibility to facilities, programs, and services.
Learn about the different programs offered by the agency, including boating education, learn-to-hunt programs, camping, and online education opportunities you can enjoy from home. TPWD staff will share resources for visitors with disabilities and demonstrate how to navigate the TPWD website to find the information you need to visit.”
When: Tuesday, May 27, 2025, 11:30 a.m. – 1:00 p.m.
Presented by: Cole Johnson, Accessibility Training Specialist, Texas Parks and Wildlife Department
To register, click here or scan the QR code below.
During this session, TPWD will highlight accessible facilities and outdoor spaces and discuss the role that accessibility plays in new parks and projects. Get information on adaptive equipment and all-terrain wheelchairs, making modification requests, and employment and volunteer opportunities that allow you to make a difference in our parks and beyond.
Make sure that you have everything you need to make an informed decision about visiting a TWPD facility and participating in a program.
This webinar will be presented in spoken English; CART (captioning) and ASL/English interpretation will be provided.
Certificates of Attendance will be awarded to attendees that may be used for continuing education documentation. In addition, participants may earn 0.15 DHHS CEUs (accepted by BEI).
Email questions to DHHS Training & Education.

Employment Readiness Updates
May 17th, 2025
New Employment Readiness Assessment Tool
On January 1, 2025, the Health and Human Services Commission (HHSC), implemented the new employment readiness benefit available to individuals enrolled in the Home and Community-based Services (HCS), Texas Home Living (TxHmL), or Deaf Blind with Multiple Disabilities (DBMD) waiver programs for individuals with intellectual or developmental disabilities. HHSC is required to assess all settings where employment readiness is provided for compliance with federal Home and Community-Based Services (HCBS) Settings requirements at 42 CFR 441.301(c)(4) before employment readiness can be provided in the setting.
All settings not previously assessed for compliance with the HCBS Settings Rule must conduct a self-assessment using the Employment Readiness Self-Assessment tool and submit it to Medicaid_HCBS@hhs.texas.gov for review and approval before providing employment readiness.
This tool is now available to providers at Employment Readiness Provider Self-Assessment Tool: HCBS Settings Rule Compliance. See Information Letters 2025-05 and 2025-01 for more details.
March 30th, 2025
Additional Information on HCBS Settings Rule Compliance for Employment Readiness Providers
HHSC has published Information Letter 2025-05 with additional information concerning Employment Readiness (ER). This letter provides information for financial management services agencies (FMSAs), local intellectual and developmental disability authorities (LIDDAs), and providers of Deaf Blind with Multiple Disabilities (DBMD), Home and Community-based Services (HCS) and Texas Home Living (TxHmL) services regarding the steps to ensure compliance with the HCBS settings rules for settings where employment readiness services are provided.
An on-site visit is required to beassessed for compliance with HCBS settings compliance rules, before providing ER services.
Current Individualized Skills and Socialization Providers In 2023, HHSC’s Contract Administration and Provider Monitoring (CAPM) staff conducted on-site visits to individualized skills and socialization provider settings to assess for compliance with HCBS Settings requirements (IL 2023-28). Providers previously assessed by CAPM staff for compliance with the HCBS Settings requirements do not need to be reassessed before the provider delivers employment readiness services in the same setting. Appropriate evidence of compliance is an email from HHSC confirming compliance. Providers who have been assessed but did not receive confirmation of compliance may reach out by email to Medicaid_HCBS@hhs.texas.gov using the subject heading: “Employment Readiness Request for Confirmation of Settings Compliance.”
If the provider of ER has not already had CAPM staff conduct an on-site visit, then they will have to complete a “self-assessment”, submit it, and then have an on-site visit to check for HCBS settings compliance.
First the ER provider must complete the self-assessment prior to the on-site visit and submit the self-assessment along with policies and other requested documents. The provider should conduct a self-assessment using the HHSC-developed assessment tool. The tool can be obtained by emailing Medicaid_HCBS@hhs.texas.gov using the subject heading “Request for Employment Readiness Self-Assessment.”
March 20th, 2025
Employment Readiness Q&A with Examples Document
HHSC has published the Employment Readiness Questions & Answers with Examples Document for Local Intellectual and Developmental Disability Authorities (LIDDAs), Deaf Blind with Multiple Disabilities (DBMD), Home and Community-based Services (HCS) and Texas Home Living (TxHmL) Programs. The document provides answers to questions about employment readiness and examples of scenarios that differentiate between employment readiness, individualized skills and socialization and employment assistance services.
January 14th, 2025
HHSC Publishes Information on Implementation of Employment Readiness
Note: The previous publication had a broken link. Please find the correct link below.
HHSC has published Information Letter 2025-01 Implementation of Employment Readiness. This letter provides a description of employment readiness and guidance related to the implementation of the new service.
***Don’t forget, the IPC form for TxHmL and HCS have been updated to include Employment Readiness Link to TxHmL form 8582 and Link to HCS form 3608 IPC
December 1st, 2024
New Service: Employment Readiness is available in the following waiver programs: HCS, TxHmL, and DBMB
As required by House Bill 4169 (88th Legislature, Regular Session, 2023), the Health and Human Services Commission (HHSC) is adding a new service similar to prevocational services to the Home and Community-based Services (HCS), Texas Home Living (TxHmL), and Deaf Blind with Multiple Disabilities (DBMD) waivers. The new service, employment readiness, will be available on Jan. 1, 2025.
Employment Readiness and Provider Fiscal Compliance Review Process Webinar
HHSC will host a webinar on Dec. 11 from 10 a.m. to noon for the Home and Community-based Services (HCS), Texas Home Living (TxHmL), and Deaf Blind with Multiple Disabilities (DBMD) program providers, local intellectual and developmental disability authorities, financial management service agencies and other interested parties.
The webinar will provide information on the new:
- Employment readiness service coming to the HCS, TxHmL and DBMD Programs on Jan. 1, 2025.
- Provider fiscal compliance review process in the HCS and TxHmL Programs, effective on Jan. 1, 2025.
Email questions about the webinar to your program policy:
What’s Employment Readiness?
Employment readiness provides assistance that prepares an individual for employment in the community. It helps an individual develop basic habilitative skills or achieve generalized vocational goals. Employment readiness activities cannot be directed at developing skills related to a specific type of employment.
Maintaining Records: Your Responsibility As A Provider
May 16th, 2025
In accordance with 26 TAC §52.113 (relating to Record Retention and Disposition) and the requirements of the Community Services Provider Contract or Provider Agreement, all records must be developed and retained in the form in which they were created until the latest of the following:
- seven (7) years after a claim is submitted;
- seven (7) years after all issues involving the record have been mitigated; or
- the individual about whom the record relates becomes 21 years of age.
If a contract is expiring or being terminated, the provider must adhere to 26 TAC §52.601 (relating to HHSC Review and Contractor Requirements Related to Expiring or Terminated Contract) and 26 TAC §52.113 (relating to Record Retention and Disposition) until the record retention period is satisfied.
Important: Providers are required to report the location of where the records will be stored and provide the name, address, phone number, and e-mail address of a person HHSC may contact to arrange access to the records. This information must be submitted to the assigned HHSC contract manager at the time of expiration, termination, when an update is necessary, or upon request.
IDD Conferences & Conventions 2025
May 15th, 2025

-
AAIDD Annual Meeting- The American Association on Intellectual and Developmental Disabilities (AAIDD) will hold its 149th annual meeting from June 23-25 inWashington D.C. This conference will focus on mentorship, access, equity, and collaboration in the IDD field.
- Texas State Chapter of AAIDD Convention- Takes place Sept. 29th-Oct. 2nd in Corpus Christi, Tx
-
CR Unite Autism and IDD Care Conference-Hosted by CentralReach, this conference for therapy providers, special educators, and supported employment agencies will be held October 20-22 inChicago, IL
-
One Voice Conference: Hosted by The American Academy of Developmental Medicine and Dentistry (AADMD) will host this conference June 5-8 inPhoenix, Arizona The theme is “Rising Phoenix: A New Era in IDD Health” and will cover topics like inclusive curriculum, intersectionality, brain & behavioral health, and clinical practice.
-
Pacific Rim International Conference on Disability and Diversity-Celebrating its 40th anniversary, this conference will be held April 15-16 inHonolulu, Hawaii
-
National Centre of Excellence in Intellectual Disability Health Conference- This conference will take place in Sydney, Australia and online, with the theme “Working together every step of the way”.
-
Global Disability Summit- Co-hosted by Germany, Jordan, and the International Disability Alliance (IDA), this summit took place April 2-3 in , Germany.
-
International Conference on Intellectual and Developmental Disabilities (ICIDD)- Organized by the World Academy of Science, Engineering and Technology, this conference will be held September 20-21 inLisbon, Portugal
.
-
DADD Conference- The Division on Autism and Developmental Disabilities (DADD) of the Council for Exceptional Children (CEC) will hold its 26th annual international conference January 22-24 inClearwater Beach, Florida
.
-
IASSIDD Congress- The International Association for the Scientific Study of Intellectual and Developmental Disabilities (IASSIDD) will host its congress inSingapore with the theme “Person-centricity as an approach to well-being of People with Intellectual and Developmental Disabilities”.
-
National Centre of Excellence in Intellectual Disability Health Conference- This conference will be held in Sydney, Australia and online.
- Aging and Developmental Disabilities Conference: The 34th annual conference will be held May 12-13 in St. Louis, MO
-
Developmental Disabilities Awareness Day Conference- This conference will take place on May 20 in Niagara Falls, NY.
-
Evidence for Success Disability Conference- This conference will be held June 22-24 in Chandler, Arizona
.
Interagency Reportable Conduct Search Engine: Informal Comments Deadline For Draft Rules
May 15th, 2025
Deadline for Informal Comments: May 30
Texas Health and Human Services Commission (HHSC) is accepting comments from stakeholders on the following draft rules related to an interagency reportable conduct search engine. The comment period ends May 30, 2025.
- Texas Administrative Code, Title 26,
- Chapter 550,
- Chapter 551,
- Chapter 553,
- Chapter 554,
- Chapter 555,
- Chapter 556,
- Chapter 557,
- Chapter 558,
- Chapter 559,
- Chapter 560,
- Chapter 565, (HCS) and
- Chapter 566 (TxHmL), concerning Long-Term Care Regulation (LTCR) Interagency Reportable Conduct Search Engine.
Questions and comments can be emailed to HHSC LTCR Rules.
Cost Report For 2024 & 2025 Accountability Report Training Information
May 6th, 2025
Additional Cost Report Training for HCS/TxHmL and ICF/IID or Related Conditions
The HHSC Provider Finance Department (PFD) has scheduled an additional 2024 Cost Report Training for Home and Community-based Services/Texas Home Living (HCS/TxHmL) and Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICF/IID) on Wednesday, May 7, 2025, at 9 a.m.
Register here for this training or visit the HHSC PFD Cost and Accountability Report Training webpage to register.
December 15th, 2024
HHSC has published the Information Letter (IL) 2024-XX regarding the 2024 Cost Report and 2024 or 2025 Accountability Report Training Information.
Information on Cost and Accountability Report Training Information can be accessed on the Provider Finance Department’s (PFD) webpage.
Review the IL for more information. If you have further questions, contact PFD-LTSS@hhs.texas.gov or (737) 867-7817.
HCS Handbook Revision 25-1
May 4th, 2025
The HCS Handbook Has Been Revised
The Home and Community-based Services (HCS), Handbook revision 25-1, updates Section 11000.
11000, Maintaining Medicaid Eligibility
Financial Eligibility Guidelines for Texas Home Living and Home and Community-based Services
This revision is effective April 29, 2025. Review the updates linked here.
November 26th, 2024
The HCS Handbook Has Been Revised
The Home and Community-based Services (HCS) Handbook revision 24-1 updates Appendix X.
This revision became effective Oct. 1, 2024. Click this link to see the updates.
Local Intellectual and Developmental Disability Authority Handbook (LIDDA) 24-4 Revision
May 3rd, 2025
The LIDDA Handbook Has Been Revised
The Local Intellectual and Developmental Disability Authority (LIDDA) Handbook, revision 25-3, updates form references.
This revision is effective May 1, 2025. Review the updates linked here.
February 26th, 2025
The LIDDA Handbook Has Been Revised
The Local Intellectual and Developmental Disability Authority Handbook (LIDDA) revision 25-2 updates sections 19220, 19230 and Form 8591.
This revision is effective Feb. 26, 2025.
Click this link to see the updates.
February 7th, 2025
The LIDDA Handbook Has Been Revised
The Local Intellectual and Developmental Disability Authority (LIDDA) Handbook revision 25-1 updates Sections 4000, 4100, 4200, 4300, 4400, 17000, 17100, 17200, 17300, 17400, 17500 and Resources.
This revision is effective Jan. 28, 2025.
Click this link to review the updates.
November 16th, 2024
The LIDDA Handbook Has Been Revised
The Local Intellectual and Developmental Disability Authority (LIDDA) Handbook revision 24-4 updates Appendix V.
This revision is effective Nov. 16, 2024. Click this link to see the updates.
October 7th, 2024
The LIDDA Handbook Has Been Revised
Local Intellectual and Developmental Disability Authority Handbook (LIDDA) 24-3 revision updates sections throughout the handbook.
The revision is effective Sept. 30, 2024. Click here for a full-size view of the updates.
| 12000 | Protocol for Offering an HCS Crisis Diversion Slot | Updates language for clarity. |
| 12100 | Purpose | Updates reference to Section 12300.
Updates language for clarity. |
| 12300 | Qualifications for the HCS Reserved Capacity Group for Crisis Diversion | Changes title to Criteria for Requesting an HCS Reserved Capacity Group Crisis Diversion Slot.
Changes language in first paragraph about how a person meets the criteria for the LIDDA to request an HCS Reserved Capacity Group Crisis Diversion slot. Removes language in fourth bullet about ICF/IID LOC I criteria, replaces it with how a person meets the criteria for LIDDA priority population per Title 26 Texas Administrative Code (TAC), Section 304.102, Diagnostic Assessment. Updates the Note to require persons to meet the diagnostic and financial criteria specified in 26 TAC Section 263.101, Eligibility Criteria for HCS Program Services and CFC Services to enroll in HCS. Updates language for clarity. |
| 12400 | Process | Removes language about ICF/IID LOC I criteria and adds language that requires a person to meet the criteria for LIDDA priority population per 26 TAC Section 304.102, Diagnostic Assessment.
Adds information about Form 1058 and submission. Removes requirements to submit a packet with a Determination of Intellectual Disability (DID) and Inventory for Client and Agency Planning (ICAP) booklet/scoring sheet. Updates HCS Program TAC reference to 26 TAC Section 263.104. Updates language for clarity. |
“Caytlin Handley Act”-House Bill 1188
April 25th, 2025
“Caytlin Handley Act”
On April 8, the House Committee on Public Education heard House Bill 1188, filed by Rep. Christian Manuel.
This bill would require school districts to provide families of students identified as eligible to receive special education services due to a diagnosis of IDD or developmental delay to their (LIDDA), ensuring students and families are informed about Medicaid waiver programs, long-term services and supports, and other community resources.
From the ARC of Texas Legislative Newsletter April 18th, 2025 Edition
“The Handley Family of Katy, Texas—Caytlin, Carey, and Boyd—have championed this bill from the start, using their voices and lived experience to lead the charge for better access to information and services for families of students with disabilities. In recognition of Caytlin’s advocacy, Rep. Harold Dutton Jr. motioned to rename the bill the “Caytlin Handley Act,” and in a rare and powerful moment, the committee voted to advance the bill immediately following testimony from the Handley family and supporters, including The Arc of Texas.”
WATCH the testimony (see timestamps of interest below).
- Rep. Manuel lays the bill out: 15:23
- The Handley Family testifies: 19:46
- Carey testifies: 20:27
- Caytlin testifies: 22:13 and 25:37
- Boyd testifies: 22:52
- Motion by Rep. Dutton: 46:23
Provider Job Openings & Employment Opportunities: HCS/ICF/ISS

Job Position
Lone Star HCS (Conroe, Tx)

Job Position: Host Home/Companion Care Service Provider
Please see information below and contacts to respond.
Looking for Host Home/Companion Care provider who wants to care for 3 young men, 2 of which are fairly independent. The 3rd individual needs a bit more help with hygiene and meal preparation. The host home is located in the Woodlands, Texas area near Conroe and Houston. If you are interested in the position, please contact Rhonda Wilson for more details.
Note: You would not be using your own home. The home would be provided by one of the individual’s family members, for the host home/companion care provider to rent along with the individuals they are caring for.
Rhonda Wilson (Program Director/Provider Coordinator)
936-777-2028 (Phone) 936-228-7641 (Fax)
March 1st, 2025
The Harris Center for Mental Health and IDD
Job Position Now Available: Program Director V, Residential & Day Services.
Please see information about the position below. We have also provided a link you may click on to apply.
**Note, this position is on page 2.
The Harris Center is now accepting candidates and will begin scheduling interviews this week. If you know any interested parties, please feel free to share.
I believe this position will be with their internal ICF/IID program
Based on the many phone calls, emails, and contacts through our social media pages concerning employment needs and job openings in the HCS/ICF/ISS programs, we will continue to use our “Updates” page as a platform to assist providers in posting these openings and opportunities.
If you contact Meghan Jones at meghanjones.tx@gmail.com and let her know where you are posting a position and who to contact, we can also just put a link and the contact person’s name, # and/or email for free at no cost. For example, you are posting on Indeed, Linkedin, BenefitMall, Facebook, PACSTX job postings, an online newspaper, etc… If you would like to post an opening with a complete job description (or longer than a few paragraphs), the cost is $15 for a one-time fee. We will continue to run this post until you notify us otherwise. All current updates are also noted in our bi-weekly newsletter.
We will also continue to repost openings when we can on our Linkedin page as well as our Facebook and Instagram pages for Twogether Consulting.
There is no charge, we just ask you all to keep referring us to others who don’t know about us for their IDD program needs and of course, we hope you will continue to use our services to assist you with your training needs, on-site and off-site assistance.
Julie Blacklock/ Owner
CFC Proposed Billing Requirements (HCS/TxHmL)-Drafts
April 15th, 2025
The proposed billing requirement revisions and a summary of changes are located on the Long-term Care Providers webpage and are outlined below:
HCS
Texas Council on Developmental Disabilities News This Week
April 15th, 2025
From our friends at Texas Council on Developmental Disabilities:
IDD Coordinating Council
TCDD Senior Public Policy Analyst Lauren Gerken provided verbal testimony on March 25 to the House Human Services Committee on House Bill (HB) 2807, which would establish a statewide intellectual and developmental disability (IDD) coordinating council. She discussed how this new council would bring multiple agencies together to develop strategies on optimizing the complex system of Medicaid waivers, education, and more. The council would also ensure implementation and proper oversight of a five-year statewide IDD strategic plan. Gerken detailed how this new council would differ from other state disability entities (PDF) such as TCDD and the Texas Governor’s Committee on People with Disabilities. HB 2807 was featured as a TCDD Bill of the Week.
Soft-Skills Training
Gerken also gave verbal testimony on March 25 to the House Subcommittee on Workforce on HB 1147, which would require the Texas Workforce Commission to establish a workplace soft-skills training pilot program. Gerken said that, while the bill is not specifically related to disability, it could allow people with disabilities to gain a certificate for soft skills that they were unable to qualify for previously. The bill would also give people with disabilities an opportunity to engage in the workforce in a more meaningful way to increase their employability.
Resources to Contact Lawmakers and Give Testimony
The House Research Organization recently published its list of legislative staff (PDF, 28 pages, 3.9 MB) for the 89th Legislature. The document provides the names and titles of staff in lawmaker and committee offices, both for the House and the Senate. It is a helpful tool for making initial contact with staff, or for following up after you’ve spoken with an office.
If you’d like to give remarks at an upcoming hearing but aren’t sure how to craft your comments, we’ve created a My Testimony Blueprint (PDF) that can be used as a guide. For more legislative advocacy resources, visit our website.
HB 1936 would strengthen the enforcement of accessible parking violations. It was authored by Rep. David Cook.
**For More information from TCDD or to subscribe to their newsletter please click on this link: TCDD
Updates on Budget Proposals For IDD Services
April 10th, 2025
Resource Links:
Consideration of the budget as well as HB 500, the supplemental budget, by the House will occur today at 9:00am, Thursday, April 10th.
HB 500 (supplemental): https://www.capitol.state.tx.us/tlodocs/89R/billtext/pdf/HB00500H.pdf#navpanes=0
House Rules Adopted related to Consideration of the Budget: To view the rules adopted by the House on April 2, 2025 related to consideration of the budget (SB 1), see pages 2 – 4 at the following link:
https://journals.house.texas.gov/hjrnl/89r/pdf/89RDAY37FINAL.PDF#page=2
Link to Watch Today’s Debate: Though the House proceedings on the budget and HB 500 will make for a long day, interested persons may view at: https://house.texas.gov/videos
Representative Donna Howard’s Proposed Accountability Amendment to Rider 23:
This amendment adds the provision below to Rider 23 which parallels the same provision in the Senate Rider. However, unlike the Senate Rider 23 which requires HHSC to create list of providers whose calculated direct care staff wage and benefits expense ratio is less than 0.95 and submit to certain legislative offices, Howard’s amendment sets it at less than 0.90.
(c) Out of funds appropriated in Strategy B.1.1, Medicaid & CHIP Contracts and Administration, HHSC shall continue to collect biennial cost reports from providers to monitor the average hourly wage and associated payroll costs, taxes, and benefits.
HHSC shall calculate for each provider the total amount that was paid to the provider that is attributable to the direct care wages, payroll costs, taxes, and benefits, the amount expended by the provider for that purpose, and the ratio of expenses to revenue to determine a direct care wage and benefits expense ratio. HHSC shall report to the Legislative Budget Board, the Lieutenant Governor, the Speaker of the House of Representatives, and the Office of the Governor on an annual basis by November 1 of each year on the findings, including a list of providers whose calculated direct care staff wage and benefits expense ratio is less than 0.90.
Gofundme Fundraiser Link For Our Friend Marie “Lynn” Palmares
March 31st, 2025

Many of you may know our friend and colleague Marie “Lynn” Palmares. Lynn has worked in ICF and HCS programs in the Dallas/Ft. Worth area for many years. In the past 8 years or so she has been working with the YES waiver program. Lynn has helped many providers as an independent contractor and as a consultant for Twogether Consulting over the past 10 years with their HCS and YES waiver programs. In addition, Lynn has assisted our clients at Twogether Consulting with their HCS-Adult Mental Health and YES waiver applications.
Lynn has been very ill over the past year and was recently diagnosed with stomach cancer. She really needs some help with her bills for treatment and medications. Even with insurance, out-of-pocket expenses for treatments and medication are very high. The medication she needs the most now costs thousands per month. I have posted her daughter’s “gofundme” page she set up for Lynn, if anyone would like to help.
Previous Temporary Exception Now A Permanent Policy Change in HCS/TxHmL For Respite and CFC PAS/HAB
March 30th, 2025
Permanent Policy Change for CFC PAS/HAB- Letter 2025-04
HHSC has published Information Letter 2025-04 Permanent Change to HCS and TxHmL Policy for Community First Choice (CFC) personal assistance services (PAS)/habilitation (HAB) service providers. This letter informs financial management services agencies (FMSAs), local intellectual and developmental disability authorities (LIDDAs), and providers of Home and Community-based Services (HCS) and Texas Home Living (TxHmL) services that the temporary policy allowing the service providers of CFC PAS/HAB to live in the same home as the person receiving CFC PAS/HAB services is now permanent.
March 15th, 2025
Permanent Policy Change for CFC PAS/HAB
In March 2020, HHSC started a temporary policy change for respite and Community First Choice (CFC) Personal Assistance Services (PAS)/Habilitation (HAB) provided in the Home and Community-based Services (HCS) and Texas Home Living (TxHmL) waiver programs.
This change allowed service providers of respite and CFC PAS/HAB to live in the same home as the person receiving these services. A person’s spouse, or parent if the person is under 18, was not allowed to be a paid service provider of these services in accordance with the HCS, TxHmL and CFC Billing Requirements.
This temporary policy change that was extended and effective through March 31st, 2025, has now been made a permanent policy change, effective April 1st, 2025!
Program providers must complete the required background checks for all service providers, including respite and CFC PAS/HAB providers living in the same home as the individual receiving services. Requirements can be found in the following references:
- The Texas Administrative Code (TAC), Title 26, Part 1, Chapter 263, and Chapter 262.
- HCS and TxHmL Rules, 26 TAC §565.9(b) and §566.9(r) and (s).
- The HCS Program Billing Requirements and the TxHmL Program Billing Requirements, Section 3400 for service provider qualifications, and the CFC Billing Requirements for HCS and TxHmL Program Providers.
If you have any additional questions, please feel free to reach out to LTCR Policy at: LTCRPolicy@hhs.texas.gov.
Exception Ending August 31st, 2023
REMINDER: COVID-19 Update to Temporary Change to HCS and TxHmL Policy for Respite, CFC PAS/HAB Service Provider
In March 2020, HHSC implemented a temporary policy change for respite and Community First Choice Personal Assistance Services/Habilitation provided in the Home and Community-based Services and Texas Home Living waiver programs. This change allows service providers of respite and CFC PAS/HAB to live in the same home as the person receiving these services.
This change has given greater access to needed services for people living in their own home or family’s home. A person’s spouse or the person’s parent, if the person is under 18, is not allowed to be a paid service provider of these services in accordance with the HCS, TxHmL and CFC Billing Requirements.
This temporary policy change is effective March 27, 2020, through Aug. 31, 2023. HHSC will provide guidance if anything changes.
Program providers must complete the required background checks for all service providers. They must follow:
- The Texas Administrative Code, Title 26, Part 1, Chapter 263 and Chapter 262.
- HCS and TxHmL Rules, Section 9.177 (n) and (o), and Section 9.579 (r) and (s).
- The HCS Program Billing Requirements and the TxHmL Program Billing Requirements Section 3400 for service provider qualifications and the CFC Billing Requirements for HCS and TxHmL Program Providers.
Overview Presentation of Specialized Telecommunications Assistance Program (STAP) For Deaf and Hard of Hearing
March 14th, 2025
![]()
Deaf and Hard of Hearing Services From HHSC Presents
Overview of the Specialized Telecommunications Assistance Program (STAP)
Wednesday, March 26, 2025
11:00 a.m. – 12:30 p.m., CST
Join Aaron Mowell, STAP manager, for an overview of the Specialized Telecommunications Assistance Program (STAP). The purpose of STAP is to allow people with disabilities to access the telephone network, enabling them to call family and friends, make doctor’s appointments, and reach emergency services. This informative session will explain the program requirements and application process and provide an opportunity for you to ask questions.
This webinar will be presented in American Sign Language (ASL) and spoken English; CART (captioning) and ASL/English interpretation will be provided.
Certificates of Attendance will be awarded to attendees that may be used for continuing education documentation. In addition, participants may earn 0.15 DHHS General CEUs (accepted by BEI).
Click on link below to register and for more information:
Registration Link & Details
HCS/TxHmL Providers & FMSAs: Technical Assistance Session For TMHP on April 2025
March 15th, 2025
Medicaid and CHIP Services (MCS) will be hosting monthly sessions for Program Providers and Financial Management Services Agencies (FMSAs), who use the Long-term Care (LTC) online portal for the Home and Community-based Services (HCS) and Texas Home Living (TxHmL) waiver programs.
- TMHP and HHSC staff will be available to troubleshoot and potentially resolve issues with forms and claim submissions in the LTC online portal.
- All attendees should be prepared to discuss and show, if needed, the issues they encounter when attempting to submit forms or claims in the LTC online portal.
Save the Date
The technical assistance session will be held on:
- Thursday, April 24, from 10am-11:30am
Documentary “Into the Spotlight” Released To The General Public
February 27th, 2025

Utilization Review Department News!
February 20th, 2025
HHSC Publishes Information on Waiver and Community Services Utilization Review Process
HHSC has published Information Letter 2025-02 Waiver and Community Services Utilization Review Process.
This letter provides a summary of the authority for conducting field utilization reviews in the Community Living Assistance and Support Services (CLASS), Deaf Blind with Multiple Disabilities (DBMD), Home and Community-based Services (HCS) and Texas Home Living (TxHmL) Programs.
There is also a link included in the letter, to the document that describes the Waiver and Community Services Utilization Review Process.
You can also click on the link to the summary of this field UR Review process here: https://www.hhs.texas.gov/sites/default/files/documents/field-ur.pdf
Employment Readiness Rates
February 18th, 2025
HHSC Publishes Payment Rates for Employment Readiness Services in DBMD, HCS, and TxHML Waiver Programs.
HHSC approved payment rates for for Employment Readiness Services in the Deaf-Blind with Multiple Disabilities (DBMD), Home and Community-Based Services
(HCS), and Texas Home Living (TxHmL) Waiver Programs effective Jan. 1, 2025.
More information about the approved payment rates is available on the HHSC Provider Finance Department webpage.
The Employment Readiness Services payment rates, effective Jan. 1, 2025, can be accessed on the HHSC Provider Finance Department webpage.
See Jan 2025 HCS & TxHmL rates here including Employment Readiness rates for HCS: HCS Rates-Jan-2025
For TxHmL: TxHmL Rates-Jan-2025
Letter To The Providers From Twogether Consulting: February 15th, 2025
February 15th, 2025

From Twogether Consulting!
Hello Everyone!
Hope everyone had a wonderful Valentine’s weekend. I feel like this month is flying by. Don’t forget we have a “Pop-Up”webinar on Feb. 21st,2025 from 1pm-3:30pm. This is especially great session for any new providers, as well as new program managers and case managers:“Care Coordination Basics: Admission, Post- Admission & Other Follow-Up Required” (HCS)
Twogether Consulting will be adding additional ICF and HCS webinars for March on the website later this week. Don’t forget we have a live 2-day training in Austin at the PPAT Office (Private Provider’s Association of Texas) for HCS Care Coordination (Case Management) on February 27th & 28th, 2025. Seating is limited, so please contact Megan Jones as soon as possible if you want to sign up. We will also be adding some live training sessions for Nurses in HCS/TxHmL programs in March in the Austin area. Look for the sessions to be posted in the near future on our home page calendars-www.twogetherconsulting.com.
If you missed the webinar for ICAP’s/IDRC’s/LON’s (ICF Program), please let us know. We do have the recorded session. We do have a variety of other pre-recorded trainings for program managers, case managers and nurses, so feel free to email us at info@twogetherconsulting.com to inquire. Let us know what areas of training you would like, to help us plan future sessions.
Please see our “Updates” section of the website for the latest news for IDD providers.

Medical Care Advisory Committee (MCAC) met Thursday, February 13, 2025
February 15th, 2025
Spotlight Musical Theater Presentation in Dallas February 22nd, 2025
February 14th, 2025
Belong Disability Ministry celebrates 15 years of Spotlight Musical Theater with a new production, “I’m on My Way” on Saturday, February 22 from 5:00 – 7:00pm at Highland Park United Methodist Church. This comedic, yet touching musical shares captivating stories of what it’s like to live with a disability through a series of DART rides. Join us in a theatrical display that features real-world scenarios, upbeat original music, and a journey in finding courage during the tough times of life. Purchase tickets HERE. For more about Spotlight Theater, please click on this Youtube link, for a newscast story about their documentary: https://www.youtube.com/watch?v=tf4lAoBuhNY
5-Year Children’s Behavioral Health Strategic Plan
February 8th, 2025
The Texas Health and Human Services Commission (HHSC) has published the 2024 Children’s Behavioral Health Strategic Plan (PDF).
The five-year plan is intended to foster an environment in which Texas children and their caregivers, based on identified need, have access to compassionate, comprehensive, and innovative behavioral health care, that will help develop their resilience and enable them to thrive emotionally, mentally, and socially.
The plan was developed by the Texas Statewide Behavioral Health Coordinating Council’s Children’s Behavioral Health Strategic Plan Subcommittee and is specific to the behavioral health of children and youth.
If you have any questions or comments, please email mentalhealth_sbhcc@hhs.texas.gov.
HHSC Publishes PL 2025-01: New Emergency Communication Tool For Long-Term Care Providers-AlertMedia
January 19th, 2025
![]()
New Emergency Communication Tool – AlertMedia.
HHSC Publishes PL 2025-01 New Emergency Communication Tool – AlertMedia. This provider letter informs providers of the emergency communication system called AlertMedia, how it will be used, and their responsibility in signing up for the system.
HHSC will use this system to send emergency and outreach notifications through email, text, voice calls, and app push if available.
All ALF’s, DAHS’s, HCSS’s, ICF’s, NF’s and HCS Providers must complete the following steps:
• Register your AlertMedia account by following the steps provided in the Self Registration Guide.
Registration process:
Users will enter their contact information, provider choices, and set a password. Users will be sent an activation pin to enter. Once the user selects Submit, registration is complete.
Registration Page: https://texashhsc.alertmedia.com/public/v2?
• HHS will send a test alert. Please save that number to your phone to ensure receipt of future communication.
• Download the optional AlertMedia mobile app for iPhone or for Android to ensure the receipt of emergency-related messages.
Providers will receive a confirmation code to their email address after registration and should refer to the Self-Registration Guide for any questions regarding registration or troubleshooting.
*Note: PL-2025-01 contains the AlertMedia Self Registration Guide – Attachment A
Contact Information
Please reach out to RSDAlertMedia@partner.hhs.texas.gov with any questions.
November 10th, 2024
REMINDER TO ALL LONG-TERM CARE PROVIDERS, BLACKBOARD CONNECT ENDED OCT. 31ST, 2024!
The current emergency communication system (Connect) for long-term care providers ended on Oct. 31 and will be replaced by the new system (AlertMedia), which is anticipated to go live no later than Dec. 1.
During this gap, no emergency communication system will be in place, so HHSC will communicate with providers through alerts, email and phone calls. Providers must respond to any request for information related to emergency preparedness and follow any instructions from HHSC.
Once AlertMedia is in place, HHSC will issue a separate communication on how to use the new system. Providers will be required to register in AlertMedia as defined by their Texas Administrative Code rule.